Vocs) in Residential Indoor Environment Using the Canadian Health Measures Survey (Cycle 2: 2009-2011) and a Multiple Receptors Based Approach
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Biomass Burning Emissions and Potential Air Quality Impacts of Volatile Organic Compounds and Other Trace Gases from Temperate Fuels Common in the United States
University of Montana ScholarWorks at University of Montana Chemistry and Biochemistry Faculty Publications Chemistry and Biochemistry 8-12-2015 Biomass burning emissions and potential air quality impacts of volatile organic compounds and other trace gases from temperate fuels common in the United States J. B. Gilman University of Colorado Boulder B. M. Lerner University of Colorado Boulder W. C. Kuster University of Colorado Boulder P. D. Goldan University of Colorado Boulder C. Warneke University of Colorado Boulder Follow this and additional works at: https://scholarworks.umt.edu/chem_pubs See next page for additional authors Part of the Biochemistry Commons, and the Chemistry Commons Let us know how access to this document benefits ou.y Recommended Citation Gilman, J. B.; Lerner, B. M.; Kuster, W. C.; Goldan, P. D.; Warneke, C.; Veres, P. R.; Roberts, J. M.; de Gouw, J. A.; Burling, I. R.; and Yokelson, Robert, "Biomass burning emissions and potential air quality impacts of volatile organic compounds and other trace gases from temperate fuels common in the United States" (2015). Chemistry and Biochemistry Faculty Publications. 89. https://scholarworks.umt.edu/chem_pubs/89 This Article is brought to you for free and open access by the Chemistry and Biochemistry at ScholarWorks at University of Montana. It has been accepted for inclusion in Chemistry and Biochemistry Faculty Publications by an authorized administrator of ScholarWorks at University of Montana. For more information, please contact [email protected]. Authors J. B. Gilman, B. M. Lerner, W. C. Kuster, P. D. Goldan, C. Warneke, P. R. Veres, J. M. Roberts, J. A. de Gouw, I. -

Ventilation in Residential Buildings Indoor Air Quality
Ventilation in residential buildings Indoor air quality Blanca Beato Arribas Senior Research Engineer BSRIA 1 Making buildings better Index • IAQ • Ventilation • Guidelines/Legislation • Exposure limits • What affects indoor air quality at home? • How to measure contaminants 2 Making buildings better Indoor Air Quality Good IAQ : “air with no known contaminants at harmful concentrations” (CIBSE) 3 Making buildings better Ventilation Ventilation is needed to: Good IAQ requires: • Provide fresh air • Low external pollution • Remove pollutants in concentrations a space • Low pollutant • Remove odours emission rates from • Remove heat loads internal sources, including materials • Control humidity • Ventilation: dilute and remove pollutants • Effective ventilation 4 Making buildings better Legislation Regulation or standard Area covered Requirements Size of opening areas for background ventilation and Building regulations Part F1 Provision of adequate fresh air rapid ventilation. Particular extract ventilation rates from kitchens, toilets, etc. Provide adequate air for Building regulations Part J1 combustion devices EH40/2005 Workplace exposure limits Provide adequate fresh air, Limit exposure to various pollutants (HSE) filtration Ensure minimal contamination of HSE Approved Code of Practice L24: Regular maintenance of mechanical systems, including air Workplace health, safety and welfare systems conditioning systems. Air quality guidelines for Europe (WHO, Provide adequate fresh air, Limit exposure to various pollutants 2000) filtration 5 Making buildings better Source:CIBSE Legislation Regulation or standard Area covered Requirements Ambient air and cleaner air Limit exposure to SO and for Europe (EEC Directive 2 suspended particulates 2008/50/EC/2008) BS EN 13986:2002 (Emissions from) wood panels (Emissions from) glued laminated BS EN 14080:2005 timber Selection of materials with low emissions. -

