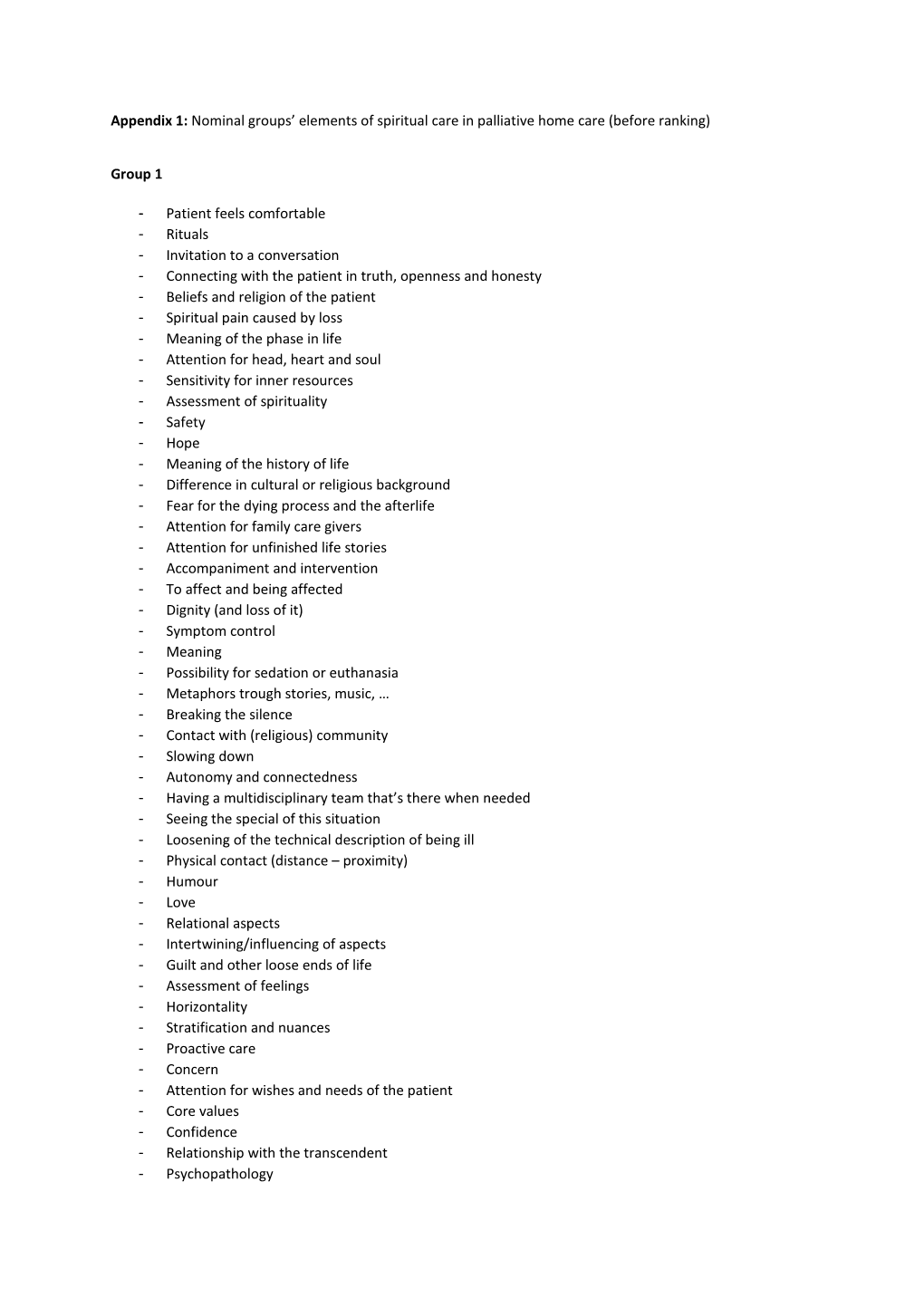
Appendix 1: Nominal groups’ elements of spiritual care in palliative home care (before ranking)
Group 1
- Patient feels comfortable - Rituals - Invitation to a conversation - Connecting with the patient in truth, openness and honesty - Beliefs and religion of the patient - Spiritual pain caused by loss - Meaning of the phase in life - Attention for head, heart and soul - Sensitivity for inner resources - Assessment of spirituality - Safety - Hope - Meaning of the history of life - Difference in cultural or religious background - Fear for the dying process and the afterlife - Attention for family care givers - Attention for unfinished life stories - Accompaniment and intervention - To affect and being affected - Dignity (and loss of it) - Symptom control - Meaning - Possibility for sedation or euthanasia - Metaphors trough stories, music, … - Breaking the silence - Contact with (religious) community - Slowing down - Autonomy and connectedness - Having a multidisciplinary team that’s there when needed - Seeing the special of this situation - Loosening of the technical description of being ill - Physical contact (distance – proximity) - Humour - Love - Relational aspects - Intertwining/influencing of aspects - Guilt and other loose ends of life - Assessment of feelings - Horizontality - Stratification and nuances - Proactive care - Concern - Attention for wishes and needs of the patient - Core values - Confidence - Relationship with the transcendent - Psychopathology - Possibility for referral - Diagnosis and duration of the illness - Enjoying
Group 2
- Patient’s expectations and wishes about the end of life - Making an inventory of needs - How is the patient’s spirituality? - Does the patient need help? - Tuning to the patient - Allowing feelings, whatever they are - What is the spiritual dimension of care? - Do I know the standards and values of my patient? - Meaning in ending up life - Is the story of my patient finished (dreams, passions)? - Confidence in the professional care giver - Respect for each other’s spirituality - Making contact - Preconditions: space, rest, tempo - Is spiritual care part of integral care? - Diagnosis of existential/spiritual peace and pain - To account for the enormous diversity of people - Dreams and passions of the patient - Sources of inspiration of the patient - Rest and space, attention - Is the care restricted to one setting? - Facilitating spiritual/religious rituals - Freedom of physical and psychological suffering - Good balance individual-community - Communication with partner - Do I know my boundaries as a care giver? - Multidisciplinary consultation (general practitioner, nurse, …) - Secrecy - Daring to talk about life questions - Assessing connections - Listening to stratification
