RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCE, BANGALORE KARNATAKA ,
PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION
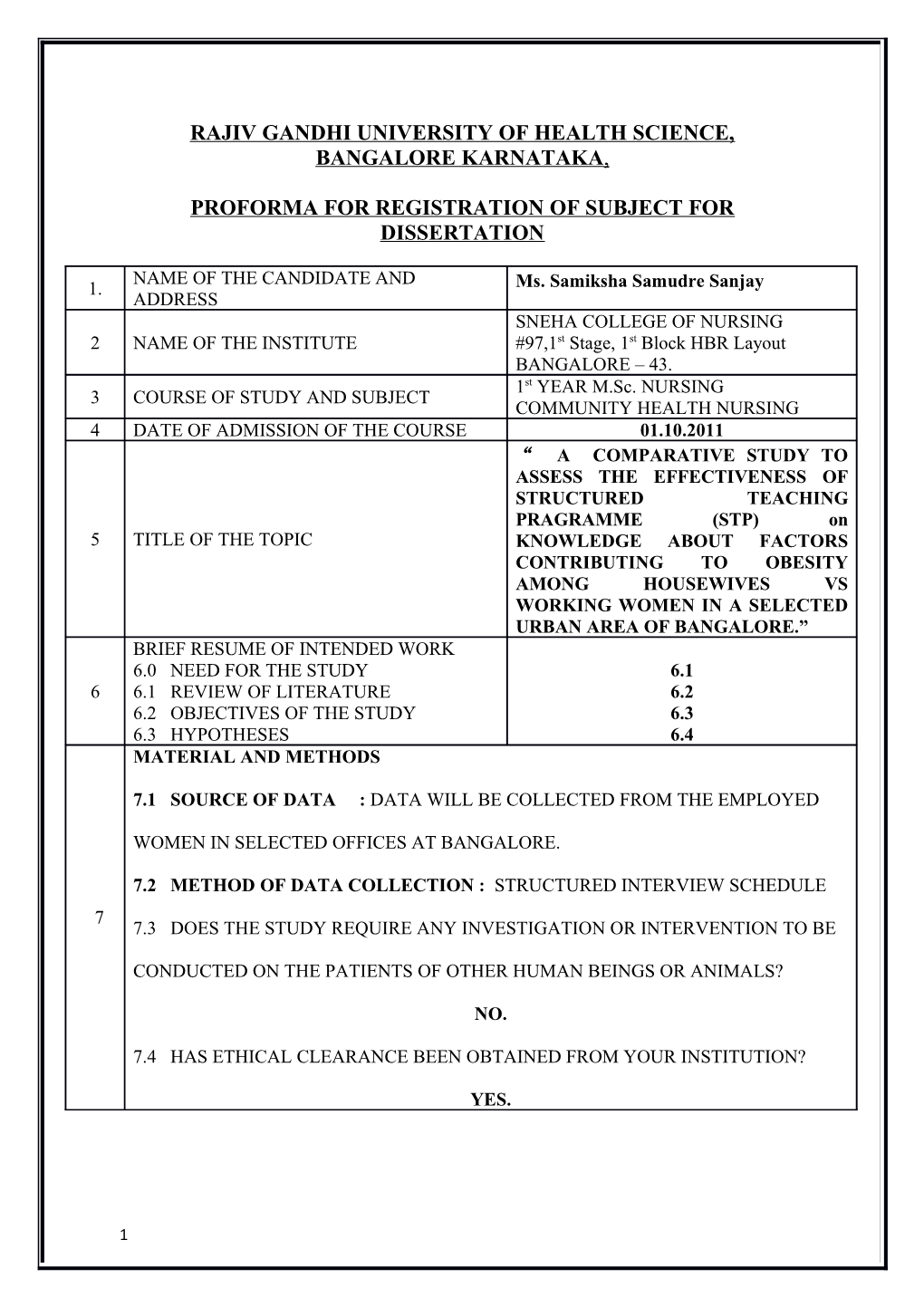
NAME OF THE CANDIDATE AND 1. Ms. Samiksha Samudre Sanjay ADDRESS SNEHA COLLEGE OF NURSING 2 NAME OF THE INSTITUTE #97,1st Stage, 1st Block HBR Layout BANGALORE – 43. 1st YEAR M.Sc. NURSING 3 COURSE OF STUDY AND SUBJECT COMMUNITY HEALTH NURSING 4 DATE OF ADMISSION OF THE COURSE 01.10.2011 “ A COMPARATIVE STUDY TO ASSESS THE EFFECTIVENESS OF STRUCTURED TEACHING PRAGRAMME (STP) on 5 TITLE OF THE TOPIC KNOWLEDGE ABOUT FACTORS CONTRIBUTING TO OBESITY AMONG HOUSEWIVES VS WORKING WOMEN IN A SELECTED URBAN AREA OF BANGALORE.” BRIEF RESUME OF INTENDED WORK 6.0 NEED FOR THE STUDY 6.1 6 6.1 REVIEW OF LITERATURE 6.2 6.2 OBJECTIVES OF THE STUDY 6.3 6.3 HYPOTHESES 6.4 MATERIAL AND METHODS
7.1 SOURCE OF DATA : DATA WILL BE COLLECTED FROM THE EMPLOYED
WOMEN IN SELECTED OFFICES AT BANGALORE.
7.2 METHOD OF DATA COLLECTION : STRUCTURED INTERVIEW SCHEDULE 7 7.3 DOES THE STUDY REQUIRE ANY INVESTIGATION OR INTERVENTION TO BE
CONDUCTED ON THE PATIENTS OF OTHER HUMAN BEINGS OR ANIMALS?
NO.
7.4 HAS ETHICAL CLEARANCE BEEN OBTAINED FROM YOUR INSTITUTION?
YES.
1 6.0 INTRODUCTION:
The foods we eat every day contribute to our well-being. Foods provide us with the nutrients we need for healthy bodies and the calories we need for energy. If we take in more calories than we burn, the extra food turns to fat and is stored in our bodies. If we overeat regularly, we gain weight, and if we continue to gain weight, we may become
obese.1
