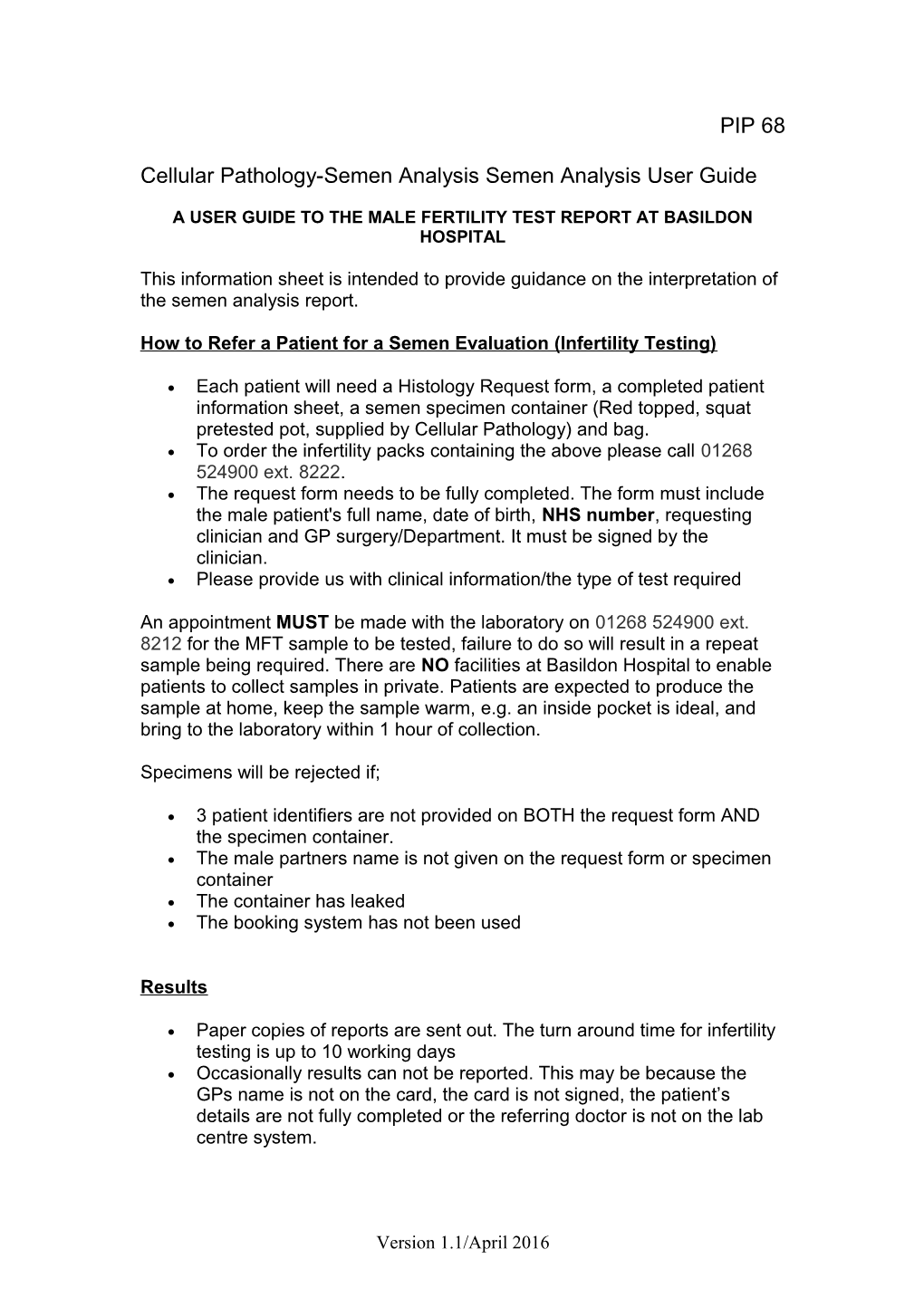
PIP 68
Cellular Pathology-Semen Analysis Semen Analysis User Guide
A USER GUIDE TO THE MALE FERTILITY TEST REPORT AT BASILDON HOSPITAL
This information sheet is intended to provide guidance on the interpretation of the semen analysis report.
How to Refer a Patient for a Semen Evaluation (Infertility Testing)
Each patient will need a Histology Request form, a completed patient information sheet, a semen specimen container (Red topped, squat pretested pot, supplied by Cellular Pathology) and bag. To order the infertility packs containing the above please call 01268 524900 ext. 8222. The request form needs to be fully completed. The form must include the male patient's full name, date of birth, NHS number, requesting clinician and GP surgery/Department. It must be signed by the clinician. Please provide us with clinical information/the type of test required
An appointment MUST be made with the laboratory on 01268 524900 ext. 8212 for the MFT sample to be tested, failure to do so will result in a repeat sample being required. There are NO facilities at Basildon Hospital to enable patients to collect samples in private. Patients are expected to produce the sample at home, keep the sample warm, e.g. an inside pocket is ideal, and bring to the laboratory within 1 hour of collection.
Specimens will be rejected if;
3 patient identifiers are not provided on BOTH the request form AND the specimen container. The male partners name is not given on the request form or specimen container The container has leaked The booking system has not been used
Results
Paper copies of reports are sent out. The turn around time for infertility testing is up to 10 working days Occasionally results can not be reported. This may be because the GPs name is not on the card, the card is not signed, the patient’s details are not fully completed or the referring doctor is not on the lab centre system.
Version 1.1/April 2016 Occasionally the sample is unsuitable for analysis. You will be informed of this via letter. Common reasons for not processing samples include; the sample leaking or the patient not booking an appointment.
Interpretation of Results
Physical Elements Colour Normally homogenous, grey- Reported as opalescent appearance, it NORMAL may appear less opaque if the or BLOODSTAINED concentration is low. A bloody sample would be indicative of haematospermia.
Volume Can be of importance in low 1.5ml is the lower sperm density, poor motility reference and poor morphology specimens. limit as advised by Low semen volume can also be World the result of collection Health Organisation problems (loss of a fraction of the (WHO) ejaculate), or partial retrograde ejaculation. Low semen volume is characteristic of obstruction of the ejaculatory duct or congenital bilateral absence of the vas deferens pH If the pH is less than 7.0 in a 7.2 is the lower semen sample with low threshold volume and low sperm numbers, limit there may be ejaculatory duct obstruction or congenital bilateral absence of the vas deferens. Viscosity High viscosity can interfere with Reported as either the determinations of NORMAL or VISCOUS motility, concentration and antibody coating of spermatozoa.
Concentratio The total number of spermatozoa The lower reference n per ejaculate and the limit for spermatozoa is sperm concentration are related to 15 million per ml both time to pregnancy and pregnancy rates Motility The total number of motile 32% is considered the
Version 1.1/April 2016 spermatozoa {progressive and lower non progressive motility} in the limit for progressive ejaculate is of biological motility significance as it is related to pregnancy rates.
Morphology The total number of The lower reference morphologically normal limit for spermatozoa normal morphology is in the ejaculate is of biological 4 % significance as fertilisation rates decrease with less than 8% normal morphology
Sperm with WHO advise that we classify the No reference ranges defects different kinds of advised by World malformations seen Health morphologically as abnormal Organisation (WHO) spermatozoa generally have a lower fertilising potential. Classifications are divided into head, neck/midpiece or tail abnormalities.
All of the analyses need to be read together and a single aberrant result may not be of any significance.
Version 1.1/April 2016