Group 3
- Goal is spiritual well-being - Learning to give the disease a place - Attention for all elements in the home context - Not coinciding with the disease - Making a life balance - Contribute to ars moriendi - Making authentic contact - Finding and accepting a new place in life - The person of the care giver with his own conscious spiritual development - Individual process (personal) - Preserving connectedness (all layers of being) - Elements awarded to the patient - Contingent processing - Resources - Wounded healer; recognising vulnerability - Curiosity and challenge - Willingness to listen - Measuring the patient’s horizon - Giving space to rituals - Enlarging the metaphorical capacity of language - Caring for the problems with meaning - Experience of loss - Care for the carers - Not uncoupling - Insight in structure of spiritual care - Knowing how to inform - Care for the environment - Respectful attitude - Unfinished business - Musicality - Patient as a teacher - Attention for religious stories - Narrativity - Creating a space wherein something can flow (physical, emotional, social care) - Openness for the sacred - Attention for shift in meaning of all possible elements in the home context
Group 4
- Feeling at home; being yourself; feeling safe - Attitude and skills of care giver to stimulate the patient to think about spiritual topics - Intertwined but specific dimension - Continuity of spiritual care (time, team) - Attention for communication and quality of relationships - Respect for the patient as a human being - Supporting the patient in ‘enduring’, enlarging patient’s capacity - Meaning of proceedings that do or doesn’t happen - Positioning what is reached and the disappointments in life - Care giver is the guest, patient is the host - Making time - Healing and reconciliation - Attention for coming to terms - Awareness of own and patient’s standards and values - Creating preconditions (space, time) to realise what patients regard as valuable - Attention for the ‘now’ - Solving ‘unresolved business’ - Support of the spiritual experiences of bystanders - Attention and space for confounders - Attention for meaning - Alignment of patient and bystanders - Time for telling stories - Who/what can support this aspect? - Dare to refer - Making non-verbal expression of connectedness possible - Designing the farewell - Rituals about dying - Availability of a professional spiritual care giver in the home care team - Attention for religion - Attention for the end of life - Silence