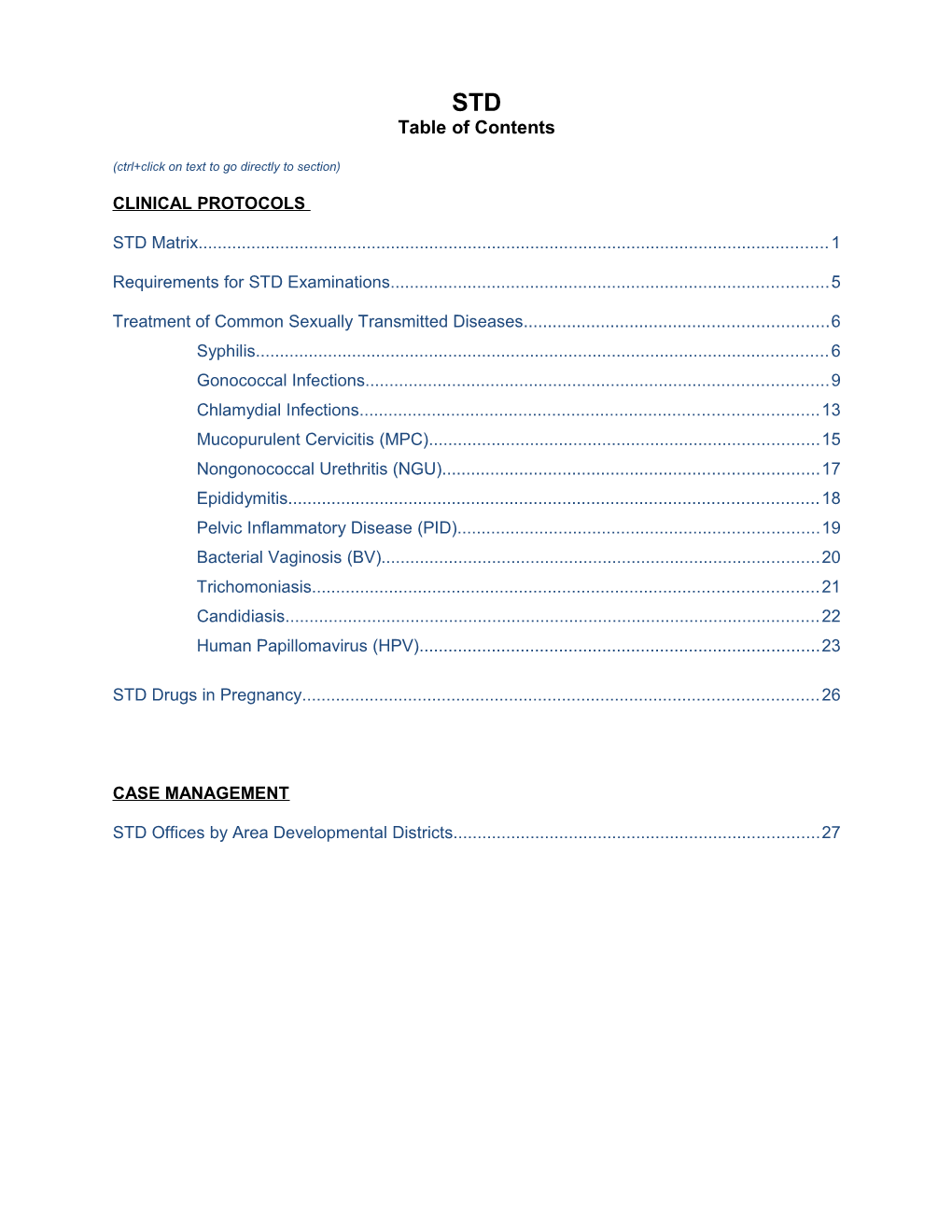
STD Table of Contents
(ctrl+click on text to go directly to section)
CLINICAL PROTOCOLS
STD Matrix...... 1
Requirements for STD Examinations...... 5
Treatment of Common Sexually Transmitted Diseases...... 6 Syphilis...... 6 Gonococcal Infections...... 9 Chlamydial Infections...... 13 Mucopurulent Cervicitis (MPC)...... 15 Nongonococcal Urethritis (NGU)...... 17 Epididymitis...... 18 Pelvic Inflammatory Disease (PID)...... 19 Bacterial Vaginosis (BV)...... 20 Trichomoniasis...... 21 Candidiasis...... 22 Human Papillomavirus (HPV)...... 23
STD Drugs in Pregnancy...... 26
CASE MANAGEMENT
STD Offices by Area Developmental Districts...... 27 STD MATRIX
STD VISIT (Primary reason for visit is due to symptoms, exposure, STD RE-VISIT partner problem, positive test and/or high risk Requirements of an STD Visit behavior) Males and Females Males and Females PRIMARY REASON: Positive Test Positive Test Symptoms – (list symptom and duration) Symptoms – ( for STD symptom and duration) Results Symptomatic Partner Follow-up appointment Exposure (list STD) Other REASON FOR STD test only HIV test only VISIT Referral (list agency) For all other clinical visits (i.e. Family planning, Adult/Child Prevention, Cancer, etc.), lab testing for STD screening does not require an STD physical exam unless STD symptoms are reported.
Significant illnesses; hospitalizations; chronic or acute Identify any changes to the medical history medical conditions obtained during the prior visit including MEDICAL Allergies allergies, prescriptions and/or antibiotics Current prescription medication and/or antibiotics w/in HISTORY the last month HX of STD/HIV (list condition, date, and place of RX) Sex with males, females or both Sexual exposure since last visit Number of partners w/in 12 mos Identify any changes to the sexual & Number of partners w/in 60 days reproductive history obtained during the prior Number of new partners w/in 60 days visit. Date of last sexual exposure (LSE) Anatomical sites exposed during sexual activity
Exposed < 60 < 12 Sites days mns SEXUAL & REPRODUCTIV Vagina E HISTORY Anus Mouth Penis
Frequency of condom usage FEMALES: Last menstrual period, obstetrical history, and gynecological conditions, and current contraceptive use.
