Sexual and Reproductive Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OB/GYN EMERGENCIES Elyse Watkins, Dhsc, PA-C, DFAAPA DISCLOSURES
OB/GYN EMERGENCIES Elyse Watkins, DHSc, PA-C, DFAAPA DISCLOSURES I have no financial relationships to disclose. TOPICS Ovarian torsion Postpartum hemorrhage Ruptured ectopic Acute uterine inversion pregnancy Amniotic fluid embolism Acute menorrhagia Placental abruption OVARIAN TORSION OVARIAN TORSION .Tumors (benign and malignant) are implicated in 50-60% of cases of torsion .20% occur during pregnancy (corpus luteum cyst) .Unilateral or bilateral abdominal-pelvic pain, usually sudden onset .Exercise or movement exacerbates pain .Nausea and vomiting 70% .Pathophys: reduced venous return, stromal edema, internal hemorrhage, and infarction → necrosis OVARIAN TORSION .Physical exam variable .Ultrasonography with color Doppler .Surgical referral RUPTURED ECTOPIC PREGNANCY RUPTURED ECTOPIC PREGNANCY .All patients of reproductive age with a hx of missed menses and pelvic pain should be considered to have an ectopic pregnancy until proven otherwise. .A patient with missed menses, irregular vaginal bleeding, pelvic pain, syncope, abdominal pain, and/or dizziness should be managed as a ruptured ectopic pregnancy until proven otherwise. RUPTURED ECTOPIC PREGNANCY .Physical exam of pts with a ruptured ectopic can reveal pelvic tenderness, an adnexal mass, and evidence of hemodynamic compromise. .A transvaginal ultrasound will often show an adnexal mass and/or fluid in the pouch of Douglas. .The serum qualitative βHCG will be > 5 mIu/mL. RUPTURED ECTOPIC PREGNANCY HTTPS://YOUTU.BE/TNN1FPWHOXS RUPTURED ECTOPIC PREGNANCY .Immediately order an H/H, type and cross, and place large bore IV access for fluid support. .Laparotomy is performed when patients are hemodynamically unstable or if visualization during laparoscopy was difficult. .Patients with a ruptured ectopic pregnancy must be managed emergently and surgically! ACUTE MENORRHAGIA ACUTE MENORRHAGIA .Abnormal uterine bleeding (AUB) can result in acute blood loss that causes hemodynamic compromise so prompt evaluation of vital signs is important. -

Heterotopic Cervical Pregnancy
Elmer ress Case Report J Clin Gynecol Obstet. 2015;4(4):307-311 Heterotopic Cervical Pregnancy Mathangi Thangavelua, b, Ravinder Kalkata Abstract tenderness or cervical excitation. Initial hormonal investiga- tions showed BHCG levels were raised to 17,276 IU and ini- We report a rare case of heterotopic cervical pregnancy, which posed tial ultrasound was suggestive of minimal retained products diagnostic challenge. With increasing IVF treatment and raising ce- of conception (Fig. 1). However, a repeat BHCG showed an sarean section rate, there is increasing incidence for non-tubal hetero- increasing trend reaching up to 29,971 IU in 96 h. A repeat topic pregnancy. We have discussed the clinical course of our case, transvaginal scan showed the endometrial cavity had mixed diagnosis and management of cervical pregnancy and some good echoes and multiple cystic spaces, largest measuring 6 × 7 × medical practices to avoid missing atypical presentations of ectopic 8 mm with color flow suggesting a possible molar pregnancy pregnancy. (Fig. 2). Bilateral ovarian cysts were present in both adnexa. Laparoscopy and dilatation and curettage were arranged Keywords: Cervical pregnancy; Heterotopic; Ectopic in view of high BHCG levels and no clear evidence of intrau- terine pregnancy. Laparoscopy was negative for tubal ectopic pregnancy and dilatation and curettage was performed. Post- operatively BHCG levels were monitored to ensure its levels were declining. The levels initially dropped to 2,611 IU from Introduction 29,971 IU in a week after D&C. However, the subsequent BHCG levels doubled to 4,207 IU 2 weeks after D&C. With We report an extremely rare case of spontaneous heterotopic the knowledge of earlier scan findings, raising BHCG levels cervical pregnancy who needed multiple investigations before raised the concern of persistent trophoblastic disease. -

