Treating Postpartum Hemorrhage and Invasive Placenta Endovascular Techniques to Improve Outcomes in Patients with Abnormal Invasive Placenta
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OB/GYN EMERGENCIES Elyse Watkins, Dhsc, PA-C, DFAAPA DISCLOSURES
OB/GYN EMERGENCIES Elyse Watkins, DHSc, PA-C, DFAAPA DISCLOSURES I have no financial relationships to disclose. TOPICS Ovarian torsion Postpartum hemorrhage Ruptured ectopic Acute uterine inversion pregnancy Amniotic fluid embolism Acute menorrhagia Placental abruption OVARIAN TORSION OVARIAN TORSION .Tumors (benign and malignant) are implicated in 50-60% of cases of torsion .20% occur during pregnancy (corpus luteum cyst) .Unilateral or bilateral abdominal-pelvic pain, usually sudden onset .Exercise or movement exacerbates pain .Nausea and vomiting 70% .Pathophys: reduced venous return, stromal edema, internal hemorrhage, and infarction → necrosis OVARIAN TORSION .Physical exam variable .Ultrasonography with color Doppler .Surgical referral RUPTURED ECTOPIC PREGNANCY RUPTURED ECTOPIC PREGNANCY .All patients of reproductive age with a hx of missed menses and pelvic pain should be considered to have an ectopic pregnancy until proven otherwise. .A patient with missed menses, irregular vaginal bleeding, pelvic pain, syncope, abdominal pain, and/or dizziness should be managed as a ruptured ectopic pregnancy until proven otherwise. RUPTURED ECTOPIC PREGNANCY .Physical exam of pts with a ruptured ectopic can reveal pelvic tenderness, an adnexal mass, and evidence of hemodynamic compromise. .A transvaginal ultrasound will often show an adnexal mass and/or fluid in the pouch of Douglas. .The serum qualitative βHCG will be > 5 mIu/mL. RUPTURED ECTOPIC PREGNANCY HTTPS://YOUTU.BE/TNN1FPWHOXS RUPTURED ECTOPIC PREGNANCY .Immediately order an H/H, type and cross, and place large bore IV access for fluid support. .Laparotomy is performed when patients are hemodynamically unstable or if visualization during laparoscopy was difficult. .Patients with a ruptured ectopic pregnancy must be managed emergently and surgically! ACUTE MENORRHAGIA ACUTE MENORRHAGIA .Abnormal uterine bleeding (AUB) can result in acute blood loss that causes hemodynamic compromise so prompt evaluation of vital signs is important. -

Uterine Atony: Uterus Soft and Relaxed
Uterine atony: uterus soft and relaxed Placenta not delivered Treat for whole retained placenta If whole placenta still retained ■ Oxytocin ■ Manual removal with prophylactic antibiotics ■ Controlled cord traction ■ Intraumbilical vein injection (if no bleeding) Placenta delivered incomplete Treat for retained placenta fragments If bleeding continues ■ Oxytocin ■ Manage as uterine atony ■ Manual exploration to remove fragments ■ Gentle curettage or aspiration Be ready at all times to transfer to a higher-level facility if the Lower genital tract trauma: Treat for lower genital tract trauma If bleeding continues patient is not responding to the excessive bleeding or shock ■ Repair of tears ■ Tranexamic acid ■ treatment or a treatment cannot contracted uterus Evacuation and repair of haematoma be administered at your facility. Uterine rupture or dehiscence: Treat for uterine rupture or dehiscence If bleeding continues excessive bleeding or shock ■ Laparotomy for primary repair of uterus ■ Tranexamic acid Start intravenous oxytocin infusion ■ Hysterectomy if repair fails and consider: • uterine massage; • bimanual uterine compression; Uterine inversion: Treat for uterine inversion If laparotomy correction not successful • external aortic compression; and uterine fundus not felt ■ Immediate manual replacement ■ Hysterectomy • balloon or condom tamponade. abdominally or visible in vagina ■ Hydrostatic correction ■ Manual reverse inversion Transfer with ongoing intravenous (use general anaesthesia or wait for effect uterotonic infusion. Accompanying -