Vapor Intrusion? Can You Get Sick from Vapor Vapor Intrusion Refers to the Vapors Produced by a Chemical Intrusion? Spill/Leak That Make Their Way Into Indoor Air
Bureau of Environmental Health Health Assessment Section VVaappoorr IInnttrruussiioonn “To protect and improve the health of all Ohioans” Answers to Frequently Asked Health Questions What is vapor intrusion? Can you get sick from vapor Vapor intrusion refers to the vapors produced by a chemical intrusion? spill/leak that make their way into indoor air. When intrusion? You can get sick from breathing harmful chemical chemicals are spilled on the ground or leak from an vapors. But getting sick will depend on: underground storage tank, they will seep into the soils and How much you were exposed to (dose). will sometimes make their way into the groundwater How long you were exposed (duration). (underground drinking water). There are a group of How often you were exposed (frequency). chemicals called volatile organic compounds (VOCs) that How toxic the spill/leak chemicals are. easily produce vapors. These vapors can travel through General Health, age, lifestyle: Young children, the soils, especially if the soils are sandy and loose or have a lot elderly and people with chronic (on-going) health of cracks (fissures). These vapors can then enter a home problems are more at risk to chemical exposures. through cracks in the foundation or into a basement with a dirt floor or concrete slab. VOC vapors at high levels can cause a strong petroleum or solvent odor and some persons may VOCs and vapors: experience eye and respiratory irritation, headache VOCs can be found in petroleum products such as gasoline and/or nausea (upset stomach). These symptoms or diesel fuels, in solvents used for industrial cleaning and are usually temporary and go away when the person are also used in dry cleaning. -

Fireplaces, Woodstoves, and Clean Air in Pima County
Pima County Department of Environmental Quality 33 N. Stone Avenue, Suite 700 Tucson, AZ 85701 520-724-7400 www.pima.gov/deq January 2016 Fireplaces, Woodstoves, and Clean Air in Pima County Wood burning is of concern in our community because it is not healthy to breathe wood smoke. Smoke is made up of a complex mixture of gases and fine particles produced when wood burns. According to 2002 estimates, there are approximately 70,000 households that burn wood in fireplaces or wood burning stoves within Pima County. The wood burned by these devices emits about 3,100 tons of carbon monoxide (CO) and particulate matter (PM) into our skies annually, in addition to other pollutants and potentially cancer-causing materials. These microscopic particles in wood smoke can be inhaled deep into the respiratory system where they may cause serious health impacts. The combination of altitude, topography, longer nights and cool winters adds to the wood smoke pollution problem in Pima County. On cold nights with little wind, layers of warm air above trap cold air in the valley, forming an inversion. This inversion layer acts like a blanket and keeps smoke and other pollutants close to the ground. These stagnant conditions can last for days and impact the health of our neighbors. Check with your neighbor to see if your fireplace smoke is causing problems with their health. Together, we can spare the air of these harmful pollutants by choosing not to use our fireplaces as much, or by making small changes in our wood-burning practices. Wood Burning Tips Use firewood that has been dried for longer than six months. -

Biomonitoring Aquatic Ecosystem.Pdf
analytica chimica acta 606 (2008) 135–150 available at www.sciencedirect.com journal homepage: www.elsevier.com/locate/aca Review Biomonitoring: An appealing tool for assessment of metal pollution in the aquatic ecosystem Qunfang Zhou, Jianbin Zhang, Jianjie Fu, Jianbo Shi, Guibin Jiang ∗ State Key Laboratory of Environmental Chemistry and Ecotoxicology, Research Center for Eco-Environmental Sciences, Chinese Academy of Sciences, Beijing 100085, China article info abstract Article history: Wide occurrence of aquatic metal pollution has caused much attention. Biomonitoring Received 17 August 2007 offers an appealing tool for the assessment of metal pollution in aquatic ecosystem. The Received in revised form bioindicators including algae, macrophyte, zooplankton, insect, bivalve mollusks, gastro- 7 November 2007 pod, fish, amphibian and others are enumerated and compared for their advantages and Accepted 7 November 2007 disadvantages in practical biomonitoring of aquatic metal pollution. The common biomon- Published on line 19 November 2007 itoring techniques classified as bioaccumulation, biochemical alterations, morphological and behavior observation, population- and community-level approaches and modeling are Keywords: discussed. The potential applications of biomonitoring are proposed to mainly include Biomonitoring evaluation of actual aquatic metal pollution, bioremediation, toxicology prediction and Metal pollution researches on toxicological mechanism. Further perspectives are made for the biomoni- Aquatic ecosystem toring of metal -