Obesity is a medical condition in which excess body fat has accumulated to the extent that it may have an adverse effect on health, leading to reduced life expectancy and/or increased health problems. Body Mass Index (BMI), a measurement which compares weight and height, defines people as overweight (pre-obese) if their BMI is between 25 and 30 kg/m2, and obese when it is greater than 30 kg/m2.2 Obesity now considered as a "Killer lifestyle" disease is an important cause of preventable death worldwide.3
According to the World Health Organization (WHO), 1.2 billion people worldwide are officially classified as overweight. This is probably the most sedentary generation of people in the history of the world.4 In the Indian scenario, even with the growing awareness about health and fitness, more than 3 percent (3 cores) of the Indian population is obese.
There is an urgent need to create public awareness about the mechanisms of identification, prevention and treatment of severe obesity than ever before.5
Worldwide, anti-smoking campaigns' success can only be attributed to persistent and repeated public awareness programs over several decades. Since 1964 when anti- smoking campaign first started-nearly half of living adults who smoked have stopped in the
2 USA.
Obesity Foundation India plans to emulate the core principles of anti smoking campaign to achieve its goal of prevention of severe obesity.6
There is strong evidence that the prevalence of obesity is high in American Indian adults. A national survey of American Indians living in communities served by the Indian
Health Service was conducted as part of the 1987 National Medical Expenditure Survey.
