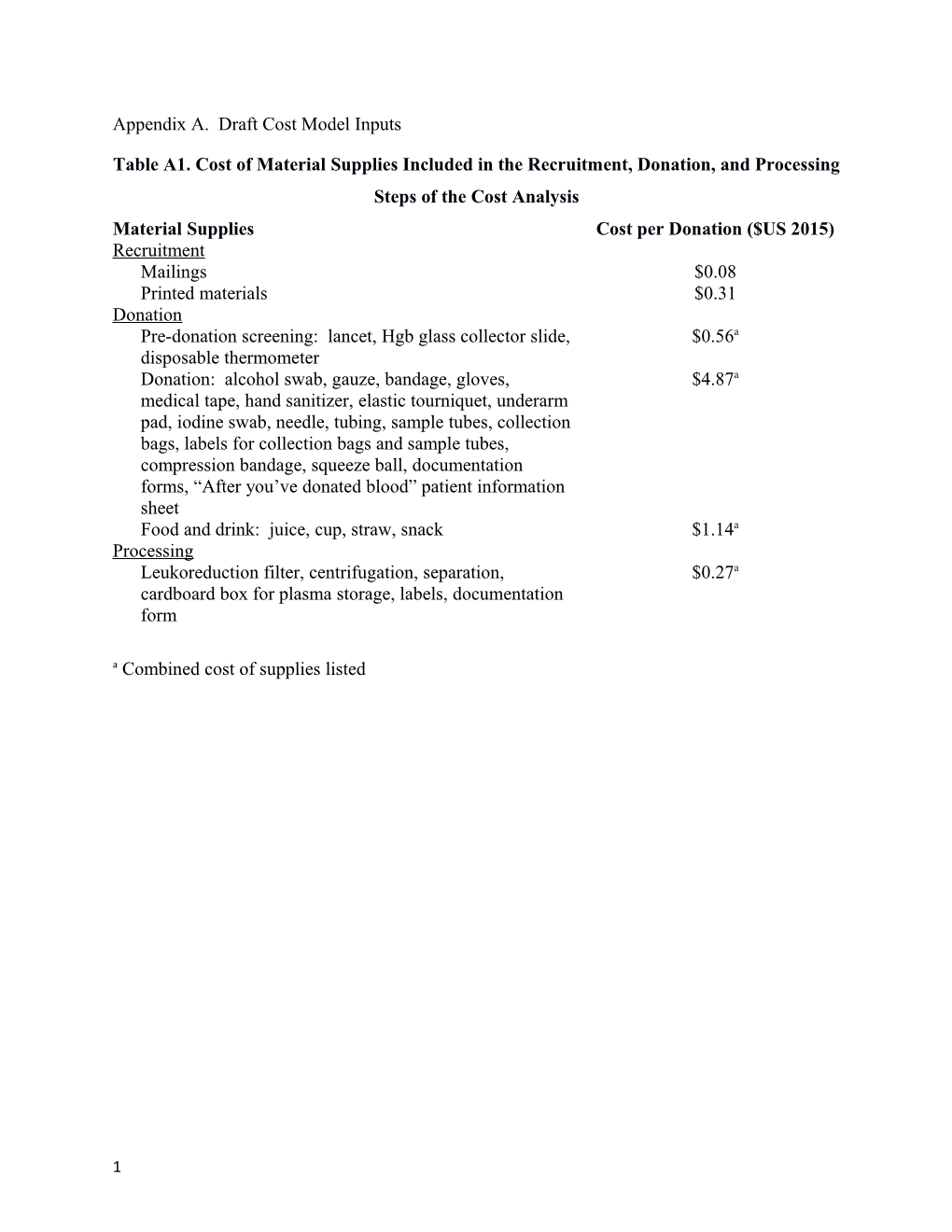
Appendix A. Draft Cost Model Inputs
Table A1. Cost of Material Supplies Included in the Recruitment, Donation, and Processing Steps of the Cost Analysis Material Supplies Cost per Donation ($US 2015) Recruitment Mailings $0.08 Printed materials $0.31 Donation Pre-donation screening: lancet, Hgb glass collector slide, $0.56a disposable thermometer Donation: alcohol swab, gauze, bandage, gloves, $4.87a medical tape, hand sanitizer, elastic tourniquet, underarm pad, iodine swab, needle, tubing, sample tubes, collection bags, labels for collection bags and sample tubes, compression bandage, squeeze ball, documentation forms, “After you’ve donated blood” patient information sheet Food and drink: juice, cup, straw, snack $1.14a Processing Leukoreduction filter, centrifugation, separation, $0.27a cardboard box for plasma storage, labels, documentation form a Combined cost of supplies listed
1 Table A2. Cost of Material Supplies Included in the Thawing through Administration Steps of the Cost Analysis
Material Supplies Cost per Patient ($US 2015) Thawing and labeling Labels $0.06 Pre-administration Blood typing and screening: gloves, tourniquet, alcohol $8.29a swab, needle with or without tubing, test tube, gauze, bandage, solid phase testing materials (reagent, trays, pipettes) Consent form $0.10 Administration Transfusion and vital sign monitoring: gloves, alcohol $10.74a swab, needle, tubing, disposable temperature probe covers, Clearlink blood filtration system, saline flush, documentation form Adverse events: blood bank lab testing materials, $2.74a documentation form a Combined cost of supplies listed
2 Figure A1. Plasma Adverse Events Tree
Summary of Variables Included in the Plasma Adverse Events Tree
VARIABLE NAME DESCRIPTION VALUE c_TACO Mean cost of treatment for TACO 6692 c_TRALI Mean cost of treatment for TRALI 21412 c_mistransfusion Mean cost of treatment for mistransfusion 9785 p_TACO Probability of TACO 1:68 p_TRALI Probability of TRALI 1:317,000 p_mistransfusion Probability of mistransfusion 1:12,000
3 Appendix B. Selected Tables from the Plasma Cost Focus Group Worksheet
Table B2. Potential Parameters to be Tested in Sensitivity Analysis
Agree or If Disagree, Assumption to be Varied Disagree Reason Donor recruitment costs: gifts (t-shirts, mugs, etc.), donor recruitment service Donor recruitment and donation costs are halved to find cost of plasma donation because TJUH produces only 1 unit RBC and 1 unit plasma per donation. Test ⅓ of these costs (vs. ½) to account for institutions that obtain 1 unit plasma + 1 unit RBC + 1 unit platelets per donor Plasma from female donors is not discarded. Test discarding plasma from female donors Test discarding plasma from all female donors except type AB Test adding cost of HLA antibody testing for female donations instead of discarding