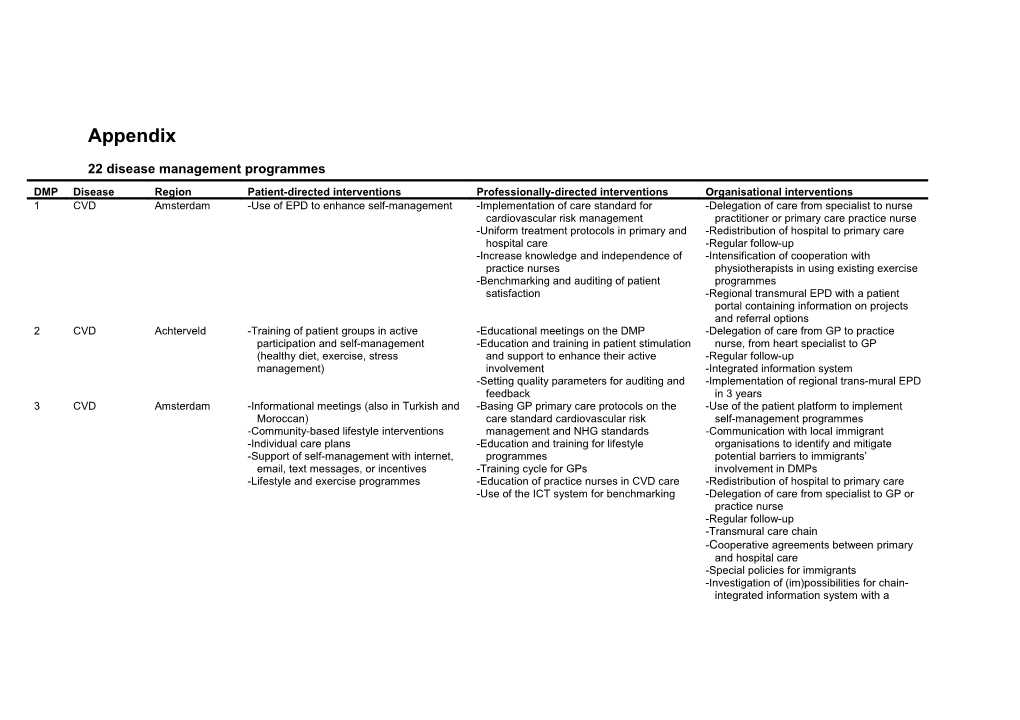
Appendix
22 disease management programmes
DMP Disease Region Patient-directed interventions Professionally-directed interventions Organisational interventions 1 CVD Amsterdam -Use of EPD to enhance self-management -Implementation of care standard for -Delegation of care from specialist to nurse cardiovascular risk management practitioner or primary care practice nurse -Uniform treatment protocols in primary and -Redistribution of hospital to primary care hospital care -Regular follow-up -Increase knowledge and independence of -Intensification of cooperation with practice nurses physiotherapists in using existing exercise -Benchmarking and auditing of patient programmes satisfaction -Regional transmural EPD with a patient portal containing information on projects and referral options 2 CVD Achterveld -Training of patient groups in active -Educational meetings on the DMP -Delegation of care from GP to practice participation and self-management -Education and training in patient stimulation nurse, from heart specialist to GP (healthy diet, exercise, stress and support to enhance their active -Regular follow-up management) involvement -Integrated information system -Setting quality parameters for auditing and -Implementation of regional trans-mural EPD feedback in 3 years 3 CVD Amsterdam -Informational meetings (also in Turkish and -Basing GP primary care protocols on the -Use of the patient platform to implement Moroccan) care standard cardiovascular risk self-management programmes -Community-based lifestyle interventions management and NHG standards -Communication with local immigrant -Individual care plans -Education and training for lifestyle organisations to identify and mitigate -Support of self-management with internet, programmes potential barriers to immigrants’ email, text messages, or incentives -Training cycle for GPs involvement in DMPs -Lifestyle and exercise programmes -Education of practice nurses in CVD care -Redistribution of hospital to primary care -Use of the ICT system for benchmarking -Delegation of care from specialist to GP or practice nurse -Regular follow-up -Transmural care chain -Cooperative agreements between primary and hospital care -Special policies for immigrants -Investigation of (im)possibilities for chain- integrated information system with a patient portal 4 CVD Eindhoven -Patient education -DMP education -GP as the central care provider in close -Motivational training -Training in motivational training collaboration with the practice nurse -Personal coaching -Use of validated performance and process -Emphasis of care providers’ coaching role -Facilitation of self-monitoring and self- indicators as quality parameters for -GP responsibility for primary care patients management auditing and feedback and ambulatory patients in hospital care -Customised programmes to quit smoking, -Individual monitoring of patients and -Specialist responsibility for clinical patients exercise, maintain healthy diet and evaluating quality of care at group level -Exercise programmes provided by a develop coping skills -Provision of feedback and suggestions for consultant at regular sports facilities improvement by the care registration team -Regular follow-up -Cooperation with diagnostic centres and hospital care specialists -Cooperative agreements between primary and hospital care -Early detection of high-risk patients -Uniform systematic registration by all professionals -Support of ICT-registration system for monitoring and feedback 5 CVD Maarssen -Lifestyle advisors and plans (exercise, diet, -Cardiovascular programme based on the -Mapping of patients’ wishes and active quit smoking) care standard for cardiovascular risk involvement of patients or patient groups -Motivational interviewing management in the CVD programme -Exercise programmes -Setting quality parameters for auditing and -Annual patient satisfaction inquiry -Quit smoking consultation hours feedback -Central care director (nurse practitioner) -Development of individual patient care -Benchmarking responsible for content of the care plan, plans based on their risk profiles -Regular intervention and goals evaluation delegation of lifestyle interventions to the by central care director lifestyle advisor, regular meetings with the pharmacist on patients’ medication use, and proactive contact with other involved professionals -Collaboration of lifestyle advisor and patient on coaching and lifestyle plans -CVD practice nurse consultation hours 4 times a week. Patient inflow through GP and active involvement with at-risk patients -Shared decision making and actively reminding patients of their decisions and treatment plans -Regular follow-up -Expansion of chain care to hospital care -Trans-mural protocol -Chain-integrated information system with a patient portal 6 Heart failure Alkmaar -Education of patients to enhance self- -Implementation of CBO trans-mural -Involvement