Fast Facts (PDF)
FAST FACTS According to the National Fire Protection Association, the leading factor contributing to home heating fires (30%) was mainly due to having a dirty chimney (i.e., creosote buildup). Heating equipment (including wood stoves) is the second leading cause of home fires, and third leading cause of home fire deaths. Most fireplace and chimney fires are caused by creosote buildup, and could be prevented. EPA believes there are approximately 13 million fireplaces, 250,000 hydronic heaters, and 8.5 million wood stoves in use nationwide. Five million (57 percent) of the nation’s wood stoves are older, inefficient devices. EPA estimates that if all of the old wood stoves in the United States were replaced with cleaner- burning hearth appliances, an estimated $56-126 billion in health benefits per year would be realized. Smoke from wood-burning stoves and fireplaces contain a mixture of harmful gases and particle matter (PM2.5). Breathing these small particles can cause asthma attacks and severe bronchitis, aggravate heart and lung disease, and may increase the likelihood of respiratory illnesses. Changing out one old dirty, inefficient wood stove is equivalent to the PM2.5 reduction of taking five old diesel trucks off the road. The benefits of replacing old wood stoves and fireplaces: • Saves money, fuel, time, and resources • Up to 50 percent more energy efficient, uses 1/3 less wood • Cuts creosote build-up in chimneys that helps reduce the risk of fire • Reduces PM2.5 indoors and out After start-up, a properly installed, correctly used EPA-certified wood stove should be smoke free. -

Biomonitoring a Best Practices Report for State Legislators
Biomonitoring A Best Practices Report for State Legislators BIOMONITORING A BEST PR A CTICES RE P ORT FOR ST A TE LEGIS la TORS By Scott Hendrick Doug Farquhar William T. Pound, Executive Director 7700 East First Place Denver, CO 80230 (303) 364-7700 444 North Capitol Street, N.W., Suite 515 Washington, D.C. 20001 (202) 624-5400 www.ncsl.org May 2010 The National Conference of State Legislatures is the bipartisan organization that serves the legislators and staffs of the states, commonwealths and territories. NCSL provides research, technical assistance and opportunities for policymakers to exchange ideas on the most pressing state issues and is an effective and respected advocate for the inter- ests of the states in the American federal system. Its objectives are: • To improve the quality and effectiveness of state legislatures. • To promote policy innovation and communication among state legislatures. • To ensure state legislatures a strong, cohesive voice in the federal system. The Conference operates from offices in Denver, Colorado, and Washington, D.C. This publication was developed with support from the Centers for Disease Control and Pre- vention and the Association of Public Health Laboratories. NCSL graciously acknowledges their support. This publication was supported by the Association of Public Health Laboratories and Cooperative Agreement Number #U60/CD303019 from Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC. Printed on recycled paper © 2010 by the National Conference of State Legislatures. All rights reserved. ISBN 1-978-58124-596-8 Biomonitoring iii CONTENTS About the Authors.................................................................................................................................... -