plasma Test efficiency of pre-thawing plasma vs. thawing as needed Test cost of a butterfly needle vs. standard needle for pre- administration type and screen 2nd tube required to confirm blood type TJUH types donor and recipient blood samples with solid phase testing machine. Test using other methods of typing (gel card, test tube) Blood Bank physician check for appropriateness and accuracy Delivery of plasma to the floor: test impact of lower level floor staff (i.e., LPN) Test prophylaxing patient with acetaminophen and/or diphenhydramine (TJUH does not routinely do this) Test varying wastage to account for differences in usage at small vs. large hospitals Test adverse event probability ranges found in the literature Test adverse event reimbursement ranges Test varying time requirements per task Test varying personnel wage rates & fringe benefits costs Test varying cost of purchased plasma Other parameters we should modify? (please list in the blank boxes below)
4 Table B2. Other Key Questions
Question Reviewer Response What was the total number of plasma units dispensed in 2012, across all patients at your institution? What was the total number of patients transfused with plasma at your institution, in 2012? What is your institution’s current supplied plasma cost, per bag? (An approximation or range is okay if exact pricing is considered confidential) What are your institution’s current shipping/transport costs for supplied plasma (if possible please indicate approximate cost per bag; if that is not known, then total monthly costs would be okay)? What percent of plasma units have to get returned to the supplier (for example due to recall, look back)? Does a blood bank or transfusion service physician review plasma orders at your institution before the product is dispensed to the patient? What percent of plasma orders are rejected/denied at your institution due to clinical judgment (i.e., determined to be inappropriate or unnecessary)? What percent of the time does a nurse or transport come to pick up plasma from the Blood Bank (in other words, instead of sending the product to the floor via pneumatic tubes)? Is there a criterion at your institution determining whether plasma bags are picked up vs. pneumatic-tubed (for example, the order must be picked up if it consists of multiple bags)? If this criterion exists, please briefly describe it. What percent of plasma recipients at your institution are prophylaxed with acetaminophen and/or diphenhydramine? What percent of plasma units that are thawed by the Blood Bank end up being wasted (for example, thawed bags in the Blood Bank’s refrigerators that are not used within 5 days, thawed bags which are mistakenly left at room temperature on the patient floor for too long)? What percent of frozen plasma is wasted by your institution due to reaching the 1 year expiration date?