Reduction of Subacute Uterine Inversion by Haultain's Method: A
This open-access article is distributed under Creative Commons licence CC-BY-NC 4.0. CASE REPORT Reduction of subacute uterine inversion by Haultain’s method: A case report E Ziki,1 MB ChB, MMed; S Madombi,1 MB ChB; C Chidhakwa,1 FCOG; M G Madziyire,1 MMed; N Zakazaka,2 MMed 1 Department of Obstetrics and Gynaecology, University of Zimbabwe, College of Health Sciences, Harare, Zimbabwe 2 Department of Obstetrics and Gynaecology, Parirenyatwa Central Hospital, Harare, Zimbabwe Corresponding author: E Ziki ([email protected]) Uterine inversion is a rare but potentially life-threatening obstetric emergency of unknown aetiology, which is often associated with inadvertent traction on the umbilical cord before separation of the placenta. Here we report a case of a 26-year-old woman who presented with a day’s history of uterine inversion after an attempt to remove a retained placenta following a second-trimester miscarriage. Reduction was attempted in casualty without success and she was taken to theatre for surgical reduction under anaesthesia. Reduction was eventually achieved using the Haultain method. S Afr J Obstet Gynaecol 2017;23(3):78-79. DOI:10.7196/SAJOG.2017.v23i3.1274 Uterine inversion is defined as the ‘turning inside out of the fundus of subacute uterine inversion was made and resuscitation was into the uterine cavity’ and the incidence is about 1 in 3 737.[1] performed using ringer’s lactate fluid and 4 units of packed red Active management of the third stage of labour resulted in a 4.4- blood cells. She was commenced on intravenous antibiotics. -
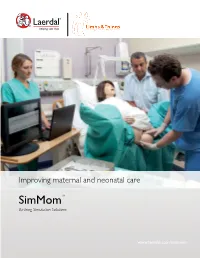
Simmomtm Birthing Simulation Solutions
Improving maternal and neonatal care SimMomTM Birthing Simulation Solutions www.laerdal.com/simmom Innovative simulation Improving patient safety Preventing adverse outcomes during birth Simulation has gathered increasing acceptance over the Simulation training is unique in its ability to facilitate effective years as an integral part of healthcare training and as a team training. By bringing together multi-disciplinary fundamental approach to help improve patient safety. healthcare professionals in a simulation to rehearse both common birthing scenarios and emergency critical incidents; In the field of obstetrics, research into suboptimal patient early recognition of birth complications, correct diagnosis outcomes have identified the following key contributory and rapid, coordinated action from the delivery team can factors: confusion in roles and responsibilities; lack of cross be perfected for improved outcomes. monitoring; failure to prioritize and perform clinical tasks in a structured, coordinated manner; poor communication and lack of organizational support. Reference : The Joint Commission, 2004, Draycott et al. 2009 2 Simulation by Laerdal and Limbs & Things SimMomTM A complete solution A progressive partnership SimMomTM is an advanced full-body birthing simulator with By integrating the strengths of the PROMPT birthing accurate anatomy and functionality. SimMom has been simulator from Limbs & Things with the ALS Simulator developed to provide you with a comprehensive simulation from Laerdal, SimMom provides anatomical accuracy and solution to support multi-disciplined staff in obstetric and authentic simulation experiences that together, facilitate midwifery care, enabling refinement of individual skills and valuable learning experiences for a wide range of midwifery team performance. and obstetric skills. With a range of Technical and Educational Services as well as pre-programmed scenarios to ease educator preparation time, SimMom is the optimal simulation experience. -