AP-42, Vol. I, CH1.9: Residential Fireplaces
1.9 Residential Fireplaces 1.9.1 Generall-2 Fireplaces are used primarily for aesthetic effects and secondarily as supplemental heating sources in houses and other dwellings. Wood is the most common fuel for fireplaces, but coal and densified wood "logs" may also be burned. The user intermittently adds fuel to the fire by hand. Fireplaces can be divided into 2 broad categories: (1) masonry (generally brick and/or stone, assembled on site, and integral to a structure) and (2) prefabricated (usually metal, installed on site as a package with appropriate duct work). Masonry fireplaces typically have large fixed openings to the fire bed and have dampers above the combustion area in the chimney to limit room air and heat losses when the fireplace is not being used. Some masonry fireplaces are designed or retrofitted with doors and louvers to reduce the intake of combustion air during use. Prefabricated fireplaces are commonly equipped with louvers and glass doors to reduce the intake of combustion air, and some are surrounded by ducts through which floor level air is drawn by natural convection, heated, and returned to the room. Many varieties of prefabricated fireplaces are now available on the market. One general class is the freestanding fireplace, the most common of which consists of an inverted sheet metal funnel and stovepipe directly above the fire bed. Another class is the "zero clearance" fireplace, an iron or heavy-gauge steel firebox lined inside with firebrick and surrounded by multiple steel walls with spaces for air circulation. Some zero clearance fireplaces can be inserted into existing masonry fireplace openings, and thus are sometimes called "inserts". -
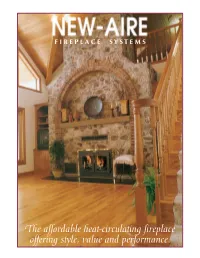
The Affordable Heat-Circulating Fireplace Offering Style, Value and Performance. After a Hard Day in a Cold World…
F I R E P L A C E S Y S T E M S The affordable heat-circulating fireplace offering style, value and performance. After a Hard Day in a Cold World… The NEW-AIRE FIREPLACE SYSTEM utilizes the basic principles of thermodynamics designed into any new high-efficient forced air furnace (radiant, conductive and convective heat transfer). By forcing air movement through a series of baffles in a specifically designed heat exchanger surrounding a steel firebox, ratings in excess of 200,000 BTU can be achieved in a full-fired condition. With 1050 cubic feet of air per minute at central HVAC static pressures, the NEW-AIRE fireplace easily matches the heat output of any high-efficiency furnace on the market today. Your home is the heart of your family’s life. A warm hearth is the gathering place that defines the spirit of the home. The NEW-AIRE fireplace, clad in brass and glass, provides both the traditional and functional elements needed in today’s life. Unlike stoves and inserts, the NEW-AIRE can be independently ducted to provide whole-house heating beyond the walls of the room in which it is installed. Certified to the International Mechanical Code, when ducted to induce heat into the central heating system, the NEW-AIRE SYSTEM efficiently provides the required heat for 4000 plus square foot homes. The NEW-AI Airtight /Airwash Door Control: heat loss, wood consumption, and smoke in the winter — air infiltration and ash smell in the summer. Makes any fireplace more efficient by controlling the “burn rate”. -

Biomonitoring of Lead and Cadmium Preliminary Study on the Added Value for Human Exposure and Effect Assessment
Biomonitoring of lead and cadmium Preliminary study on the added value for human exposure and effect assessment RIVM Letter report 2016-0215 B. Tiesjema │ M. Mengelers Biomonitoring of lead and cadmium Preliminary study on the added value for human exposure and effect assessment RIVM Letter report 2016-0215 B. Tiesjema│M. Mengelers RIVM Letter report 2016-0215 Colophon © RIVM 2017 Parts of this publication may be reproduced, provided acknowledgement is given to: National Institute for Public Health and the Environment, along with the title and year of publication. B. Tiesjema (author), RIVM M. Mengelers (author), RIVM Contact: [email protected] This investigation has been performed by order and for the account of the Netherlands Food and Consumer Product Safety Authority (NVWA), Office for Risk Assessment and Research, within the framework of the project ‘Indicators for human body burden’, research question 9.1.62. This is a publication of: National Institute for Public Health and the Environment P.O. Box 1 | 3720 BA Bilthoven The Netherlands www.rivm.nl/en Page 2 of 49 RIVM Letter report 2016-0215 Synopsis Biomonitoring of lead and cadmium Preliminary study on the added value for human exposure and effect assessment People are exposed to all kinds of substances (for example via food) , which can be harmful to their health. To accurately estimate the health effects, it is important to determine to what extent these substances actually harm the body. In order to do so it may be helpful to measure concentrations of these substances in body fluids and/or tissues (biomonitoring). RIVM chose the substances lead and cadmium to investigate to what extent such measurements show a relationship with the exposure as well as the health effects of these substances. -