5 Appendix C. Changes to the draft model recommended by the focus group and accepted by the investigators
1. Include a scenario where donor recruitment costs are significantly reduced, since donors are recruited for the purpose of obtaining blood, not plasma. Thus, plasma could be viewed as a byproduct of the blood donation process. Our draft model assumed $36.13 per donor for telerecruitment; the final model assumed $1.95 per donor recruited 2. Add probability of a potential donor failing the pre-donation screening; we estimated this to be 22% 3. Add wastage for the following steps: a. Processing, where wastage is assumed if the donor plasma fails pathogen testing or leukoreduction and the wastage cost is calculated as the sum of costs occurring prior to the wastage b. Thawing, where wastage is assumed if the plasma bag breaks or expires before use and the wastage cost is calculated as the sum of costs occurring prior to the wastage 4. Personnel costs for the tasks performed during donation, where a technologist/technician is assumed to do a set of tasks, then test the impact of a nurse performing these tasks, since some institutions have nurses completing donation (tasks affected included pre- donation screening interview and completion of the donation itself) 5. Personnel costs for centrifugation, to account for lower or higher level technologists/technicians performing this task (personnel costs for this task were modified by +/-25% in the final model) 6. Include only the following adverse events: TACO, TRALI, and mistransfusion since the infectious events considered (transmission of Hepatitis B, Hepatitis C, or West Nile Virus) are exceedingly rare and hence there is limited data on the rate of their occurrence. Further, these events were assumed to be detected post-hospitalization and thus were beyond the scope of our model’s time horizon 7. Reduce the probability of TACO since the assumption used in the draft model (0.01471 or 1/68 cases) seems high. In the final model we assumed that the probability of TACO could be as low as 0% but as high as that in our draft model 1.47%) 8. Increase the probability of TRALI since the assumption used in the draft model (0.00000315 or 1/317,000 cases) seems low. In the final model we assumed that the probability of TRALI could be as low as 0.00000315 or as high as 0.0001 9. Modify the cost of adverse events +/- 50% to account for uncertainty in the published reimbursement data used to inform the draft model 10. In the case of an adverse event, add wastage (the transfusion is stopped). In this case it was assumed that one unit of plasma would be wasted per event 11. Probability of blood typing on the patient before administration, to account for patients having their blood type on record in the medical record/chart (draft model assumption
6 was that all patients required typing; final model base case was 25% and range tested was 10-50%) 12. For purchased plasma, modify the cost to account for pricing differences between institutions (base case assumption was $40.47 per unit; range tested in final model was $36.13-$61.94 per unit) 13. For purchased plasma, add the costs of receiving, inventory, and storage
7 Appendix D. Decision Trees Included in the Model
Figure D1. Donor Recruitment (Step 1) Decision Tree
Summary of Variables Included in the Step 1 Decision Tree
VARIABLE NAME DESCRIPTION VALUE c_telerecruit Cost of blood donation telerecruitment service 5.46 cm_mailing Material cost of blood donation recruitment mailings 0.08 cm_printed Material cost of printed materials (posters, signage, etc.) 0.31 cp_mailing Personnel cost of blood donation recruitment mailings 0.04 cp_printed Personnel cost of printed materials (posters, signage, etc.) 0.04 p_telerecruit Probability of blood donor recruited by telerecruitment service 0.2955
8 Figure D2. Blood Donation (Step 2) Decision Tree
Summary of Variables Included in the Step 2 Decision Tree
VARIABLE NAME DESCRIPTION VALUE Material cost of Blood Bank documentation of failures in the 0 cm_BBfaildocument process Material cost of blood donation from needle stick preparation 4.87 cm_donation through donation finish cm_foodandgiveaway 1.14 Material cost of food and giveaways s cm_screening Material cost of blood donor pre-donation screening 0.56 Personnel cost of Blood Bank documentation of failures in the 0 cp_BBfaildocument process Personnel cost of blood donation from needle stick preparation 3.47 cp_donation through donation finish cp_screening Personnel cost of blood donor pre-donation screening 0.77
9 p_alimentation Probability of giving snack and/or drink to blood donor 1 p_failstick Probability of blood donor needle stick failure 0.032609 p_longdonate Probability of blood donation lasting >15 minutes 0.028777 p_screenfail Probability of a blood donor failing pre-donation screening 0.22