The prevalence of overweight [body mass index (BMI; in kg/m2) > 85th percentile of
NHANES II reference population ] self-reported by American Indian adults in this survey was 34% for men and 40% for women, higher than the US rates of 24% and 25%, respectively . For both men and women the prevalence varied by age, with the highest prevalence occurring between 35 and 64 y of age. The most extensive tribe-specific estimates of obesity in adults are in Pima Indians. Adult Pima Indians have a far greater prevalence of obesity than the US population. The age-specific prevalence of overweight ranged from 61% to 78% in 20–64-y-old men and from 81% to 87% in women of the same age. 7
The Strong Heart Study gathered data on men and women aged 45–74 y in 13
American Indian tribes in Arizona, Oklahoma, and the Dakotas. The prevalence's of overweight (defined as BMI >27.8 for men and >27.3 for women) in Arizona, Oklahoma, and the Dakotas were 67%, 65% and 54%, respectively, for men, and were substantially higher at 80%, 71%, and 66%, respectively, for women.8 These are considerably higher than the NHANES III all-races rate of 27% and 28% overweight for same-age men and women, respectively . Recent findings from the Navajo Health and Nutrition Survey
(NHNS) indicated that one-third of men aged 20–39 y and one-half of men aged 40–59 y,
3 but <10% of men aged ≥60 were overweight. Two-thirds more women in all age groups were overweight.9
6.1 NEED OF THE STUDY:
The epidemic of obesity in American Indian communities and the need for childhood obesity-prevention programs. Obesity increases the likelihood of various diseases, particularly heart disease, type 2 diabetes, obstructive sleep apnea, certain types of cancer, and osteoarthritis. 10 Obesity is most commonly caused by a combination of excessive food energy intake, lack of physical activity, and genetic susceptibility, although a few cases are caused primarily by genes, endocrine disorders, medications or psychiatric illness. Evidence to support the view that some obese people eat little yet gain weight due to a slow metabolism is limited; on average obese people have a greater energy expenditure than their thin counterparts due to the energy required to maintain an increased body mass.11
Obesity Silent Killer in India a new study released by the Registrar General of India indicates that obesity-related diseases have joined malnutrition as leading causes of death.
As India's economy grows, so does the temptation for many people to eat more and do less.
Tired and home late? Fatty food is just a phone call away. In a country where the Global
Hunger Index shows that nearly half of all children are malnourished, many of India's well- off citizens are now seeking treatment for obesity. New Delhi-based business professional
Aradhna Tripathi admits she loves to eat. "Eating is the most important thing in any Indian
4 household and how you show your love and gratitude for a person is through the kind of food you serve him," she said. "Indian people are used to eating the kinds of foods cooked at home that are filled with masala and oil. With the kind of sedentary lifestyle we lead, these are the reasons we have obesity increasing. "
India's current National Family Health Survey indicates that more than 20 percent of urban Indians are overweight or obese. And in the north-western state of Punjab, nearly
40 percent of all women are overweight or obese.12 Tripathi says she was inspired to lose weight after contracting gestational diabetes during her recent pregnancy. Her mother and grandmother are both diabetic.13
More and more Indians are signing up for weight loss programs out of fear of disease, says Vandana Luthra, managing director of VLCC, a global slimming agency based in India. "Earlier it was more of a luxury going to a spa or wellness centre, but today it has become a necessity," she said.14
New data released by the International Diabetes Federation shows every sixth diabetic in the world is an Indian - earning India the title "the world's diabetes capital."
Research over the past decade shows that genetically, Indians store more body fat per kilogram than Europeans. Leading health professionals agree, obesity puts Indians at an even greater risk of getting diabetes. This risk is now crossing socioeconomic lines, says
Dr. Anoop Misra director of diabetes and metabolic disease at New Delhi's Fortis Hospital.