Sexual and Reproductive Health
Sexual and Reproductive Health Guide for the Care of the Most Relevant Obstetric Emergencies Guide for the Care of the Most Relevant Obstetric Emergencies Fescina R*, De Mucio B*, Ortiz El**, Jarquin D**. *Latin American Center for Perinatology Women and Reproductive Health **Latin American Federation of Societies of Obstetrics and Gynecology Scientific Publication CLAP/WR N° 1594-02 Latin American Center for Perinatology Women and Reproductive Health CLAP/ WR Sexual and Reproductive Health Cataloguing-in-Publication Data Fescina R, De Mucio B, Ortiz E, Jarquin D. Guide for the care of the most relevant obstetric emergencies. Montevideo: CLAP/WR; 2013. (CLAP/WR. Scientific Publication; 1594-02) ISBN: 1. Maternal Mortality - Prevention 2. Pregnancy Complications 3. Placenta Previa 4. Pre-Eclampsia 5. Pregnancy Complications, Infectious 6. Eclampsia 7. Postnatal care 8. Postpartum Hemorrhage 9. Pregnancy, High-Risk 10.Pregnancy, Ectopic I. CLAP/WR II.Title The Pan American Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. Applications and inquiries should be addressed to Editorial Services, Area of Knowledge Management and Communications (KMC), Pan American Health Organization, Washington, D.C., U.S.A. The Latin American Center for Perinatology, Women and Reproductive Health (CLAP/WR), Area of Family and Community Health, Pan American Health Organization, will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © Pan American Health Organization, 2013 All rights reserved. Publications of the Pan American Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. -

Retained Placenta After Vaginal Birth - Uptodate
2019/3/17 Retained placenta after vaginal birth - UpToDate Official reprint from UpToDate® www.uptodate.com ©2019 UpToDate, Inc. and/or its affiliates. All Rights Reserved. Retained placenta after vaginal birth Author: Andrew Weeks, MD, MRCOG Section Editor: Vincenzo Berghella, MD Deputy Editor: Vanessa A Barss, MD, FACOG All topics are updated as new evidence becomes available and our peer review process is complete. Literature review current through: Feb 2019. | This topic last updated: Dec 12, 2018. INTRODUCTION The third stage of labor is the interval from delivery of the infant to expulsion of the placenta. Delayed separation and expulsion of the placenta is a potentially life-threatening event because it interferes with normal postpartum contraction of the uterus, which can lead to hemorrhage. This topic will discuss the diagnosis and management of a retained placenta after vaginal birth. Management of retained products of conception after a miscarriage or pregnancy termination is reviewed separately. (See "Retained products of conception".) DEFINITION Retained placenta can be defined as lack of expulsion of the placenta within 30 minutes of delivery of the infant [1,2]. This is a reasonable definition in the third trimester when the third stage of labor is actively managed (ie, administration of a uterotonic agent before delivery of the placenta, controlled cord traction) because 98 percent of placentas are expelled by 30 minutes (figure 1) in this setting [3]. Physiological management of the third stage (ie, delivery of the placenta without the use of uterotonic agents or cord traction) increases the frequency of retained placenta: only 80 percent of placentas are expelled by 30 minutes (figure 1) and it takes about 60 minutes before 98 percent of placentas are expelled. -

Macroscopic Examination of Fetal Appendices in Delivery Room: Good Practice at Panzi Hospital
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Walala BD et al. Int J Reprod Contracept Obstet Gynecol. 2020 May;9(5):2215-2221 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20201841 Clinical Problem Solving Macroscopic examination of fetal appendices in delivery room: good practice at Panzi hospital Boengandi Walala D.1*, Nyakio Ngeleza O.1, Mukanire Ntakwinja B.1, Raha Maroyi K.1, Katenga Bosunga G.2, Mukwege Mukengere D.1 1Department of Gynecology and Obstetrics, Panzi Hospital, School of Medicine, Evangelical University in Africa, Bukavu, DR Congo 2Department of Gynecology and Obstetrics, Kisangani University Clinics, School of Medicine, Kisangani University, Kisangani, DR Congo Received: 14 January 2020 Revised: 20 February 2020 Accepted: 28 February 2020 *Correspondence: Dr. Boengandi Walala D., E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT The review of fetal appendices is described in the literature, and its importance is well established. Indeed, pathological findings in the placenta can provide information on the pathogenesis of the fetus, including intrauterine growth retardation, mental retardation or neurodevelopmental disorders. This helps to understand a child's disability, but also maternal complications such as preeclampsia. Despite the relevant information provided by the various studies, fetal appendices are not systematically examined in several maternity hospitals in our country, DR Congo. -