Residential Wood Combustionš PM2.5 Emissions
Residential Wood Combustion— PM2.5 Emissions Prepared by: James E. Houck and Paul E. Tiegs OMNI Environmental Services, Inc. 5465 SW Western Avenue Beaverton, Oregon 97005 Prepared for: WESTAR PM2.5 Emission Inventory Workshop Reno, Nevada July 22-23, 1998 1 Residential Wood Combustion — PM2.5 Emissions Table of Contents 1. Description of Appliances and Fuels 1.1 Woodstoves and Heaters 1.2 Fireplaces 1.3 Fuel Characteristics 2. Current Home Heating Status 2.1 Space Heating by Fuel Type 2.2 Old versus New Technology Wood Stoves/Heaters 2.3 Aesthetic and Heating Uses of Fireplaces 2.4 Regional and HDD data 3. Physical and Chemical Characterization of Wood Smoke 4. PM2.5 Emissions Units 5. Emission Inventories 5.1 Emission Factors 5.2 Surveys 6. Tracers and Modeling 6.1 RWC Tracers 6.2 Chemical Mass Balance Modeling 6.3 Correlations with CO and Nephelometer Data 7. SIP Implications 7.1 Emission Reductions with New Appliances and Fuels 7.2 Economics of New Appliances and Fuels 2 Woodstoves and Heaters C Conventional Woodstoves 40 year lifetime 8.3 million in use or about 90% of total C Certified Noncatalytic Woodstoves 0.6 million in use Phase II, July 1990, 7.5 g/hr, 119 models C Certified Catalytic Woodstoves 0.4 million in use Phase II, 4.1g/hr, 83 models Durability, maintenance program C Certified and Exempt Pellet Stoves 0.3 million in use 5 certified models 35 to 1 air- to-fuel ratio (low burn rate) Suspected lower PM2.5 to total ratio C Masonry Heaters Higher cost, few in use, exempt from EPA certification High burn rate, lower emissions -

City of Topeka Licensed Contractors As of 4/16/2021
City of Topeka Licensed Contractors as of 4/16/2021 Mechamical Contractor PHONE_WORK 4 ECO SERVICES 816-241-2112 Mechamical Contractor A & J SHEET METAL HEAT & AIR LLC 620-277-6268 Mechamical Contractor A & S MECHANICAL HEATING & COOLING LLC Mechamical Contractor A-1 APPLIANCE 785-862-2149 Mechamical Contractor AA AIR HEATING & COOLING 660-856-3089 Mechamical Contractor AARONS AIR COND SERV INC 785-654-3601 Mechamical Contractor ABRAHAM MECHANICAL LLC 816-861-0866 Mechamical Contractor ACE PLUMBING CO INC 785.234.3384 Mechamical Contractor ADVANTAGE HEATING & AIR CONDITIONING INC 785-842-6996 Mechamical Contractor AIR CARE HEATING & COOLING 913-362-5274 Mechamical Contractor AIR CONTROL LLC 913-426-1406 Mechamical Contractor AIR TECH SP 785-783-8030 Mechamical Contractor ALL CLIMATE REFRIGERATION LLC 816-795-3700 Mechamical Contractor ALTERNATIVE AIR LLC 785-410-2530 Mechamical Contractor ANDYS REFRIGERATION LLC 785-379-9237 Mechamical Contractor ARIES HOLDING LLC DBA CMS/NEXTECH 321-473-0435 Mechamical Contractor ARNOLDS REFRIGERATION INC 785-364-4700 Mechamical Contractor AUTOMATED CONTROL SYSTEMS CORP 913-248-8828 Mechamical Contractor BARRINGTON HEATING & AIR LLC Mechamical Contractor BILLS PLUMBING & HEATING INC 785-636-5377 Mechamical Contractor BOB HAMILTON PLUMBING, HEATING & A/C 913-888-4262 Mechamical Contractor BOYETT HEATING & COOLING LLC Mechamical Contractor BRANDONS HEATING & AIR 785-893-1349 Mechamical Contractor BRISCOE AIR & HEATING 913-980-9889 Mechamical Contractor C & K CONSTRUCTION 785-210-5546 Mechamical Contractor