Uterine Atony: Uterus Soft and Relaxed
Uterine atony: uterus soft and relaxed Placenta not delivered Treat for whole retained placenta If whole placenta still retained ■ Oxytocin ■ Manual removal with prophylactic antibiotics ■ Controlled cord traction ■ Intraumbilical vein injection (if no bleeding) Placenta delivered incomplete Treat for retained placenta fragments If bleeding continues ■ Oxytocin ■ Manage as uterine atony ■ Manual exploration to remove fragments ■ Gentle curettage or aspiration Be ready at all times to transfer to a higher-level facility if the Lower genital tract trauma: Treat for lower genital tract trauma If bleeding continues patient is not responding to the excessive bleeding or shock ■ Repair of tears ■ Tranexamic acid ■ treatment or a treatment cannot contracted uterus Evacuation and repair of haematoma be administered at your facility. Uterine rupture or dehiscence: Treat for uterine rupture or dehiscence If bleeding continues excessive bleeding or shock ■ Laparotomy for primary repair of uterus ■ Tranexamic acid Start intravenous oxytocin infusion ■ Hysterectomy if repair fails and consider: • uterine massage; • bimanual uterine compression; Uterine inversion: Treat for uterine inversion If laparotomy correction not successful • external aortic compression; and uterine fundus not felt ■ Immediate manual replacement ■ Hysterectomy • balloon or condom tamponade. abdominally or visible in vagina ■ Hydrostatic correction ■ Manual reverse inversion Transfer with ongoing intravenous (use general anaesthesia or wait for effect uterotonic infusion. Accompanying -

Cornual Pregnancy Discovered on CT Scan: a Case Report Baadi F1*, Gakosso C1, Rachid2, Oubahha2, Fakhir B2, Zouita I1, Jalal H1
Scholars International Journal of Obstetrics and Gynecology Abbreviated Key Title: Sch Int J Obstet Gynec ISSN 2616-8235 (Print) |ISSN 2617-3492 (Online) Scholars Middle East Publishers, Dubai, United Arab Emirates Journal homepage: https://saudijournals.com Case Report Cornual Pregnancy Discovered on CT scan: A Case Report Baadi F1*, Gakosso C1, Rachid2, Oubahha2, Fakhir B2, Zouita I1, Jalal H1 1Radiology Department, Mother and Child Hospital, Mohammed VI CHU, Cadi Ayyad University, Marrakech 2Obstetrics and Gynecology Department, Mother and Child Hospital, Mohammed VI CHU, Cadi Ayyad University, Marrakech DOI: 10.36348/sijog.2021.v04i01.004 | Received: 26.11.2020 | Accepted: 09.12.2020 | Published: 29.01.2021 *Corresponding author: Baadi F Abstract Cornual pregnancy is uncommon among ectopic pregnancies. A diagnosis of cornual pregnancy remains challenging, and rupture of a cornual pregnancy causes catastrophic consequence due to massive bleeding. The purpose of this study is to determine the contribution of imaging in the early diagnosis and management of this rare entity, in order to avoid complications. Keywords: Cornual pregnancy, US, CT, MRI. Copyright © 2021 The Author(s): This is an open-access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-NC 4.0) which permits unrestricted use, distribution, and reproduction in any medium for non-commercial use provided the original author and source are credited. NTRODUCTION This patient presents as obstetric history: fetal I death in utero estimated at 34 weeks pregnant with pre- Cornual pregnancy is a rare form of ectopic eclampsia. pregnancy, defined by the implantation of a gestational sac in the horn of the uterus, occurs in 2% of ectopic According to her gynecologist performed an pregnancies [1]. -

Successful Treatment of Cervical Ectopic Pregnancy with Multi Dose
Case Report iMedPub Journals Gynaecology & Obstetrics Case report 2020 www.imedpub.com ISSN 2471-8165 Vol.6 No.2:14 DOI: 10.36648/2471-8165.6.2.94 Successful Treatment of Cervical Ectopic Iqbal S1*, Iqbal J2, Nowshad N1 and Pregnancy with Multi Dose Methotrexate Mohammad K1 Therapy 1 Department of Obstetrics and Gynecology, Latifa Hospital, Dubai Health Authority Jaddaf, Dubai, UAE 2 Department of Medical Education, Dubai Abstract Medical University, Dubai, UAE Cervical ectopic pregnancies account for less than 1% of all pregnancies. Earlier, it was associated with significant hemorrhage and was treated presumptively with hysterectomy. With the advent of enhanced ultrasound techniques, early *Corresponding author: Iqbal S detection of these pregnancies has led to the development of more effective conservative management. We present a case of a cervical ectopic pregnancy successfully treated with multi-dose Methotrexate therapy. [email protected] A 37-year-old lady, G3P0+2, pregnant for 9 weeks and 4 days, presented with bleeding per vagina, mild lower abdomen and back pain. Serum Beta-hCG done Department of Obstetrics and Gynecology, 5 days ago was 950 mIU/mL. She was diagnosed as ectopic cervical pregnancy Latifa Hospital, Dubai Health Authority by clinical examination which was confirmed by transvaginal ultrasonography Jaddaf, Dubai, UAE. and subsequently managed by Methotrexate (MTX) Hybrid double dose protocol. Due to rising Beta-hCG and continuous bleeding, it was modified to Multi dose Tel: 971569400124 Methotrexate Therapy. Thereafter, the patient was asymptomatic with falling beta-hCG and she was put on a weekly follow up in the clinic. Keywords: Ectopic pregnancy; Cervical pregnancy; Methrotrexate; Gynaecology Citation: Iqbal S, Iqbal J, Nowshad N, Mohammad K (2020) Successful Treatment of Cervical Ectopic Pregnancy with Multi Received: March 31, 2020; Accepted: May 02, 2020; Published: May 06, 2020 Dose Methotrexate Therapy. -