15
A Mid Day survey and research study revealed India's obese population goes up by
70 million .Dieting and physical exercise are the mainstays of treatment for obesity. Diet quality can be improved by reducing the consumption of energy-dense foods such as those high in fat and sugars, and by increasing the intake of dietary fiber. Anti-obesity drugs may be taken to reduce appetite or inhibit fat absorption together with a suitable diet. If diet,
5 exercise and medication are not effective, a gastric balloon may assist with weight loss, or surgery may be performed to reduce stomach volume and/or bowel length, leading to earlier satiation and reduced ability to absorb nutrients from food.16
Many people were thin and undernourished. The other side was many were fat and some of these belonged to the poorest section of this slum. This was a clear contrast, a paradox occurring in the same community. Half people over nourished, half undernourished," he said. He blames the rise in obesity on inexpensive and oily snacks popular in Indian slums, and a lack of preventative education. China is not too far behind
India. The World Health Organization says China's obesity rates hover at 5 percent and almost 20 percent in select cities. But Dr. Misra says China is better equipped to contain the epidemic because it can employ uniform prevention efforts in schools.17
India has a more heterogeneous mix of government and private schools. Obesity is a leading preventable cause of death worldwide, with increasing prevalence in adults and children, and authorities view it as one of the most serious public health problems of the
21st century. Obesity is stigmatized in much of the modern world (particularly in the western world), though it was widely perceived as a symbol of wealth and fertility at other times in history, and still is in some parts of the world. Excessive body weight is associated with various diseases, particularly cardiovascular diseases, diabetes mellitus type 2, obstructive sleep apnea, certain types of cancer, and osteoarthritis. As a result, obesity has been found to reduce life expectancy.18
A study undertaken in America and Europe reveals that Obesity is one of the leading preventable causes of death worldwide. Large-scale American and European studies have found that mortality risk is lowest at a BMI of 20–25 kg/m2 in non-smokers and at 24–27 kg/m2 in current smokers, with risk increasing along with changes in either
6 direction. A BMI above 32 has been associated with a doubled mortality rate among women over a 16-year period. In the united states obesity is estimated to cause an excess
111,909 to 365,000 deaths per year, while 1 million (7.7%) of deaths in the European are attributed to excess weight. On average, obesity reduces life expectancy by six to seven years: a BMI of 30–35 reduces life expectancy by two to four years, while severe obesity (BMI > 40) reduces life expectancy by 10 years. Obesity increases the risk of many physical and mental conditions. These co morbidities are most commonly shown in metabolic syndrome, a combination of medical disorders which includes: diabetes mellitus type 2, high blood pressure, high blood cholesterol, and high triglyceride levels.
Complications are either directly caused by obesity or indirectly related through mechanisms sharing a common cause such as a poor diet or a sedentary lifestyle. The strength of the link between obesity and specific conditions varies.19
One of the strongest is the link with type 2 diabetes. Excess body fat underlies 64% of cases of diabetes in men and 77% of cases in women. Health consequences fall into two broad categories: those attributable to the effects of increased fat mass (such as osteoarthritis, obstructive sleep apnea, and social stigmatization) and those due to the increased number of fat cells (diabetes, cancer, cardiovascular disease, non-alcoholic fatty liver disease). Increases in body fat alter the body's response to insulin, potentially leading to insulin resistance. Increased fat also creates a pro-inflammatory state, and a prothrombotic state. Although the negative health consequences of obesity in the general population are well supported by the available evidence, health outcomes in certain subgroups seem to be improved at an increased BMI, a phenomenon known as the obesity survival paradox. The paradox was first described in 1999 in overweight and obese people undergoing haemodialysis, and has subsequently been found in those with heart failure and
Peripheral Artery Disease (PAD).In people with heart failure, those with a BMI between
7 30.0 and 34.9 had lower mortality than those with a normal weight. This has been attributed to the fact that people often lose weight as they become progressively more ill. Similar findings have been made in other types of heart disease. People with class I obesity and heart disease do not have greater rates of further heart problems than people of normal weight who also have heart disease. In people with greater degrees of obesity, however, risk of further events is increased. Even after cardiac bypass surgery, no increase in mortality is seen in the overweight and obese. One study found that the improved survival could be explained by the more aggressive treatment obese people receive after a cardiac event. Another found that if one takes into account Chronic Obstructive Pulmonary Disease
(COPD) in those with pad the benefit of obesity no longer exists.20
6.2 REVIEW OF LITERATURE:
A study conducted Factors affecting prevalence of overweight among 12- to 17- year-old urban adolescents in Hyderabad, India. The problem of overweight and obesity is not confined only to developed countries but is also widely prevalent in developing countries. The objective of this study was to assess the prevalence of overweight and obesity as defined by the International Obesity Task Force (IOTF) among school-age children in Hyderabad, India, and identify its associated factors. A cross-sectional and institutional study, adopting a multistage stratified cluster sampling procedure, was carried out during 2003 on adolescents 12 to 17 years of age of both sexes from Hyderabad, India.