RISK Suggested Questions to Ask During Identify any changes since last visit ASSESSMENT The Sexual History When was the last time you had sex? How many partners have you had sex with in the last 12 months? How many new partners have you had sex with in the last 2 months? When is the last time you had sex with a man? Woman? Both? At what age did you become sexually active? What are you doing to prevent pregnancy? Did you use a barrier the last time you had sex? How often do you use a barrier when you have sex? When is the last time you engaged in oral, anal, or vaginal intercourse? Are you the insertive partner, the receptive partner, or both?
Was the sexual encounter consensual or nonconsensual?
Page 2 of 27 Core Clinical Service Guide Section: STD September 1, 2012 STD VISIT (Primary reason for visit is due to symptoms, exposure, STD RE-VISIT partner problem, positive test and/or high risk Requirements of an STD Visit behavior) Males and Females Males and Females Have you ever been paid for sex (exchanged sex for drugs or exchanged sex for money)? Have you ever been a resident in a correctional facility? Do you have a history of sexually transmitted diseases? Has your judgment ever been impaired by the use of alcohol or drugs?
STD/HIV exposure Substance abuse including IV drug use and alcohol Multiple partners Anonymous partners Sex for money or drugs Abuse or domestic violence
PHYSICAL ALL: 5. Repeat physical exam per medical/sexual EXAM Oral examination. history and risk assessment Skin inspection over entire body, especially the lower abdomen, inguinal areas, thighs, hands, palms, and forearms. Inspection of the pubic hair for lice and nits. Inspect external genitalia, perineum, and anus. Palpate for lymphadenopathy, especially the inguinal and femoral regions.
FEMALES: The examination for STD’S should not be deferred for menses unless bleeding is extremely heavy. Urine specimen can be collected for CT/GC testing.
A pregnant patient should be examined and tested in the same manner as the non-pregnant patient with the exception of the bimanual pelvic exam. If a pregnant patient is experiencing vaginal bleeding she should be immediately referred to her obstetrician or certified nurse midwife. Examine the vagina and the cervix, using the appropriate speculum. It is highly recommended that a specimen be obtained from the vaginal vault for a wet mount. Obtain an endocervical specimen for gonorrhea and Chlamydia utilizing an APTIMA test kit. A urine specimen should be obtained from females without a cervix. Obtain specimens for gonorrhea from other exposure sites as indicated i.e. throat, rectum Perform a Bimanual pelvic examination. A bimanual exam is to be performed on all females presenting for STD evaluation with the exception of pregnancy and hysterectomy. Recommend women complaining of rectal symptoms to have an anoscopic exam at their primary care provider or an appropriate specialist.
MALES: Inspect scrotum and palpate scrotal contents; inspect rectal area (perineum & anus) if patient has had male- male sex.
Page 3 of 27 Core Clinical Service Guide Section: STD September 1, 2012 STD VISIT (Primary reason for visit is due to symptoms, exposure, STD RE-VISIT partner problem, positive test and/or high risk Requirements of an STD Visit behavior) Males and Females Males and Females Inspect and palpate penis, retract foreskin, and inspect urethra. Using APTIMA Test Kits, obtain intraurethral specimens for gonorrhea and Chlamydia testing and Gram staining if available. If patient is asymptomatic and has not urinated for one hour, may obtain first-catch urine specimen for gonorrhea and Chlamydia. Obtain specimens for gonorrhea from other exposure sites as indicated, i.e. throat, rectum Recommend men complaining of rectal symptoms to have an anoscopic exam at their primary care provider or an appropriate specialist.
Note: Repeat labs per medical/sexual history and risk LABORATORY Routine laboratory tests shall be obtained at each STD assessment. visit. An STD visit is defined as a visit in which the (Note: Testing for Chlamydia less than 3 weeks patient presents with new symptoms, new exposure, from date of treatment may result in a positive partner problem, positive test and/or high risk behavior. result which may represent nonviable Chlamydia remnants from an earlier infection) Obtain blood specimens from all patients for VDRL (Venereal Disease Research Laboratory) or RPR (Rapid Plasma Reagin) at each visit except for those patients who have had a documented non-reactive VDRL within the past 30 days. Patients presenting with symptoms suggestive of syphilis or who are epidemiologically related to another person with syphilis should have a syphilis test regardless of documentation of testing within the last 30 days. For patients presenting with lesion(s) suggestive of syphilis, a confirmatory test should be requested. Confirmatory tests for syphilis are IGG, TPPA and FTA. Obtain specimen for Chlamydia (CT/GC APTIMA Test) Except in pregnant women, a test of cure is not recommended for persons treated with the recommended or alternative regimens, unless therapeutic compliance is in question symptoms persist, or re-infection is suspected. Testing in less than 3 weeks after completion of therapy could yield a false positive result due to the presence of dead CT organisms. Obtain specimen for Gonorrhea (CT/GC APTIMA Test) Test of cure is not recommended routinely for patients with uncomplicated gonorrhea who have been treated with the recommended regimens. Patients with persistent symptoms or whose symptoms recur shortly after treatment should be reevaluated by culture; positive isolates should undergo antimicrobial susceptibility testing. Obtain blood specimens for HIV testing from all patients seeking STD services except for those patients who have a documented negative HIV test within the past 90 days or if the patient declines.
Page 4 of 27 Core Clinical Service Guide Section: STD September 1, 2012 STD VISIT (Primary reason for visit is due to symptoms, exposure, STD RE-VISIT partner problem, positive test and/or high risk Requirements of an STD Visit behavior) Males and Females Males and Females Stat Testing (Dependent upon availability at the LHD) Stat RPRs for syphilis, if available, should be ordered on patients with ANY of the following: Genital lesion(s) Rash suggestive of syphilis Epidemiological link to another person with syphilis History of lesions or lymphadenopathy since last negative serologic test for syphilis (STS).