Chronic Uterine Inversion Due to Myoma Geburt
Scientific Foundation SPIROSKI, Skopje, Republic of Macedonia Open Access Macedonian Journal of Medical Sciences. 2020 Dec 22; 8(C):223-225. https://doi.org/10.3889/oamjms.2020.5547 eISSN: 1857-9655 Category: C - Case Reports Section: Case Report in Gynecology and Obstetrics Chronic Uterine Inversion due to Myoma Geburt Bobby Indra Utama* Department of Obstetrics and Gynecology, Division of Urogynecolgy, RSUP Dr. M. Djamil, Padang, Indonesia Abstract Edited by: Igor Spiroski BACKGROUND: Uterine inversion is a rare obstetric emergency but potentially serious complication of labor. This Citation: Utama BI. Chronic Uterine Inversion due to Myoma Geburt. Open Access Maced J Med Sci. 2020 disease characterized by severe pain and can cause life-threatening condition. If these not immediately identified, the Dec 22; 8(C):223-225. massive and underestimated blood loss can lead to hypovolemic shock. Therefore, early diagnosis and management https://doi.org/10.3889/oamjms.2020.5547 of this condition is desirable. The objective of the study was to report on the management of chronic uterine inversion Keywords: Uterine inversion; Myoma geburt *Correspondence: Bobby IndraUtama, Department due to myoma geburt. of Obstetrics and Gynecology, Division of Urogynecolgy, RSUP Dr. M. Djamil Padang, Indonesia. CASE REPORT: A 46-year-old patient was admitted to the gynecology ward of Dr. M. Djamil Central General E-mail: [email protected]; Hospital with slight bleeding from vagina for 1 month ago with 2–3 pieces of underwear dark red colored, with pain. 08116660500 Received: 28-Oct-2020 Bleeding from the vagina often recurs. There was a mass revealed from vagina with size as big as baby’s head. -

Uterine Inversion - an Obstetrician’S Nightmare: a Series of 3 Cases of Uterine Inversion and a Review of Management Options
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Jalvee RG et al. Int J Reprod Contracept Obstet Gynecol. 2021 May;10(5):2050-2054 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: https://dx.doi.org/10.18203/2320-1770.ijrcog20211536 Case Series Uterine inversion - an obstetrician’s nightmare: a series of 3 cases of uterine inversion and a review of management options Rashmi G. Jalvee*, Reena J. Wani Department of Obstetrics and Gynecology, HBT Medical College and Dr. R. N. Cooper Hospital, Mumbai, Maharashtra, India Received: 23 February 2021 Revised: 03 April 2021 Accepted: 14 April 2021 *Correspondence: Dr. Rashmi G. Jalvee, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Acute puerperal uterine inversion is an extremely rare but potentially life-threatening complication in which the uterine fundus collapses within the endometrial cavity and beyond. Although the causes of uterine inversion are unclear, several predisposing factors have been described. Maternal mortality is extremely high unless the condition is recognized and corrected. We present here a series of three cases of uterine inversion managed in our hospital over a period of 3 years. Our first case, Mrs XYZ referred to our hospital after vaginal delivery followed by postpartum collapse. The patient was in hypovolemic shock with 2nd degree uterine inversion. Second case, Mrs ABC referred to our hospital after vaginal delivery and mass coming out of the vagina. -