10 Figure D3. Processing of the Donation into Plasma (Step 3) Decision Tree
Summary of Variables Included in the Step 3 Decision Tree
VARIABLE NAME DESCRIPTION VALUE c_ABOtype Cost of internal ABO typing of donated blood (service cost) 1.27 c_exttest Cost of external testing of donated blood (service cost) 11.25 c_WBwastage Cost of wastage of one unit of whole blood 10.64 cm_BBfaildocument Material cost of Blood Bank documentation of failures in the 0 process cm_centrifuge Material cost of whole blood centrifugation, component 0.27 separation, bagging, documentation, and storage cm_leukoreduce Material cost of leukoreduction 0 cp_BBfaildocument Personnel cost of Blood Bank documentation of failures in the 0 process cp_centrifuge Personnel cost of whole blood centrifugation, component 6.39 separation, bagging, documentation, and storage
11 cp_leukoreduce Personnel cost of leukoreduction 0.38 cp_resting Personnel cost of resting stage of processing 0.07 p_failexttest Probability of donated blood failing external testing 0.012 p_leukofail Probability of leukoreduction filter failure 0.002
12 Figure D4. Thawing and Labeling the Plasma for the Patient (Step 4) Decision Tree
Summary of Variables Included in the Step 4 Decision Tree
VARIABLE NAME DESCRIPTION VALUE c_unitwastage Cost of wastage of an entire unit of plasma 37.17 cm_BBfaildocument Material cost of Blood Bank documentation of failures in the 0 process cm_tagconvert Material cost of tagging and converting a unit of plasma 0.06 cm_thaw Material cost of thawing a unit of plasma 0 cp_BBfaildocument Personnel cost of Blood Bank documentation of failures in the 0 process cp_tagconvert Personnel cost of tagging and converting a unit of plasma 2.55 cp_thaw Personnel cost of thawing a unit of plasma 2.55 p_thawfail Probability of failure of plasma unit to thaw correctly 0.01923 p_unitexpiration_posttha Probability of thawed unit of plasma expiring before use after 0.014297 w thawing p_unitexpiration_prethaw Probability of unit of plasma expiring before thawing 0
13 Figure D5. Ordering and Obtaining the Plasma for the Patient (Step 5) Decision Tree
Summary of Variables Included in the Step 5 Decision Tree
VARIABLE NAME DESCRIPTION VALUE cm_consent Material cost of consent process 0.10 cm_orderplasma Material cost of ordering plasma from the Blood Bank for 0 administration to a patient cm_recipsample Material cost of taking a recipient blood sample for ABO typing 8.29 cp_consent Personnel cost of consent process 5.24 cp_cooler Personnel cost of delivery of plasma to floor by transportation in a 9.64 cooler cp_orderplasma Personnel cost of ordering plasma from the Blood Bank for 5.24 administration to a patient cp_pneumatic Personnel cost of delivery of plasma to floor via pneumatic tube 0 system cp_recipsample Personnel cost of taking a recipient blood sample for ABO typing 6.81 p_pneumatic Probability of delivery of plasma to floor via pneumatic tube 0.8 system p_recipsample Probability of taking a recipient blood sample for ABO typing 0.25
14 15 Figure D6. Administering Plasma to the Patient and Adverse Events (Step 6) Decision Tree
Summary of Variables Included in the Step 6 Decision Tree
VARIABLE NAME DESCRIPTION VALUE c_mistransfusion Cost of mistransfusion based on ICD-9 code 999.89 9785.95 c_TACO Cost of TACO based on ICD-9 code 276.61 6693.04 c_TRALI Cost of TRALI based on ICD-9 code 518.7 21411.11 c_unitwastage Cost of wastage of an entire unit of plasma 37.17 cm_BBAEdocument Material cost of Blood Bank documentation after AE 0 cm_BBAEtesting Material cost of Blood Bank lab testing after AE 2.64 cm_FlAEdocument Material cost of AE documentation done on hospital floor by floor 0.10 nurse cm_transfus Material cost of vital sign taking during transfusion process 10.74 cm_transident Material cost of identity and blood type verification at beginning 0 of transfusion cp_BBAEdocument Personnel cost of Blood Bank documentation after AE 5.10 cp_BBAEtesting Personnel cost of Blood Bank lab testing after AE 34.82
16 cp_FlAEdocument Personnel cost of AE documentation done on hospital floor by 8.29 floor nurse cp_transfus Personnel cost of tranfusion process 33.54 cp_transident Personnel cost of identity and blood type verification at beginning 14.92 of transfusion p_mistransfusion Probability of mistransfusion per unit RBC transfused 0.0000833 p_returnedunusable Probability of unused unit(s) of plasma being returned from the 0.01126 floor not in usable condition p_TACO Probability of TACO per unit transfused 0.01471 p_TRALI Probability of TRALI per unit transfused 0.00000315457
17