The overall prevalence of overweight was 6.1% [95% confidence interval (CI): 4.2, 8.0] among boys and 8.2% among girls (CI: 6.0, 10.4); 1.6% and 1.0% were obese, respectively.
The logistic regression analysis revealed that the prevalence of overweight was 4 times higher among the adolescents of high socioeconomic status [odds ratio (OR): 4.1; CI: 2.25,
8 7.52], 3 times higher in those not participating in outdoor games (OR: 2.75; CI: 1.56, 4.72), and 1.92 times higher in those watching television > or =3 h/d (OR: 1.92; CI: 1.16, 3.18).21
A study conducted in India Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Department of Community Health and Epidemiology, Queen's University,
Kingston, Ontario K7L 3N6, Canada. [email protected] purposes of this systematic review were to present and compare recent estimates of the prevalence of overweight and obesity in school-aged youth from 34 countries and to examine associations between overweight and selected dietary and physical activity patterns. Data consisted of a cross-sectional survey of 137 593 youth (10-16 years) from the 34 (primarily European) participating countries of the 2001-2002 Health Behaviour in School-Aged Children Study.
The prevalence of overweight and obesity was determined based on self-reported height and weight and the international child body mass index standards. Logistic regression was employed to examine associations between overweight status with selected dietary and physical activity patterns. The two countries with the highest prevalence of overweight
(pre-obese + obese) and obese youth were Malta (25.4% and 7.9%) and the United States
(25.1% and 6.8%) while the two countries with the lowest prevalence were Lithuania (5.1% and 0.4%) and Latvia (5.9% and 0.5%). Overweight and obesity prevalence was particularly high in countries located in North America, Great Britain, and south-western
Europe. Within most countries physical activity levels were lower and television viewing times were higher in overweight compared to normal weight youth. In 91% of the countries examined, the frequency of sweets intake was lower in overweight than normal weight youth. Overweight status was not associated with the intake of fruits, vegetables, and soft drinks or time spent on the computer. In conclusion, the adolescent obesity epidemic is a global issue. Increasing physical activity participation and decreasing television viewing
9 should be the focus of strategies aimed at preventing and treating overweight and obesity in youth.22
A study about Television viewing as a cause of increasing obesity among children in the United States, 1986-1990.The prevalence of obesity among children and adolescents has increased, and television viewing has been suggested as a cause. We examined the relation between hours of television viewed and the prevalence of overweight in 1990, and the incidence and remission of overweight from 1986 to 1990 in a nationally representative cohort of 746 youths aged 10 to 15 years in 1990 whose mothers were 25 to 32 years old.
Overweight was defined as a body mass index higher than the 85th percentile for age and gender. We observed a strong dose-response relationship between the prevalence of overweight in 1990 and hours of television viewed. The odds of being overweight were 4.6
(95% confidence interval, 2.2 to 9.6) times greater for youth watching more than 5 hours of television per day compared with those watching 0 to 2 hours. When adjustments were made for previous overweight (in 1986), baseline maternal overweight, socioeconomic status, household structure, ethnicity, and maternal and child aptitude test scores, results were similar (odds ratio, 5.3; 95% confidence interval, 2.3 to 12.1). We also found significant relations between television viewing and increased incidence and decreased remission of overweight during this 4-year period, adjusted for baseline covariates. The adjusted odds of incidence were 8.3 (95% confidence interval, 2.6 to 26.5) times greater for youth watching more than 5 hours of television per day compared with those watching for 0 to 2 hours. Estimates of attributable risk indicate that more than 60% of overweight incidence in this population can be linked to excess television viewing time.23
A study again conducted about Determinants of Overweight and Obesity in Affluent
Adolescent in Surat City, South Gujarat region, India. Obesity is a major global burden.
