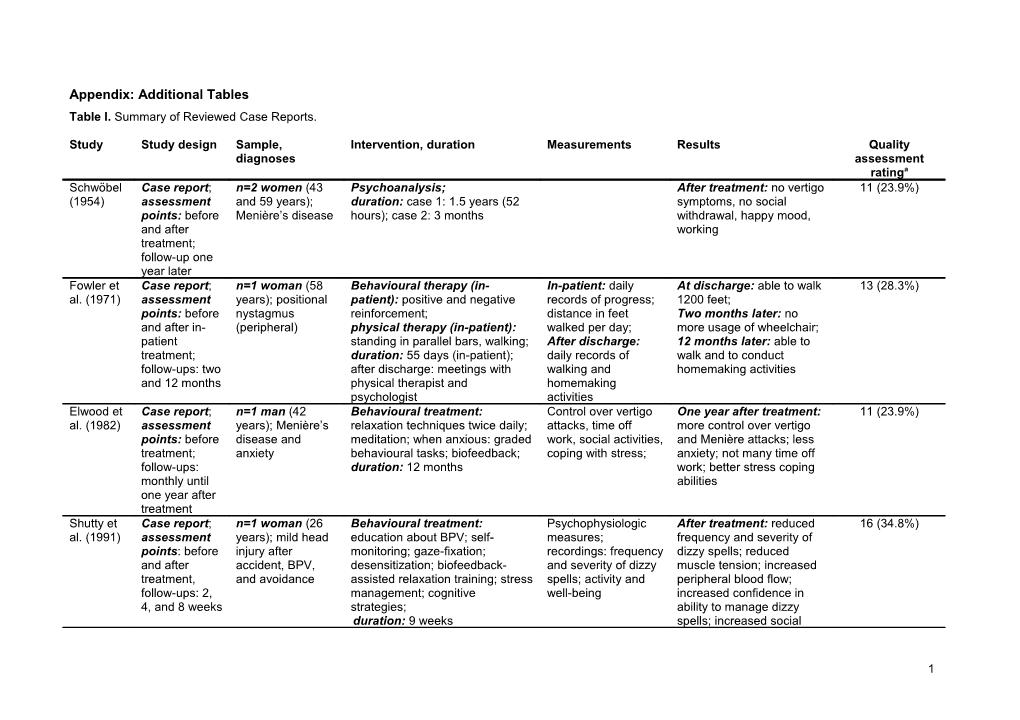
Appendix: Additional Tables Table I. Summary of Reviewed Case Reports.
Study Study design Sample, Intervention, duration Measurements Results Quality diagnoses assessment ratinga Schwöbel Case report; n=2 women (43 Psychoanalysis; After treatment: no vertigo 11 (23.9%) (1954) assessment and 59 years); duration: case 1: 1.5 years (52 symptoms, no social points: before Menière’s disease hours); case 2: 3 months withdrawal, happy mood, and after working treatment; follow-up one year later Fowler et Case report; n=1 woman (58 Behavioural therapy (in- In-patient: daily At discharge: able to walk 13 (28.3%) al. (1971) assessment years); positional patient): positive and negative records of progress; 1200 feet; points: before nystagmus reinforcement; distance in feet Two months later: no and after in- (peripheral) physical therapy (in-patient): walked per day; more usage of wheelchair; patient standing in parallel bars, walking; After discharge: 12 months later: able to treatment; duration: 55 days (in-patient); daily records of walk and to conduct follow-ups: two after discharge: meetings with walking and homemaking activities and 12 months physical therapist and homemaking psychologist activities Elwood et Case report; n=1 man (42 Behavioural treatment: Control over vertigo One year after treatment: 11 (23.9%) al. (1982) assessment years); Menière’s relaxation techniques twice daily; attacks, time off more control over vertigo points: before disease and meditation; when anxious: graded work, social activities, and Menière attacks; less treatment; anxiety behavioural tasks; biofeedback; coping with stress; anxiety; not many time off follow-ups: duration: 12 months work; better stress coping monthly until abilities one year after treatment Shutty et Case report; n=1 woman (26 Behavioural treatment: Psychophysiologic After treatment: reduced 16 (34.8%) al. (1991) assessment years); mild head education about BPV; self- measures; frequency and severity of points: before injury after monitoring; gaze-fixation; recordings: frequency dizzy spells; reduced and after accident, BPV, desensitization; biofeedback- and severity of dizzy muscle tension; increased treatment, and avoidance assisted relaxation training; stress spells; activity and peripheral blood flow; follow-ups: 2, management; cognitive well-being increased confidence in 4, and 8 weeks strategies; ability to manage dizzy duration: 9 weeks spells; increased social
1 activities; less psychological distress; Follow-ups: increased activity and well-being Andersson Case report; n=1 woman (68 CBT and VR: education about Questionnaire: After treatment: 18.5 (40.2%) & Yardley assessment years); dizziness, dizziness; balance / movement VHS; neuro- improved balance, (1998) points: before fear of falling, and exercises; relaxation for difficult otological testing: equilibrium score, and and after avoidance situations; positive / negative eye