If stat RPR is not available and the patient has a lesion(s,),obtain a blood specimen for VDRL or RPR plus request confirmatory testing such as IGG, TPPA or FTA (a negative VDRL or RPR with clinical symptoms suggestive of primary syphilis such as a lesion(s) does not rule out syphilis – confirmatory testing is required)
Gram stain for gonorrhea, if available, should be ordered on male patients who present with ANY of the following: Penile Discharge Dysuria
Treatment as indicated in this guide or CDC Treatment Guidelines. As assessed for individual patient needs. Recommendation/Referral for other health care needs or to a higher level provider if needed. Recommendation/Referral for social services (as needed) Linkage for partner services (contact STD regional area to initiate partner services if patient is diagnosed with PROVIDE syphilis and/or HIV. Follow up appointment (as needed) Condoms Priority consideration in regards to patient flow should be given to patients who are known to be infected with an STD or is an epidemiological link to an individual known to be infected.
Counseling messages should include: As assessed for individual patient needs. Take medication as directed. Abstain from sex until the patient and patient’s sex partners have completed treatment. Abstinence should be continued until 7 days after a single-dose regimen or after completion of a muti-dose regimen. Return for all follow-up appointments. COUNSELING How to obtain test results. Safe sex, risk reduction messages. Pregnancy prevention. Provide partner services to individuals diagnosed with Chlamydia, gonorrhea, NGU or MPC.
Educational materials can be located at: http://www.cdc.gov/std/products/default.htm
REQUIREMENTS FOR STD EXAMINATIONS
Page 5 of 27 Core Clinical Service Guide Section: STD September 1, 2012 Page 6 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES
RECOMMENDED CONDITION SYMPTOMS TESTS ALTERNATIVES PARTNER SERVICES REPORTING TREATMENT
SYPHILIS (see 2010 CDC guidelines for follow-up recommendations and management of congenital syphilis)
PRIMARY (1º), PRIMARY(1º): Indurated VDRL/RPR BENZATHINE (For penicillin Contact STD Supervisor Complete SECONDARY (2º) chancre usually PENICILLIN G allergic within your regional area EPID 200 and OR painless IGG or TPPA 2.4 million units non-pregnant within 24 hours to fax to State EARLY LATENT SECONDARY (2º) or FTA, or (MU) IM in a single adult patients) initiate partner services STD Program (<1 YEAR) Rash - bilateral macular, MHA dose for index patient. within 24 Adults papular, follicular, DOXYCYCLINE hours. papulosquamous or Stat RPR and 100 mg orally All Sex partners exposed pustular lesions. Dark Field is Symptomatic men & 2 times a day to any stage of syphilis in Alopecia , Condylomata desired if women shall be for 14 days the previous 90 days lata, Mucous Patches primary or treated empirically on should be examined, EARLY LATENT secondary SX their initial visit. OR tested and preventively treated for syphilis on their No Symptoms (SX) at are present Exam CEFTRIAXONE 1 initial visit. Partners shall PLUS one of the following: 1 g daily IV or IM be screened for History (HX) of SX within for 10-14 days. gonorrhea, Chlamydia and (w/in) last 12 months (please see footnote HIV. Sexual partners Documented Negative below) This beyond 90 days shall be test w/in last 12 months recommendation is examined and screened Epidemiological link to based on limited another infected studies. Therefore, for syphilis, HIV, individual the optimal dose and gonorrhea, and duration of Chlamydia. ceftriaxone therapy have not been defined. Children Same as Adult Same as Adult Benzathine penicillin G Infants and Contact STD Supervisor Same as Adult Primary, Secondary Plus 50,000 units/kg IM, up children who are within your regional area Plus or Early Latent CSF to the adult dose of allergic to > 12 years of age. Report (aged > 1 month) 2.4 MU in a single dose Examination penicillin should suspected cases See CDC Treatment Generally, RX for STDs be desensitized of sexual abuse Guidelines for the found in a pre-pubertal child and then treated to the Dept of should be managed by the management of with penicillin Community child’s physician. LHDs congenital syphilis shall assure adequate RX. Based Services
Page 7 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES
PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
RECOMMENDED CONDITION SYMPTOMS TESTS ALTERNATIVES PARTNER SERVICES REPORTING TREATMENT
SYPHILIS (see 2010 CDC guidelines for follow-up recommendations and management of congenital syphilis) LATE LATENT None VDRL/RPR Benzathine (For penicillin Contact STD Supervisor Complete (>1 penicillin G allergic non- within your regional EPID 200 and YEA IGG or TPPA 2.4 million units IM pregnant adult area. fax to State R) or FTA, or for 3 doses, 1 week patients) STD Program. OR MHA apart (total: LAT 7.2 million units) DOXYCYCLINE ENT See CDC 100 mg orally OF Treatment 2 times a day UN Guidelines to for 28days (for KN determine if CSF adults only) OW exam is needed N DU RAT ION
Adults
Children Same as Adult Same as Adult Benzathine Infants and Contact STD Supervisor Same as Adult Late Latent or Latent of Plus penicillin G 50,000 children who are within your regional area Plus Unknown Duration CSF units/kg IM up to allergic to > 12 years of age. (aged > 1 month) Examination the adult dose of penicillin should Report See CDC Treatment 2.4 million units, be desensitized suspected cases Guidelines for the administered for and then treated of sexual abuse management of three doses at with penicillin to the Dept of congenital syphilis 1 week intervals Community Based Services Generally, RX for STDs (total 150,000 units/kg found in a pre-pubertal up to the adult total child should be managed dose of 7.2 million
Page 8 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES by the child’s physician. units) LHDs shall assure adequate RX. NEUROSYPHILIS Neurologic or CSF Aqueous crystalline Procaine penicillin Contact STD Supervisor Complete ophthalmic Examination penicillin G 18-24 2.4 million units IM within your regional EPID 200 and abnormalities million units per day, once daily for 10- area. fax to State administered as 3-4 14 days plus STD Program. probenecid 500 mg million units IV every orally 4 times a 4 hours or continuous day for 10-14 days infusion, for 10-14 days PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
RECOMMENDED CONDITION SYMPTOMS TESTS ALTERNATIVES PARTNER SERVICES REPORTING TREATMENT
SYPHILIS (see 2006 CDC guidelines for follow-up recommendations and management of congenital syphilis)
SYPHILIS WITH A SEE ABOVE SEE ABOVE For 1º, 2º and early The use of any Contact STD Supervisor Notify CO-INFECTION latent syphilis: Treat alternative within your regional area HIV/AIDS OF HIV as above. Additional therapy in HIV if index patient is co- surveillance if doses of Benzathine infected infected w/HIV to initiate newly penicillin G in early persons has partner services. diagnosed HIV syphilis do not not been well case. enhance efficacy, studied; regardless of HIV therefore the status. use of For late latent doxycycline syphilis or latent and ceftriaxone syphilis of unknown must be duration: Perform undertaken CSF exam to with caution rule-out neurosyphilis
Page 9 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES
SYPHILIS AND SEE ABOVE SEE ABOVE Penicillin is the only N/A Contact STD Supervisor Complete PREGNANCY recommended within your regional area EPID 200 and treatment for syphilis within 24 hours of fax to State during pregnancy. laboratory receipt. STD Program Women who are within 24 allergic should be hours. desensitized and then Indicate treated with penicillin. pregnancy Dosages are the same status on as in non-pregnant EPID 200. patients for each stage of syphilis.2
Page 10 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued) RECOMMENDED CONDITION SYMPTOMS TESTS ALTERNATIVES PARTNER SERVICES REPORTING TREATMENT
GONOCOCCAL INFECTIONS Also treat for Chlamydial infection if not ruled out by a sensitive test such as a nucleic acid amplification test.