of patient associations management skills guidelines -Delegation of care from GP to practice -Implementation of NHG standard in all nurse and heart specialist to GP primary care settings -Patient follow-up to improve continuity of -Education of professionals involved in the care DMP -Design of a trans-mural care standard or -Setting quality parameters for auditing and protocol to improve cooperation and feedback provide clear referral agreements between all professionals involved in the DMP -Communication platform for professionals to discuss patients -Chain-integrated information system 7 Stroke Amsterdam -Informational meetings -Implementation of care standard for -Delegation of care from specialist to -Lifestyle programmes through motivational cardiovascular risk management primary care practice nurse supervised by interviewing -Checklist for risk factors GP -Customized exercise programmes -Measurement of treatment adherence -Assessment of patient satisfaction for -Assessment of patient satisfaction for quality improvement quality improvement -Lifestyle programmes provided by physical therapist and stroke nurse -Enhanced secondary prevention led by GP or stroke nurse at the nursing home and monitored by the neurologist -Regular follow-up -Multidisciplinary approach in hospital care 8 CVD Arnhem -Joint medical consultations for primary care -Improved implementation of guidelines for -Knowledge exchange and hospital care patients (n = 10), a cardiovascular care in primary and -One-stop outpatient clinic spouse/family member, and a physician hospital settings -Joint consultation hours -Implementation of care standard for -Regular follow-up in primary care cardiovascular risk management to -Cooperation between primary and hospital improve implementation of CBO and NHG care protocols in primary and hospital care -Uniform treatment plan in primary and settings hospital care -Education for GPs -Early recognition of high-risk patients at -Cooperative learning among nurses at the outpatient clinics and general practices outpatient clinic -Transmural EPD vascular risk management with a patient portal -Development of trans-mural DBC 9 CVD Nijmegen -Patient education on cardiovascular risk -Education of a Turkish-speaking practice -Delegation of care from GP to nurse management nurse -Nurse-managed consultation -Exercise programmes -Implementation of a special immigrant -Provision of customized, demand-driven -Quit smoking programme run by a quit- protocol care smoking consultant -Auditing and feedback to improve the -Semi-weekly meetings between GP and -Healthy diet plans quality of patient satisfaction and outcome practice nurse -Health counselling indicators -Ability of practice nurse to contact professionals from other disciplines (e.g., dietician) -Regular follow-up -Special immigrant policy -New structured and formalized roles and cooperation between nurses, GPs, and other professionals involved in the DMP -Development of a safe integrated ICT system 10 CVD Nijmegen* -Patient-driven choice programme: patient -Implementation of care standard for -Internist and vascular nurse as central care can choose a central care provider, the cardiovascular risk management providers risk factor(s) he/she wants to tackle, the -Education of professionals -Regular follow-up intervention(s), personal goals, and use of -Auditing and feedback sessions to improve -Contact with unmotivated patients every 3 web-based support quality of patient satisfaction and months -Individual care plans with personal goals outcomes -Development of trans-mural collaborative -Self-management support with vulnerable -Email alerts for professionals that identify care structure groups unmotivated patients -Enhanced interaction and cooperation -Motivational interviewing among professionals involved in the DMP -Cognitive behavioural therapy on referrals and treatment plans -Contact with patients of low socioeconomic status and different cultural backgrounds -Online patient files accessible to all professionals and the patient -Registration of risk profiles in the ICT system 11 CVD Huizen -Education of patients to enhance self- -Implementation of care standard for -Consultation with several patient groups management skills cardiovascular risk management -Patient satisfaction research -Motivational interviewing -Education of professionals on informing -Delegation of care from GP to practice -Individual care plans patients and motivational interviewing nurse -Exercise programmes -Education of physician’s assistants on -Practice nurse as central care provider -Quit smoking counselling cardiovascular risk factors -Identification of patient groups based on -Healthy diet counselling -Auditing and feedback on performance risk profiles -Web-based support programmes to indicators and benchmarking -Pharmacist monitoring of medication enhance self-management (access patient -Physical therapist-run exercise file, information, e-consultation) programmes -Healthy diet counselling from practice nurse in collaboration with dietician -Development of multidisciplinary treatment programme for obesity -Registration of risk profiles -Structural knowledge exchange -Regular follow-up -Cardiovascular counselling hours -Cooperation between primary and hospital care -Development of a multidisciplinary programme for obesity -Electronic self-management tool -Professional information exchange in the ICT system 12 COPD Tilburg* -Mirror interviews -Professionals work according to regional -Regional chain-integrated information COPD guidelines system -Quarterly online distribution of a newsletter and DMP information -Semi-annual casuistry meetings of lung specialists, GPs, and practice nurses on spirometry and correct interpretation of results -Regular general practice audits of lung specialists -Document review of all lung function measures performed at the general practices by lung specialist at the hospital -Individual and regional feedback from the ICT system 13 COPD Arnhem -Individual care plans -Implementation of CBO and NHG -Assignment of COPD physicians and lung -Customised exercise programmes standards nurses as consultants -Customised COPD education -Ability of GPs to adapt protocols and -Distribution of hospital to primary care -Quit smoking programmes agreements to their own practices -Chain-integrated information system -Monitoring self-management during every -Education of involved professionals in -Implementation of (care standard) protocols consultation COPD and spirometry in all information systems -Education of practice nurse in motivational -Design of a trans-mural care standard or interviewing of COPD patients protocol to improve cooperation and -Auditing and feedback on quality of life and provide clear referral agreements between process and outcome measures all professionals involved in the DMP 14 COPD Monnickendam -Individual care plans -Auditing and feedback on lung function, -Collaboration of practice nurse and COPD -Quit-smoking programmes muscles, exacerbation parameters and patient on care plan -Exercise programmes (optional) quality of life -Regional trans-mural care agreements -Patient groups to increase disease-related -Active follow-up of asthma patients for early knowledge and self-management skills detection of COPD -Treatment of psychological problems that -Development of a care plan for COPD inhibit coping skills GOLD 3 and 4 patients: policy addressing exacerbations, adherence, exercise programmes, monitoring, and changes in quality of life -Setting a regional example to facilitate regional continuation of the DMP 15 COPD Boxmeer* -Individual care plans -Educational meetings on improving -Integration of care programmes for -Education of patients through an prevention and enhancing healthy diabetes, COPD, and CVD Diabetes informational booklet lifestyles -Regional network for improved prevention -General lifestyle programmes -Systematic measurement of patient-level and healthy lifestyles CVD -E-health programmes to improve preventive outcomes and benchmarking -Participation in development of centre for behaviour, healthy lifestyle and self- prevention and health management skills -Regional ICT system to support self- -Group consultations management programmes -Attempt to implement several chain DBCs 16 COPD Almere -Education of patients through an -Education of professionals and practice -Sounding board for COPD patients for informational booklet, online information, nurses in recognizing psychosocial discussion and progress in the DMP information about patient associations, problems and screening for stress -Core team (GP and practice nurse) can be websites, and meetings -Auditing and feedback on quality of life and contacted for quality of care -Four informational meetings providing NHG standard indicators -Training of practice nurses in early general information about COPD, recognition of psychosocial problems and multidisciplinary treatment and self- referrals to mental health care management -Regular follow-up -Class/course for COPD patients with -Semi annual screening for distress psychosocial problems -Cooperative agreements -Regional transmural patient file (EPD) accessible to professionals and patients with additional COPD protocol 17 Diabetes Zeist -Education of patients -Implementation of NHG care standard for -Involvement of patient associations -E-health programmes to improve preventive diabetes -Delegation of care from GP to practice behaviour, healthy lifestyle and self- -Education of professionals nurse management skills -Auditing and feedback on patient -Hospital management of diabetic care, satisfaction dietary counselling, and eye care -Consultations with dieticians for newly diagnosed diabetics -Consultations with diabetic nurses and dieticians for new insulin users -Regular follow-up -Multidisciplinary trans-mural cooperation and cooperative agreements between primary