Terminology for Describing Normally-Sited and Ectopic Pregnancies on Ultrasound: ESHRE Recommendations for Good Practice
Terminology for describing normally-sited and ectopic pregnancies on ultrasound: ESHRE recommendations for good practice Set-up The invitation to review was sent to the members of the SIG Implantation and early pregnancy (n=7443 email addresses). In addition, the invitation was mailed to the members of the ESHRE Executive Committee and the Committee of National Representatives (n=74). An announcement was also placed on the eshre.eu website. The stakeholder review started on 20th of April 2020, and was closed after 4 weeks, on the 18th of May 2020. Summary Thirty reviewers, representing nineteen countries, submitted a total of 212 comments (on average 7 comments per reviewer). All reviewers are listed on page 2. IMPACT OF THE COMMENTS 9% General comment or language correction 25% Comments resulting in a change Comments to which a reply 66% was formulated This report comprises the list of reviewers, and the overview of comments, with a reply from the working group. Page 1 of 40 List of reviewers Name Country Organization Masoud Kamrava Iran Steven Goldstein USA Ulrike Metzger France Grigorios Derdelis Greece Luca Savelli Italy Gangaraju Buvaneswari India Mridu Sinha India Onur Erol Turkey Aboubakr Mohamed Elnashar Egypt Jiuzhi Zeng China Carlos Calhaz-Jorge Portugal Dr. Nidaa Qatar Attilio Di Spiezio Sardo Italy Melinda Mitranovici Romania Ali Sami Gurbuz Turkey Philippe Merviel France Roy Farquharson UK Ilan Timor USA Alessandra Pipan United Arab Emirates Company, Taiwan IVF Wen Jui Yang Taiwan Group Center Lorenzo Abad de Velasco Spain Monica Varma India Kumaran Aswathy India Annick Geril Belgium Snezana Vidakovic Serbia Lukasz Polanski, Miriam Baumgarten, Rebecca McKay, Laura Rutherford, Ouma Pillay, Anita Jeyaraj, Kanna Jayaprakasan and Kamal Ojha UK organization Mohamed Shahin UK Mohsen M El-Sayed UK International Society of Ultrasound in Obstetrics and Gynecology (ISUOG) ISUOG European Niche taskforce group of the ESGE and international Prof. -

Sonography in First Trimester Bleeding
Review Sonography in First Trimester Bleeding Manjiri Dighe, MD,1 Carlos Cuevas, MD,1 Mariam Moshiri, MD,1 Theodore Dubinsky, MD,1 Vikram S. Dogra, MD2 1 Department of Radiology, University of Washington Medical Center, Seattle, WA 98195 2 Department of Imaging Sciences, University of Rochester School of Medicine, 601 Elmwood Avenue, Box 648, Rochester, NY 14642 Received 19 April 2007; accepted 1 October 2007 ABSTRACT: Vaginal bleeding is the most common however, the most common cause of bleeding is cause of presentation to the emergency department spotting caused by implantation of the conceptus in the first trimester. Approximately half of patients into the endometrium. A complete assessment of with first trimester vaginal bleeding will lose the preg- the first trimester pregnancy requires correlation nancy. Clinical assessment is difficult, and sonogra- of serum b human chorionic gonadotropin (b- phy is necessary to determine if a normal fetus is hCG) levels with the appearance of the gesta- present and alive and to exclude other causes of bleeding (eg, ectopic or molar pregnancy). Diagnosis tional sac (GS) using sonography. of a normal intrauterine pregnancy not only helps the physician in terms of management but also gives psy- SPONTANEOUS ABORTION chologic relief to the patient. Improved ultrasound technology and high-frequency endovaginal trans- Spontaneous abortion is defined as the termina- ducers have enabled early diagnosis of abnormal and tion of a pregnancy before the twentieth completed ectopic pregnancies, decreasing maternal morbidity week of gestation. Sixty-five percent of spontane- and mortality. The main differential considerations of ous abortions occur in the first 16 weeks of preg- first trimester bleeding are spontaneous abortion, ec- nancy. -