GC - ADULTS Female- MALE & Symptomatic men & Azithromycin Sex partners Complete Often FEMALE: women presenting 2gm orally in a exposed during the EPID 200 and fax asymptomatic. APTIMA CT/GC for an STD visit single dose previous 60 days or mail to State COMBO shall be treated should be examined, STD Program Cervix, OR Urethra, Cervical: (NAATS) empirically for both tested and within 14 days. Rectum Cervical discharge. TEST GC and CT on their Single-dose preventively treated for gonorrhea and EPID 200’s that Also-Increased initial visit. injectible 1 Chlamydia on their do not contain vaginal discharge, APTIMA is not cephalosporin 1 initial visit. They treatment at time bleeding between approved by the Ceftriaxone regimens shall also be of initial report periods and dysuria. FDA for rectal or 250 mg IM in a pharyngeal single dose screened for shall be updated specimens. See 2010 CDC Chlamydia, syphilis with treatment Male- OR Culture is the guidelines for and HIV. information and May be discussion of Cefixime 400 mg sent to state STD asymptomatic. preferred method of orally in a single PLUS office 7 days after detection. dose3 RX administration Urethra: Discharge Adequate (white, yellow or treatment for 85% of patients Male: Gram Chlamydia. green), Dysuria. stain (if test is PLUS diagnosed w/GC alternative regimens should be treated available at Adequate 4 within 14 days Males & Females- LHD) of urethral treatment for Quinolones should Rectal: Pain, itching discharge. Chlamydia . not be used for from the date of discharge, bleeding; treatment of lab collection and gonorrhea may be 90% within asymptomatic. 30 days from the date of lab collection.
Page 11 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued) RECOMMENDED PARTNER CONDITION SYMPTOMS TESTS ALTERNATIVES REPORTING TREATMENT SERVICES GONOCOCCAL INFECTIONS Also treat for Chlamydial infection if not ruled out by a sensitive test such as a nucleic acid amplification test. GC – PHARYNX Sore throat, APTIMA is not Ceftriaxone1 250 mg Ciprofloxacin 4 500 mg SEE ABOVE SEE ABOVE pharyngeal approved by the IM in a single dose orally in a single dose exudate, FDA for rectal or enlarged pharyngeal PLUS specimens. Culture PLUS cervical Adequate is the preferred Adequate lymph nodes; treatment for treatment for often method of Chlamydial Chlamydial detection. infection. asymptomatic. infection. DLS does not (Individuals receiving perform GC alternative regimens for cultures. pharyngeal GC shall have a test of cure 3-5 days after treatment)
GC in SEE GC SX IN Culture is Ceftriaxone1 N/A SEE ABOVE if Complete CHILDREN ADULTS preferred method 125 mg IM once > 12 years of EPID 200 and (<45KG or <100 lbs) of detection age. fax or mail to vagina, cervix, PLUS State STD urethra, DLS lab does not Program within pharynx, rectum Adequate 14 days. perform GC treatment for cultures. Chlamydia. Generally, RX for Report suspected STDs found in a pre- cases of sexual pubertal child should Because of the legal abuse to the Dept be managed by the implications of a child’s physician. of Community diagnosis of N. Based Services LHDs shall assure gonorrhoeae infection in adequate RX. a child, culture is the preferred method. NAATs, however, can be used for vaginal or
Page 12 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued) RECOMMENDED PARTNER CONDITION SYMPTOMS TESTS ALTERNATIVES REPORTING TREATMENT SERVICES GONOCOCCAL INFECTIONS Also treat for Chlamydial infection if not ruled out by a sensitive test such as a nucleic acid amplification test. urine specimens from girls (only).
GC in SEE GC SX IN Culture is preferred Same regimen as Same regimen as SEE ABOVE if Complete CHILDREN ADULTS method of detection recommended for recommended for adults > 12 years of EPID 200 and (>45KG) adults age. fax or mail to DLS lab does not State STD Generally, RX for perform GC Program STDs found in a pre- within 14 pubertal child should cultures. be managed by the Because of the legal days. child’s physician. implications of a LHDs shall assure diagnosis of N. Report adequate RX. gonorrhoeae infection in suspected cases a child, culture is the of sexual abuse preferred method. to the Dept of NAATs, however, can Community be used for vaginal or Based Services urine specimens from girls (only).