Low levels of physical activity, TV watching, and dietary pattern are modifiable risk
10 factors for overweight and obesity in adolescent The overall prevalence of obesity and overweight was 6.55% and 13.9% (boys: 6.7% and 15.1%; girls 6.4% and 13.35%). Final model of multiple logistic regression analysis showed that important determinants of overweight and obesity were low levels of physical activity, watching television or playing computer games, and consuming junk foods, snacks and carbonated drinks.24
A study about Obesity and cardiovascular risk in children and adolescents.
Population Health Research Institute (PHRI) and David Braley Cardiac, Vascular, and
Stroke Research Institute (DBCVSRI), Hamilton, Ontario, Canada. The global prevalence of overweight and obesity in children and adolescents has increased substantially over the past several decades. These trends are also visible in developing economies like India.
Childhood obesity impacts all the major organ systems of the body and is well known to result in significant morbidity and mortality25. Obesity in childhood and adolescence is associated with established risk factors for cardiovascular diseases and accelerated atherosclerotic processes, including elevated blood pressure (BP), atherogenic dyslipidemia, atherosclerosis, metabolic syndrome; type II diabetes mellitus, cardiac structural and functional changes and obstructive sleep apnea. Probable mechanisms of obesity-related hypertension include insulin resistance, sodium retention, increased sympathetic nervous system activity, activation of the renin-angiotensin-aldosterone system and altered vascular function. Adiposity promotes cardiovascular risk clustering during childhood and adolescence. Insulin resistance has a strong association with childhood obesity. A variety of pro inflammatory mediators that are associated with cardio metabolic dysfunction are also known to be influenced by obesity levels. Obesity in early life promotes atherosclerotic disease in vascular structures such as the aorta and the coronary arteries. Childhood and adolescent adiposity has strong influences on the structure and function of the heart, predominantly of the left ventricle. Obesity compromises pulmonary
11 function and increases the risk of sleep-disordered breathing and obstructive sleep apnea.
Neglecting childhood and adolescent obesity will compromise the cardiovascular health of the pediatric population and is likely to result in a serious public health crisis in future.26
A study about environmental factors which leads to obesity conducted by Pune
University in Maharashtra, a changing environment has broadened food options and eating habits. Grocery stores stock their shelves with a greater selection of products. Pre-packaged foods, fast food restaurants, and soft drinks are also more accessible. While such foods are fast and convenient they also tend to be high in fat, sugar, and calories. Choosing many foods from these areas may contribute to an excessive calorie intake. Some foods are marketed as healthy, low fat, or fat-free, but may contain more calories than the fat containing food they are designed to replace. It is important to read food labels for nutritional information and to eat in moderation. Portion size has also increased. People may be eating more during a meal or snack because of larger portion sizes. This results in increased calorie consumption. If the body does not burn off the extra calories consumed from larger.27
All these factors are leading and alarming factors for obesity.
6.2 STATEMENT OF THE PROBLEM:
A comparative study to assess the effectiveness of structured teaching pragramme
(stp) on knowledge about factors contributing to obesity among housewives vs working women in a selected urban area of Bangalore.”
6.3 OBJECTIVES OF THE STUDY:
To assess the knowledge about factors contributing to obesity among working
women and the housewives.
12 To find the effectiveness of structured teaching programmed among working
women and housewives.
To find out the association between knowledge about obesity and selected
demographic variables like age, educational status, income, religion, occupation,
type of family and number of child birth.
6.4 HYPOTHESIS:
H01: There will not be significant difference between pre test and post test
knowledge regarding factors contributing to obesity among housewives and
working women.
H02: There will not be significant difference between housewives and working
women knowledge regarding factors contributing to obesity among housewives and
working women
H1: There will be significant difference between pre test and post test knowledge
regarding factors contributing to obesity among housewives and working women.
6.5. ASSUMPTION.
This study assumes that:-
It is assumed that women possess inadequate knowledge regarding factors
contributing to obesity among housewives and working women.
Appropriate education will help to increase the knowledge regarding factors
contributing to obesity among housewives and working women.
6.6. OPERATIONAL DEFINATIONS
Assess: Measure the level of knowledge about the prevention and management of
factors contributing to obesity among housewives and working women.
13 Effectiveness: Out come of the intervention is measured in terms of numerical
scores.