Subacute Uterine Inversion Following an Induced Abortion in a Teenage Girl: a Case Report Asiphas Owaraganise* , Leevan Tibaijuka and Joseph Ngonzi
Owaraganise et al. BMC Women's Health (2020) 20:220 https://doi.org/10.1186/s12905-020-01089-0 CASE REPORT Open Access Subacute uterine inversion following an induced abortion in a teenage girl: a case report Asiphas Owaraganise* , Leevan Tibaijuka and Joseph Ngonzi Abstract Background: Subacute uterine inversion is a very rare complication of mid-trimester termination of pregnancy that should be considered in a situation where unsafe abortion occurs. Case presentation: We present a case of subacute uterine inversion complicated by hypovolemic shock following an unsafe abortion in a 17-year-old nulliparous unmarried girl. She presented with a history of collapse, mass protruding per vagina that followed Valsalva, and persistent lower abdominal pain but not vaginal bleeding. This followed her second attempt to secretly induce an abortion at 18 weeks amenorrhea. On examination, she was agitated, severely pale, cold on palpation, with an axillary temperature of 35.8 °C, a tachycardia of 143 beats per minute and unrecordable low blood pressure. The abdomen was soft and non-tender with no palpable masses; the uterine fundus was absent at its expected periumbilical position and cupping was felt instead. A fleshy mass with gangrenous patches protruding in the introitus was palpated with no cervical lip felt around it. We made a clinical diagnosis of subacute uterine inversion complicated with hypovolemic shock and initiated urgent resuscitation with crystalloid and blood transfusion. Non-operative reversal of the inversion failed. Surgery was done to correct the inversion followed by total abdominal hysterectomy due to uterine gangrene. Conclusion: Our case highlights an unusual presentation of subacute uterine inversion following unsafe abortion. -
Uncontrollable Uterine Atony After Replacement of Uterine Inversion
Katsura et al. Journal of Medical Case Reports (2020) 14:181 https://doi.org/10.1186/s13256-020-02528-0 CASE REPORT Open Access Uncontrollable uterine atony after replacement of uterine inversion managed by hysterectomy: a case report Daisuke Katsura1* , Suzuko Moritani2, Shunichiro Tsuji1, Kounosuke Suzuki1, Kazutaka Yamada1, Mizuki Ohashi1, Fuminori Kimura1 and Takashi Murakami1 Abstract Background: Uterine inversion may cause massive hemorrhage, resulting in maternal deterioration and death. Replacement of the inverted uterus must be performed as soon as possible. As time passes, the inverted uterus becomes atonic and necrotic, and a surgical approach may be required. Case presentation: A 27-year-old Japanese woman was admitted to our hospital 4 hours postpartum with increased hemorrhage after the replacement of an inverted uterus. Recurrent inversion was diagnosed, and though the atonic uterus was replaced again by the Johnson maneuver, hemorrhage persisted. Balloon tamponade was not successful in stopping the hemorrhage, and uterine artery embolization was performed. Bleeding resumed the next day on removal of the balloon, and hysterectomy was performed. Massive hemorrhage, coagulopathy, and uterine necrosis caused uterine atony, and the reperfused blood flow on replacement of the ischemic uterus increased hemorrhage. Conclusions: Cases of uterine inversion with coagulopathy lasting for more than 4 hours may require a surgical intervention, and uterine replacement may have to be delayed until the maternal hemodynamic condition is stabilized. Uterine replacement under laparotomy may be also be considered due to the risk of increased hemorrhage. Keywords: uterine inversion, replacement, atony of uterus, reperfused blood flow, ischemic uterus, case report Background makes restoration of the normal uterus position difficult Although uterine inversion is a rare obstetric emergency [2, 3]. -

Postpartum Hemorrhage
Postpartum Hemorrhage Susan Leong-Kee, MD Assistant Professor Director of Simulation Baylor College of Medicine Department of Obstetrics and Gynecology I have no financial conflicts of interest to disclose Agenda • Postpartum hemorrhage didactic overview • Simulation skills training • Debrief Objectives • Review the incidence of pregnancy-related hemorrhage, specifically postpartum hemorrhage (PPH) • Review the pregnancy-related vascular changes that can lead to PPH • Identify risk factors for PPH • Recognize prevention and develop management skills Incidence Causes of maternal death worldwide by percentage (Source: WHO) • Hemorrhage is one of 9 the leading causes of 11 28 maternal death worldwide 8 • PPH: 27% of maternal mortality (WHO, 2014) 14 • 1 woman dies every 4 27 minutes due to PPH Pre-existing medical conditions (ACOG, 2013) Hemorrhage Pregnancy related hypertension Abortion complications Infections Obstetric morbidity + mortality in the U.S. • Rate of maternal deaths has tripled from 6 per 100,000 in 1996 to 17 per 100,000 annual births in 1999 • Blood transfusions increased 92% during delivery hospitalizations between 1997 and 2005 Annual Postpartum Hemorrhage Rates, United States, 1994-2006 7 Defining postpartum hemorrhage • Vaginal delivery: – Greater than 500 mL blood loss • Cesarean section: – Greater than 1000 mL blood loss Hemodynamic changes of pregnancy • Plasma volume expansion • Increase in red blood cell mass • Cardiac output (SV X HR =CO) increases • Pro-coagulant factors (i.e., fibrinogen) increase Classification