Page 13 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued) RECOMMENDED PARTNER CONDITION SYMPTOMS TESTS ALTERNATIVES REPORTING TREATMENT SERVICES GONOCOCCAL INFECTIONS Also treat for Chlamydial infection if not ruled out by a sensitive test such as a nucleic acid amplification test. GC - SEE GC SX IN SEE GC TESTS IN Ceftriaxone 1 250 mg Azithromycin 2 g orally Sex partners Complete PREGNANCY ADULTS ADULTS IM once in a single dose exposed during EPID 200 and (sufficient to treat for the previous fax or mail to OR both GC and CT) 60 days should State STD Cefixime 400 mg be examined, Program within
orally in a single tested and 14 days. dose3 preventively PLUS treated for Indicate PLUS gonorrhea and pregnancy Adequate Chlamydia on status on treatment for Adequate their initial visit. EPID 200 form. treatment for Chlamydial Chlamydial infection (for They shall also infection (for pregnant be screened for pregnant women). Chlamydia, women). syphilis and HIV.
Page 14 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued) RECOMMENDED PARTNER CONDITION SYMPTOMS TESTS ALTERNATIVES REPORTING TREATMENT SERVICES CHLAMYDIAL INFECTIONS
CT - ADULT Men- APTIMA CT/GC Symptomatic men Erythromycin Sex partners Complete EPID 200 Urethral COMBO (NAATS) test and women, base 500 mg exposed during and fax or mail to discharge or presenting for an orally 4 times a the previous State STD Program dysuria; often APTIMA is not STD visit, shall be day for 7 days 60 days should be within 14 days. examined, tested EPID 200’s that do asymptomatic. approved by the FDA treated OR for rectal or empirically for and preventively not contain Erythromycin Women- pharyngeal specimens both CT and GC treated for treatment at time and must be on their initial ethylsuccinate Chlamydia on their of initial report Vaginal/cervical 800 mg orally discharge, confirmed by culture visit. initial visit. They shall be updated at a certified 4 times a day for shall also be with treatment dysuria; often 7 days asymptomatic. laboratory. Azithromycin 1 g screened for information and orally single OR gonorrhea, sent to state STD DLS does not perform dose Ofloxacin4 syphilis and HIV. office 7 days after CT cultures. 300 mg orally RX administration OR 2 times a day for 85% and 90% of Retest men and women Doxycycline 7 days OR patients DX w/CT who have been treated for 100 mg orally 4 Levofloxacin should be treated within Chlamydia whenever they 2 times a day for 500 mg orally 14 and 30 days, seek medical care within 7 days once a day for respectively, from the 3–12 months following date of lab collection. treatment. 7 days CT in CHILDREN SEE CT SX IN Culture is preferred Erythromycin N/A N/A Complete EPID 200 (<45 KG or <100 lbs) ADULTS ABOVE (DLS lab does not base or and fax or mail to perform CT cultures). ethylsuccinate State STD Program Generally, RX for STDs 50 mg/kg/day within 14 days. found in a pre-pubertal orally divided PLUS child should be managed Non-culture, non-amplified by the child’s physician. probe tests for CT should into four doses LHDs shall assure not be used because of the daily for Report suspected adequate RX. possibility of false-positive 14 days6 cases of sexual abuse test results. to the Dept of Community Based Services
Page 15 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued) RECOMMENDED PARTNER CONDITION SYMPTOMS TESTS ALTERNATIVES REPORTING TREATMENT SERVICES CHLAMYDIAL INFECTIONS CT in CHILDREN SEE CT SX IN SEE CT IN CHILDREN Azithromycin 1 g N/A N/A See Above (>45 KG and <8 years ADULTS ABOVE “TESTS” ABOVE orally single dose of age) Generally, RX for STDs found in a pre-pubertal child should be managed by the child’s physician. LHDs shall assure adequate RX.
CT in CHILDREN SEE CT SX IN SEE CT IN CHILDREN Azithromycin 1 g Doxycycline SEE ABOVE if See Above ( > 8 years) ADULTS ABOVE “TESTS” orally single 100 mg orally > 12 years of age. ABOVE dose 2 times a day for 7 days
CT IN PREGNANCY SEE ABOVE SEE ABOVE Azithromycin 1 g Erythromycin Sex partners Complete EPID 200 orally single base 500 mg exposed during and fax or mail to Repeat testing dose orally 4 times a the previous State STD Program (preferably by NAAT) OR day for 7 days 60 days should be within 14 days. 3 weeks after Amoxicillin 500 OR examined, tested completion of therapy is mg orally Erythromycin and preventively Indicate pregnancy recommended for all 3 times a day for 250 mg orally treated for status on EPID 200 pregnant women to 7 days 4 times a day for Chlamydia on their form. ensure therapeutic cure. 14 days OR initial visit. They Erythromycin shall also be ethylsuccinate screened for 800 mg orally gonorrhea, 4 times a day for syphilis and HIV. 7 days OR Erythromycin ethylsuccinate 400 mg 4 times a day for 14 days
Page 16 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
RECOMMENDED CONDITION SYMPTOMS TESTS ALTERNATIVES PARTNER SERVICES REPORTING TREATMENT MPC Mucopurulent Cervicitis
MPC 1. Endocervical APTIMA CT/GC Symptomatic women Azithromycin 1 gm Sex partners MPC is not a Mucopurulent discharge which COMBO presenting for an orally in a single exposed during the reportable Cervicitis may appear (NAATS) test STD visit, shall dose* previous 60 days condition. green or yellow receive empirical should be examined, However if the OR when viewed on treatment for both CT tested, and Chlamydia or a white cotton and GC during their Erythromycin preventively treated gonorrhea test is tipped swab. initial visit. 500 mg orally for gonorrhea and positive, complete 2. Easily induced MPC is a clinical 4 times a day for chlamydia on their the EPID 200 form cervical assessment based on all 7 days initial visit pending and report to state or some of the symptoms lab results of the STD program bleeding listed. (friability, i.e. original patient. They within 14 days. bleeding when Azithromycin 1 g shall also be the first swab is orally single dose screened for syphilis placed in the and HIV. OR *Consider concurrent endocervix. treatment for Doxycycline 100 mg gonococcal infection if orally 2 times a day prevalence of for 7 days gonorrhea is high in the patient population *Consider concurrent under assessment. treatment for gonococcal infection if prevalence of gonorrhea is high in the patient population under assessment.