Knowledge : In this study knowledge refers to the correct response from the
mothers regarding factors contributing to obesity among housewives and working
women.
Housewives: Women who are married after 18years of age and don't have
employment.
Working women: women who are married after 18years of age and are employed.
Factors: Desired cause for any condition.
Obesity: Increased in fat levels of the body leading to weight gain in the adipose
tissue of the body which is also known as overweight.
6.7. SAMPLING CRITERIA:
1. Inclusion criteria
Women who are willing to participate.
Women who are present at the time of study.
Women who can understand Kannada & English.
Women who are housewives.
Women those who are working.
II. Exclusion criteria
Women who are absent during the study.
Women who are not willing to participate.
Women who cannot understand English or Kannada.
6.8. MATERIAL AND METHODS OF STUDY:-
Source of data: Data will be collected from housewives and working women in selected urban community area at Bangalore.
14 7. METHOD OF DATA COLLECTION:
1. Type of tool:
Part-I Demographic proforma
Part-II Structured interview Schedule
Part-III Determination of body mass index (BMI)
2. Research design: Comparative descriptive design
3. Research setting: The study will be conducted in selected urban community area at Bangalore.
4. Sample size: Sample comprises of 30 housewives and 30 working women.
5. Sample technique: Non probability, convenient sampling method will be used.
7.1 VARIBLES:-
Independent variable: Structured Teaching Programme regarding contributing factors of obesity among the housewives and working women.
Dependent variable: The dependent variable is level of knowledge regarding contributing factors of obesity among the housewives and working women.
Extraneous variable: Demographical variable like age, education , occupation, type of family, income, religion, number of child birth, diet habits and source of information.
7.2 PLANS FOR DATA ANALYSIS:
Descriptive statistics and inferential statistics will be used to analysis the data.
7.3 ETICHAL CONSIDERATION
Does the study require any investigation or investigations to be conducted on patients or humans or animals? If so please describe briefly.
No.
Has ethical clearance been obtained from your institution?
15 Yes.
BIBLIOGRAPHY:
1. en.wikipedia.org/wiki/Obesity_in_India
2. World Health Report (2008), Body mass Index, world health organization, 2008.
3. www.ultrafitnessdynamics.com/3803/obesity-a-killer-disease/
4. World Health Report (2011) Incidence report on Obesity, 2011.
5. Obesity Foundation of India “Journal of Obesity Factors” 2011 August.
16 6. Obesity in India article and report on “Obesity leading cause as Smoking in adults”
2006 November.
7. National Medical Expenditure Survey “Statistical data American Indian
Communities” 2009 July.
8. ajrccm.atsjournals.org/content/159/1/179
9. http://www.cdc.gov/nchs/nhanes/nh3data.htm
10. http://articles.timesofindia.indiatimes.com/2010-11-12/india/28245306_1_obesity-
india-and-china-overweight-rates
11. http://www.ncbi.nlm.nih.gov/pubmed/15373948
12. articles.timesofindia.indiatimes.com/2011-08-24/mumbai/29921602_1_obesity-
bariatric-surgeon-shashank-joshi
13. Press information bureau, Government of India, pib.nic.in/new site/erelease.aspx?
relid=31835
14. www.obesitydiscussion.com/forums/weight-loss-programs-worldwide/vlcc-
celebrates-anti-obesity-day-2751.html
15. http://www.medicaltourismco.com/india-hospitals/doctors/dr-anoop-misra.php
16. Mid day journal of health “ article obesity trends and factors affecting health” 2007
September Vol.7
17. www.herbalifescience.com/advisory-board/anoop-misra
18. http://en.wikipedia.org/wiki/Obesity
19. www.who.int/nutrition/publications/obesity/en/index.htm
20. http://en.wikipedia.org/wiki/Obesity
21. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3028965/
22. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3104708/
23. http://www.nature.com/oby/journal/v15/n8/abs/oby2007251a.html
17 24. http://www.phgfoundation.org/news/4427/
25. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3028965/
26. http://www.bookrags.com/research/obesity-genetic-factors-wog/
27. www.obesityasia.com/
18