and hospital care -ICT infrastructure to support e-health programme with multi-user functionality and patient portal 18 Diabetes Den Haag -Patient version of the diabetes standard of -Educational meetings with other partners in -Special policy for Surinamese and Hindu care the care chain to transfer knowledge people -E-health programmes for patients to keep a -Education of GPs in quality of diabetic care -Multidisciplinary cooperation between logbook and access their files -Education of practice nurses primary and hospital care -Lifestyle programmes -Auditing and feedback on process and -Exercise programmes outcome indicators based on the care standard and benchmarking -Feedback meetings to discuss results of visitations build relationships among partners
19 Diabetes Nieuwegein* -Informational meetings -Implementation of the care standard for -Auditing of patients’ experiences of quality -Informational health fair diabetes of care -Self-management course: 10–12 patients -Training for practice nurses, diabetes -Redefinition of care process leading to care are trained in medical and psychosocial nurses, and dieticians in teaching self- differentiation in three patient groups: self- aspects of self-care management managers, patients with minor support, -Minor and intensive support groups -Auditing and feedback on patients at and patients with intensive support individual and group levels (patients -Regular follow-up (intensity depends on enrolled in the self-management patient group) course/support group consultations) -ICT system with patient portal -Auditing and feedback on quality according to patient experiences 20 Depression Eindhoven -Motivational interviewing -Implementation of NHG standard for -Client board -Post-diagnostic stepped care: group and depression -Focus group discussion with patients individual interventions, internet courses -Education of professionals in interventions, -Delegation of care from GP to mental -E-consultations motivational interviewing and Beck health practice nurse Depression Inventory (to distinguish -GP or mental health practice nurse between mild and severe depression) diagnosis of patients and provision of -Auditing and feedback with bottleneck treatment (stepped care) within 2 weeks analyses, evaluation of intervention -Mental health practice nurse provision of effectiveness, benchmarking, focus group psychological education (part of group discussions with patients on care intervention) evaluation, and evaluative meetings -Physical therapist provision of exercise between GPs programme (part of group intervention) -Psychologist management of internet course -GP and/or mental health practice nurse provision of individual interventions -Email contact with patients -Stepped care method can be adapted to the demands of each individual practice -Depression screening among elderly and chronically ill patients -ICT system accessible to involved professionals -Internet self-management tool 21 Psychotic Den Bosch -Implementation of family interventions -Information module on psychotic disorders -Development and implementation of alert for relevant partners (schools, police, plans disorders social workers) -Active community treatment team -Training of involved professional on alert responsibility for intensive treatment, care, plan and addiction treatment -Implementation of multidisciplinary -Connection with internal and external guidelines on schizophrenia partners within the mental health chain, -Auditing and feedback through routine improved transition of care from critical to outcome monitoring of treatment a more stabilized situation outcomes -Auditing and feedback on patient, programme, and organisational levels 22 Eating Leidschendam* -Preventive public education through -Training of professionals in enhancing -Assessment of patient satisfaction to websites, guest lecturers at schools; patients’ self-management develop further approaches disorders provision of information to GPs -Auditing and feedback on patients’ weight, -Involvement of people with eating disorders -Educate patients on eating disorders eating behaviours, and moods in the design and development of a -Distribution of signal cards to parents programme; discussion of prevention and -Self-management enhancement through self-management internet, self-support groups, buddy -Regular follow-up contact with an experienced professional, -Early recognition of people with eating regular general assessment, psychiatric disorders home care, and regular outpatient treatment
Notes: DMP = disease management programme; CVD = cardiovascular disease; EPD = electronic patient dossier; GP = general practitioner; NHG = Dutch GPs association; ICT = information and communications technologies; CBO = Dutch Institute for Quality Improvement; DBC = documentation-based care; COPD = chronic obstructive pulmonary disease; GOLD = Global initiative for chronic obstructive lung disease; *qualitative research case.