Page 17 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
RECOMMENDED CONDITION SYMPTOMS TESTS ALTERNATIVES PARTNER SERVICES REPORTING TREATMENT MPC Mucopurulent Cervicitis
MPC in SEE ABOVE SEE ABOVE Azithromycin 1 g Azithromycin 1 gm SEE ABOVE SEE ABOVE PREGNANCY orally single dose orally in a single dose * OR OR Amoxicillin 500 mg orally 3 times a day Erythromycin 500 for 7 days mg orally 4 times a day for 7 days *Consider concurrent treatment for *Consider concurrent gonococcal infection if treatment for prevalence of gonococcal infection if gonorrhea is high in prevalence of the patient population gonorrhea is high in under assessment. the patient population under assessment.
Page 18 of 27 Core Clinical Service Guide Section: STD September 1, 2012
(Continued) PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
CON RECOMMENDED PARTNER DITI SYMPTOMS TESTS ALTERNATIVES REPORTING TREATMENT SERVICES ON NGU Nongonococcal Urethritis
NON- Urethral NGU is a Symptomatic men Erythromycin All persons sexually NGU is not a GON Discharge clinical shall receive base8 500 mg exposed within the reportable OCO (Often early a.m.) assessment empirical treatment orally 4 times a previous 60 days condition. CCAL And Dysuria. based on for both CT and GC day for 7 days OR should be tested However if the URET symptoms. during their initial Erythromycin and preventively Chlamydia or HRITI Discharge can be visit. ethylsuccinate8 treated for gonorrhea test is S mucopurulent, It is best 800 mg orally chlamydia and positive, (NGU purulent or clear. supported by Azithromycin7 1 g 4 times a day for gonorrhea on their complete the ) one type of lab. orally single dose 7 days OR initial visit. Partners EPID 200 form Men Such as a gram OR Ofloxacin4 300 mg shall be screened and report to stain with five (5) Doxycycline orally 2 times a for CT, GC, syphilis state STD Inflammation of or more PMNs 100 mg orally day for 7 days OR and HIV. program within the urethra not per oil immersion 2 times a day for Levofloxacin4 14 days. caused by field with no 7 days 500 mg orally gonorrhea. once a day for Empiric treatment for evidence of partners with a drug Chlamydia gonorrhea. PLUS 7 days regimen effective against trachomatis has chlamydia is Adequate been implicated Submit PLUS recommended for women as the cause of treatment for exposed to NGU APTIMA CT/GC Adequate regardless of whether a NGU in 15% - gonorrhea if COMBO gram stain is treatment for specific etiology is 55% of cases. (NAATS) test identified in the original not available. gonorrhea if patient. Empiric partner gram stain is treatment for gonorrhea not available. may be omitted if ruled out by Gram Stain or NAATS testing in the original patient.
Page 19 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
RECOMMENDED CONDITION SYMPTOMS TESTS ALTERNATIVES PARTNER SERVICES REPORTING TREATMENT EPIDIDYMITIS
Epididymitis9 1. Acute pain Submit CT/GC Ceftriaxone1 Ofloxacin4 All persons sexually Epididymitis is (present for less APTIMA test. 250 mg IM single 300 mg orally exposed within the not a reportable than 7 days) and dose PLUS twice daily for previous 60 days condition. swelling in area Doxycycline 10 days should be tested and However, if the of epididymis 100 mg orally preventively treated Chlamydia or OR (may also involve 2 times a day for for Chlamydia and gonorrhea test is testes). 10 days Levofloxacin4 gonorrhea on their positive, initial visit. Partners complete the 2. Tender swelling, Consult Physician 500 mg orally shall be screened for EPID 200 form infrequently or refer if: once a day for CT, GC, syphilis and and report to accompanied by Any patient with 10 days HIV. state STD redness, usually No. 1 and No. 2 program within unilateral noted listed under 14 days. in the posterior symptoms who is aspect of the 40 yrs of age or scrotum. older. History of 3. Accompanying symptoms urethral present for longer discharge or than 30 days. dysuria. Consider testicular torsion in adolescent without pyuria/white cells on urethral smear with acute onset pain. Note: This is a surgical emergency.
Page 20 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued) RECOMMENDED PARTNER CONDITION SYMPTOMS TESTS ALTERNATIVES REPORTING TREATMENT SERVICES PELVIC INFLAMMATORY DISEASE (PID)
PELVIC 1.Low abdominal Submit CT/GC REGIMEN A REGIMEN B Sexual contacts PID, alone, is INFLAMMATORY pain or painful APTIMA test. Ceftriaxone Ceftriaxone within the not a reportable DISEASE (PID)10 intercourse by 250 mg IM once 250 mg IM once previous 60 days condition. (outpatient patient’s PLUS should be However, if the Perform stat OR management) history. pregnancy test Doxycycline 100 mg evaluated and Chlamydia or Cefoxitin 2 g IM treated for GC gonorrhea test 2.Low abdominal (Although PID is orally 2 times a day These regimens and CT during is positive, tenderness on uncommon in for 14 days once plus to be used with their initial visit. complete EPID bimanual exam. pregnancy, (Doxycycline is probenecid 1 g or without regimens contraindicated in orally once Partners shall 200 form and metronidazole 3.Adnexal appropriate for pregnancy – also be screened report to state OR 500 mg orally tenderness or PID in pregnant Erythromycin 500 mg 4 for syphilis and STD program twice a day for adnexal mass. women may be x daily for 14 days is Other third HIV. within 14 days. 14 days used after appropriate for pregnant generation Mark “PID” box 4.Cervical motion women) as well as the tenderness or physician/ARNP cephalosporin evaluation and appropriate CT pain. Assessment is made OR and/or GC box. concurrence. by identifying 5.Fever and chills Patients should symptoms No. 3 or No. 2 g 6.Nausea and be directed for 4 or both. Azithromycin admission to a vomiting. If symptoms No. 3, 4, hospital) 5, 6 and/or abdominal PLUS rebound tenderness is identified, treat and Doxycycline refer to E.R. 100 mg orally Women w/PID should be re- 2 times a day for evaluated in 3-4 days and 10-14 14 days days after initial visit to re- assess symptoms and RX tolerance. Consult with an upper level provider. If worse, direct the patient to a hospital of her choice.