Ruptured Subcapsular Hematoma of the Liver Due to Pre‑Eclampsia Presenting As Interstitial Pregnancy and the Role of Intra‑Abdominal Packing
[Downloaded free from http://www.njcponline.com on Friday, February 20, 2015, IP: 41.135.175.148] || Click here to download free Android application for this journal Case Report Ruptured subcapsular hematoma of the liver due to pre‑eclampsia presenting as interstitial pregnancy and the role of intra‑abdominal packing NC Ngene, N Amin1, J Moodley2 Department of Obstetrics and Gynaecology, Edendale Hospital Pietermaritzburg, 1School of Education, 2Women’s Health and HIV Research Group, University of KwaZulu‑Natal, Durban, South Africa Abstract Ruptured subcapsular hematoma of the liver (RSHL) can mimic ruptured interstitial pregnancy because each of these conditions occasionally presents at the same gestational period and both do manifest hemodynamic instability. The similarities between the two conditions pose a diagnostic challenge, especially in an unbooked patient. We report a case of an unbooked primigravida, at 21 weeks of gestation, who arrived at a regional hospital with evidence of intra‑abdominal bleeding and hypovolemic shock. She was diagnosed as potentially having a ruptured interstitial pregnancy. During the ensuing emergency laparotomy, RSHL was discovered, the area around the ruptured liver capsule was packed with large abdominal swabs, and the patient recovered. This case report illustrates the need to consider RSHL in patients presenting with features of ruptured interstitial pregnancy, as this will assist in the planning of intraoperative care. We also describe abdominal packing and highlight the need for this essential -

Cornual Pregnancy and Interstitial Pregnancy Kornual Ve Interstisyal Gebelik
Letter to the Editor 61 Cornual pregnancy and interstitial pregnancy Kornual ve interstisyal gebelik Cemil Yaman Department of Obstetrics and Gynecology, General Hospital of Linz, Linz, Austria Dear editor; Interstitial pregnancies often progress without symptoms until a rupture occurs later than other tubal pregnancies. The man- Comments regarding the published case report from Günenç agement of cornual pregnancy can be complicated because et al “Laparoscopic surgery of interstitial (cornual) pregnancy of malformations (1, 2). Due to these facts there is a need to 2009 11-2: 102-4 in TGGA” Authors reported: “The terms cor- differentiate between these pathologies. Furthermore, the nual and interstitial pregnancy are used synonymously (page occurrence of an angular pregnancy, which is distinguished 102, line 17) to define pregnancy implanted in the interstitial from cornual and interstitial pregnancy anatomically by its part of the fallopian tube which is the proximal portion that is embodied within the muscular wall of the uterus”. position in relation to the round ligament, should be taken into the diagnostic considerations. Unlike the interstitial and Comments cornual pregnancies, angular pregnacies may have a favor- able outcome (4). In the North American literature and in a small number of European literature, the terms “interstitial pregnancy” and Conflict of interest “cornual pregnancy” are used synonymously. However, it No conflict of interest is declared by authors. seems that recent studies indicate differences between these two pregnancies (1-3). References Cornual pregnancy is a pregnancy in one horn of a bircor- nuated uterus or, by extension, in one half of a septated or 1. Malinowski A, Bates SK. -