Page 21 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
PARTNER CONDITION SYMPTOMS TESTS RECOMMENDED TREATMENT ALTERNATIVES REPORTING SERVICES BV Bacterial Vaginosis BACTERIAL 1. Mild to 1.Note character of Metronidazole11 500 mg Tinidazole 2 g orally N/A N/A VAGINOSIS moderate amount vaginal discharge orally 2 times a day for once daily for 2 days (BV) of homogeneous 2.Ensure normal 7 days. chalky white or appearance of OR OR grey-green cervix with discharge; patient speculum exam Metronidazole gel 0.75% Tinidazole 1 g orally may complain of 3.Collect discharge intravaginally once a day once daily for 5 days odor. from lateral wall of for 5 days. 2. Positive vagina OR OR whiff test: fishy 4.Determine vaginal amine odor from pH Clindamycin cream12 2% Clindamycin 300 mg vaginal fluids 5.Perform intravaginally at bedtime for enhanced by 7 days orally 2 times a day for microscopic exam 7 days mixing with 10% of discharge with KOH. 10% KOH to Assessment is made by OR 3. pH of discharge identifying 3 out of the 4 vaginal secretion Clindamycin ovules 100 6.Perform amine or symptoms listed. > 4.5. g intravaginally at whiff test after 4. Clue cells bedtime for 3 days application of 10% on saline wet KOH to discharge mount of vaginal discharge 11 BV11 AND SEE ABOVE SEE ABOVE Metronidazole11 500 mg Metronidazole 250 mg N/A N/A PREGNANCY orally 2 times a day for orally 3 times a day for 7 days 7 days BV in pregnancy has been associated with preterm delivery. OR Metronidazole can be given during Clindamycin 300 mg pregnancy, but avoid repeated orally 2 times a day for 7 dosing. Consult and/or direct days patient to an upper level provider if BV is suspected.
Page 22 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
PARTNER CONDITION SYMPTOMS TESTS RECOMMENDED TREATMENT ALTERNATIVES REPORTING SERVICES Trichomoniasis
Trichomoniasis 1.Frothy grey or SEE Metronidazole11 2 g orally Metronidazole11 Advise females N/A Females yellow-green ABOVE single dose 500 mg orally to have partners vaginal 2 times a day for treated. Male OR discharge 7 days partners shall be 13 2.Pruritus/Itching Tinidazole 2 g orally single screened for CT, dose (not recommended in GC, syphilis and 3.Cervical pregnancy) HIV. Men petechiae exposed to (“strawberry- Usual mode of assessment is Trichomoniasis cervix”) made by observation of motile should be treated trichomonas in saline wet mount. on their initial visit: Consult and/or direct patient to an Metronidazole upper level provider if 2 g orally In a Trichomoniasis is suspected. single dose OR
Tinidazole14 2 g orally single dose
Page 23 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
PARTNER CONDITION SYMPTOMS TESTS RECOMMENDED TREATMENT ALTERNATIVES REPORTING SERVICES Candidiasis
Candi 1.Thick white SEE ABOVE Terazol 7, 0.4% vaginal cream, Femstat N/A N/A da discharge of a 1 application full H.S. for vaginal cream (Yeast cottage cheese 7 days 2% - one ) consistency applicator full OR 2.Itching and of cream burning of the Clotrimazole vaginal cream intravaginally, labia and vulva 1% (over the counter) – 5 g at bedtime, for intravaginally for 7-14 days 3 days 3.Painful intercourse OR OR 4.Burning during Clotrimazole vaginal cream Fluconazole 150 urination 2% (over the counter) – 5 g mg PO for intravaginally for 3 days 1 dose 5.Pelvic exam (contraindicated reveals cheese in pregnancy) discharge in Assessment is made by labial folds and observing budding yeast at vaginal cells or pseudo hyphae on opening with 10% KOH exam, wet mount or patches Gram stain adhering to OR vaginal wall and cervix Clinical presentation and symptoms
Consult and/or direct patient to a higher level provider if candida is suspected
(If pH is abnormally high (>4.5) consider concurrent BV or Trichomoniasis)
Page 24 of 27 Core Clinical Service Guide Section: STD September 1, 2012 PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
PARTNER CONDITION SYMPTOMS TESTS RECOMMENDED TREATMENT ALTERNATIVES REPORTING SERVICES HPV HUMAN PAPILLOMAVIRUS (Genital Warts) HPV (Genital 1. Pedunculate Screening women EXTERNAL GENITAL WARTS EXTERNAL GENITAL N/A N/A Warts) d, elongated, or men with an WARTS raised fleshy HPV test, outside PROVIDER –APPLIED Cryotherapy lesions of the of the with liquid nitrogen or cryoprobe. PATIENT-APPLIED genitalia; pink recommendations Repeat application every 1-2 weeks. (Available w/script) to red in for cervical cancer OR Podofilox 0.5% solution or 14 color. Large screening, is not Trichloroacetic acid (TCA) or gel . Apply 2 times a day lesions recommended. bichloroacetic acid (BCA) 80% -90%. for 3 days, followed by 4 days of no therapy. This appear in Apply small amount only to warts. cycle can be repeated as cauliflower- Assessment of Allow to dry. Repeat weekly if necessary for up to like masses or genital warts is necessary 4 times. Total wart area clusters made by visual OR should not exceed 10 cm2 2. Usually inspection. HPV Podophyllin resin 10%-25%14 in a and total volume applied painless, may be confirmed compound tincture of benzoin. Allow to daily not to exceed 0.5 mL. unless there by biopsy, but air dry. Limit application to <10 cm2 (Contraindicated in pregnancy).OR is irritation needed only under and to <0.5 ml. Wash off 1-4 hours after 14 . from friction certain application. Repeat weekly if Imiquimod 5% cream Apply once daily at or secondary circumstances necessary. (Contraindicated in bedtime 3 times a week for infection (diagnosis is pregnancy). up to 16 weeks. Wash uncertain, lesions treatment area with soap do not respond to and water 6-10 hours after standard therapy; application (Not for use in lesions worsen Consult and/or direct the patient to a pregnancy) during therapy, higher level provider for evaluation and OR warts are treatment of suspected HPV lesions Sinecatechins 15% pigmented, ointment (Not for use in pregnancy) indurated, bleeding, etc.)
PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
PARTNER CONDITION SYMPTOMS TESTS RECOMMENDED TREATMENT ALTERNATIVES REPORTING SERVICES HPV HUMAN PAPILLOMAVIRUS (Genital Warts) HPV SEE ABOVE SEE ABOVE EXTERNAL GENITALPage 25 of WARTS27 EXTERNAL GENITAL N/A N/A Core Clinical Service Guide (Genital Section: STD WARTS Warts) and Genital warts can PROVIDER –APPLIEDSeptember 1, Cryotherapy2012 Pregnancy proliferate and with liquid nitrogen or cryoprobe. N/A become friable Repeat application every 1-2 weeks. during pregnancy. OR (Imiquimod, podophyllin, Many specialists Trichloroacetic acid (TCA) or Sinecatechins and advocate their Podofilox should not be removal during bichloroacetic acid (BCA) 80% -90%. PROTOCOLS FOR TREATMENT OF COMMON SEXUALLY TRANSMITTED DISEASES (continued)
1 Some patients who are allergic to penicillin may also be allergic to ceftriaxone or other cephalosporin regimens. Doxycycline is the preferred syphilis treatment if allergic to PCN. There are limited clinical studies for ceftriaxone for the treatment of syphilis. If neither penicillin nor doxycycline can be administered for the treatment of syphilis desensitization may be necessary. Close follow-up of persons receiving any alternative therapies is essential. 2 Tetracycline/doxycycline is contraindicated in pregnancy; erythromycin is not recommended for the treatment of syphilis in pregnancy because it does not reliably cure an infected fetus; data insufficient to recommend azithromycin or ceftriaxone. 3 Cefixime tablets are currently not available through the state STD Program, and spectinomycin is not currently available in the US. 4 In most situations Quinolones should not be used for the treatment of gonorrhea. If a quinolone is the only alternative regimen available for gonorrhea, a test of cure is required. 5 Unreliable to treat pharyngeal infections. Patients who have suspected or known pharyngeal infection should have a pharyngeal culture 3-5 days after treatment to verify eradication of infection. 6 The efficacy of treating neonatal Chlamydial conjunctivitis and pneumonia is about 80%. A second course of therapy may be required. An association between oral erythromycin and infantile hypertrophic pyloric stenosis (IHPS) has been reported in infants aged less than 6 weeks treated with this drug. Data on other macrolides (azithromycin, clarithromycin) for the treatment of neonatal Chlamydial infection are limited. The results of one study involving a limited number of patients suggest that a short course of azithromycin 20 mg/kg/day, 1 dose daily for 3 days may be effective for Chlamydial conjunctivitis. 7 Infections with M. genitalium may respond better to azithromycin. 8 If this dose cannot be tolerated, then erythromycin base 250 mg orally or erythromycin ethylsuccinate 400 mg orally 4 times a day for 14 days can be used. 9 The recommended regimen of ceftriaxone and doxycycline is for epididymitis most likely caused by GC or CT infection. The alternative regimen of ofloxacin or levofloxacin is recommended if the epididymitis is most likely caused by enteric organisms, or for patients allergic to cephalosporins and/or tetracycline. 10 Metronidazole will also treat bacterial vaginosis, frequently associated with PID. Whether the management of immunodeficient HIV-infected women with PID requires more aggressive intervention has not been determined. 11 Multiple studies and meta-analyses have not demonstrated a consistent association between metronidazole use during pregnancy and teratogenic or mutagenic effects in newborns. Screening for, and oral treatment of, BV in pregnant women at high risk for premature delivery is recommended by some experts and should occur at the first prenatal visit. Intravaginal clindamycin treatment for low risk women should be used only during the first half of pregnancy. 12 Clindamycin cream is oil-based and may weaken latex condoms and diaphragms for 5 days after use. 13 Safety during pregnancy not established.
Page 26 of 27 Core Clinical Service Guide Section: STD September 1, 2012 A. Table I STD Drugs in Pregnancy
DRUG USE IN PREGNANCY
Acyclovir OK Amoxicillin OK Azithromycin OK Cefixime OK Cefoxitin OK Ceftriaxone OK Clindamycin OK; do not use cream in pregnancy Clotrimazole* OK Doxycycline Contraindicated Erythromycin+ OK Famciclovir No data; avoid Fluconazole Avoid Imiquimod Contraindicated Lindane Contraindicated Metronidazole OK; Avoid repeated dosing in pregnancy Ofloxacin Contraindicated Penicillin G (all forms) OK Permethrin OK Podophyllin Contraindicated Podofilox Contraindicated Probenecid OK Pyrethrins OK Sinecatechins Contraindicated Trimethroprim-sulfamethoxazole Avoid especially third trimester Valacyclovir No data; avoid
+ Except erythromycin estolate (Ilosone), this is contraindicated.
Medications available from the State STD Program for the treatment of STDs:
Amoxicillin (500 mg tablets) Benzathine Penicillin G (Bicillin LA) Azithromycin (500 mg tablets) Doxycycline Hyclate (100 mg tablets) Ceftriaxone (Rocephin) 250 mg Erythromycin (250 mg and 500 mg tablets)
Page 27 of 27 Core Clinical Service Guide Section: STD September 1, 2012 STD Offices by Area Developmental Districts (ADD) ADD STD Office Telephone
1–4 Warren County Health Dept., Bowling Green, KY (270) 781-2490, ext. 213 or ext. 214
5–6 Specialty Clinic, Louisville, KY (502) 574-6699
Northern Kentucky Independent District Health 7 (859) 363-2075 Dept., Florence, KY
8–15 Fayette County Health Dept., Lexington, KY (859) 288-2458
State Kentucky Public Health Department – STD Program (501) 564-4804, ext. 3541 or ext. 3544 Office Regional STD Programs should be contacted to initiate partner services for early syphilis and/or HIV cases.
Page 28 of 27 Core Clinical Service Guide Section: STD September 1, 2012