Ectopic Pregnancy Management: Tubal and Interstitial SIGNS / SYMPTOMS DIAGNOSIS
8/29/19njm Ectopic Pregnancy Management: Tubal and interstitial SIGNS / SYMPTOMS Pain and vaginal bleeding are the hallmark symptoms of ectopic pregnancy. Pain is almost universal; it is generally lower abdominal and unilateral. Bleeding is also very common following a short period of amenorrhea. Physical exam may reveal a tender adnexal mass, often mentioned in texts, but noted clinically only 20 percent of the time. Furthermore, it may easily be confused with a tender corpus luteum of a normal intrauterine pregnancy. Finally signs and symptoms of hemoperitoneum and shock can occur, including a distended, silent, “doughy” abdomen, shoulder pain, bulging cul de sac into the posterior fornix of the vagina, and hypotension. DIAGNOSIS Initially, serum hCG rises, but then usually plateaus or falls. Transvaginal ultrasound scanning is a key diagnostic tool and can rapidly make these diagnoses: 1. Ectopic is ruled out by the presence of an intrauterine pregnancy with the exception of rare heterotopic pregnancy 2. Ectopic is proven when a gestational sac and an embryo with a heartbeat is seen outside of the uterus 3. Ectopic is highly likely if ANY adnexal mass distinct from the corpus luteum or a significant amount of free pelvic fluid is seen. When ultrasound is not definitive, correlation of serum hCG levels is important. If the hCG is above the “discriminatory zone” of 3000 mIU/ml IRP, a gestational sac should be visible on transvaginal ultrasound. The discriminatory zone varies by ultrasound machine and sonographer. If an intrauterine gestational sac is not visible by the time the hCG is at, or above, this threshold, the pregnancy has a high likelihood of being ectopic. -
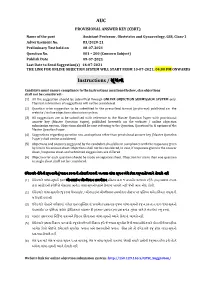
AUC Instructions / ૂચના
AUC PROVISIONAL ANSWER KEY (CBRT) Name of the post Assistant Professor, Obstetrics and Gynaecology, GSS, Class-1 Advertisement No. 83/2020-21 Preliminary Test held on 08-07-2021 Question No. 001 – 200 (Concern Subject) Publish Date 09-07-2021 Last Date to Send Suggestion(s) 16-07-2021 THE LINK FOR ONLINE OBJECTION SYSTEM WILL START FROM 10-07-2021; 04:00 PM ONWARDS Instructions / ૂચના Candidate must ensure compliance to the instructions mentioned below, else objections shall not be considered: - (1) All the suggestion should be submitted through ONLINE OBJECTION SUBMISSION SYSTEM only. Physical submission of suggestions will not be considered. (2) Question wise suggestion to be submitted in the prescribed format (proforma) published on the website / online objection submission system. (3) All suggestions are to be submitted with reference to the Master Question Paper with provisional answer key (Master Question Paper), published herewith on the website / online objection submission system. Objections should be sent referring to the Question, Question No. & options of the Master Question Paper. (4) Suggestions regarding question nos. and options other than provisional answer key (Master Question Paper) shall not be considered. (5) Objections and answers suggested by the candidate should be in compliance with the responses given by him in his answer sheet. Objections shall not be considered, in case, if responses given in the answer sheet /response sheet and submitted suggestions are differed. (6) Objection for each question should be made on separate sheet. Objection for more than one question in single sheet shall not be considered. ઉમેદવાર નીચેની ૂચનાઓું પાલન કરવાની તકદાર રાખવી, અયથા વાંધા- ૂચન ગે કરલ રૂઆતો યાને લેવાશે નહ (1) ઉમેદવાર વાંધાં- ૂચનો ફત ઓનલાઈન ઓશન સબમીશન સીટમ ારા જ સબમીટ કરવાના રહશે. -

Reduction of Subacute Uterine Inversion by Haultain's Method: A
This open-access article is distributed under Creative Commons licence CC-BY-NC 4.0. CASE REPORT Reduction of subacute uterine inversion by Haultain’s method: A case report E Ziki,1 MB ChB, MMed; S Madombi,1 MB ChB; C Chidhakwa,1 FCOG; M G Madziyire,1 MMed; N Zakazaka,2 MMed 1 Department of Obstetrics and Gynaecology, University of Zimbabwe, College of Health Sciences, Harare, Zimbabwe 2 Department of Obstetrics and Gynaecology, Parirenyatwa Central Hospital, Harare, Zimbabwe Corresponding author: E Ziki ([email protected]) Uterine inversion is a rare but potentially life-threatening obstetric emergency of unknown aetiology, which is often associated with inadvertent traction on the umbilical cord before separation of the placenta. Here we report a case of a 26-year-old woman who presented with a day’s history of uterine inversion after an attempt to remove a retained placenta following a second-trimester miscarriage. Reduction was attempted in casualty without success and she was taken to theatre for surgical reduction under anaesthesia. Reduction was eventually achieved using the Haultain method. S Afr J Obstet Gynaecol 2017;23(3):78-79. DOI:10.7196/SAJOG.2017.v23i3.1274 Uterine inversion is defined as the ‘turning inside out of the fundus of subacute uterine inversion was made and resuscitation was into the uterine cavity’ and the incidence is about 1 in 3 737.[1] performed using ringer’s lactate fluid and 4 units of packed red Active management of the third stage of labour resulted in a 4.4- blood cells. She was commenced on intravenous antibiotics.