movements, behaviour provocation; treatment; thoughts; vicious circles; reflexes, caloric test, Pre to post to follow-up: follow-up: expectations; dynamic Improved VHS three months duration: 10 weeks (five posturography; sessions, one phone call) behaviour provocation test Hägnebo Case report; n=1 woman (62 CBT: relaxation training; Clinical interview; After treatment: no more 19 (41.3%) et al. assessment years); Menière’s desensitization of anxiety- recordings: number vertigo attacks; (1998) points: before disease and provoking situations; cognitive of vertigo attacks and At 24 months: no more and after anxiety / worries restructuring; behavioural task of positive / negative vertigo attacks; normal treatment; setting; enhancement of bodily events social functioning, less follow-ups: 3, awareness; worries 6, 10, and 24 duration: 9 weeks (in addition: 2 months Booster sessions at 6 months after treatment) Sareen Case report, n=1 woman (35 Behavioural treatment: episodes of dizziness After treatment: no more 9 (19.6%) (2003) assessment years); dizziness, education about dizziness; daily dizziness; points: before anxiety, and exposure to dizziness; Follow-up: maintained and after avoidance Duration: 4 sessions improvement treatment; follow-up: 6 months Whitney et Case report; n=1 man (37 Behavioural therapy: exposure Expert interview; After behavioural 17.5 (38.0%) al. (2005) assessment years); fear of to virtual height scenes; questionnaires: therapy: reduced anxiety points: before heights and duration: 8 sessions; CAQ, ATHQ, SitQ, and avoidance of heights; treatment, dizziness Followed by vestibular therapy: IIRS, DHI; SF-36, increased quality of life; after exercises; duration: 8 weeks behavioural persistent symptoms of behavioural avoidance test; dizziness and discomfort of therapy and optic flow testing space and motion; after vestibular After vestibular therapy: therapy reduced anxiety and avoidance of heights; less
2 perceived dizziness handicap; less visually dependent; improved quality of life; better daily functioning Goto et al. Case report; n=1 man (51 Psychotherapy and AT (three Questionnaires: After a few weeks: no 13 (28.3%) (2008a) assessment years); Menière’s times daily); duration: 6 SDS, STAI, CMI, Y-G more vertigo, tinnitus, and points: before disease, anxiety, sessions, every three weeks insomnia; and during and insomnia At follow-ups: no more treatment; vertigo and insomnia follow-ups: 6 and 9 months Goto et al. Case report; n=1 woman (37 Medication: antidepressant, Questionnaires: After 2 weeks: symptoms 13 (28.3%) (2008b) assessment years); PPV, herbal medicine; SDS, STAI, CMI, slightly improved, points: before anxiety, insomnia, Psychotherapy and AT (three MAS, MOCI medication was stopped; and during headache, and times daily); duration: 6 sessions After a few weeks: no treatment; tinnitus (à 45 minutes), every three weeks more dizziness, insomnia, follow-ups: 6 and headache; and 9 months Follow-ups: no more dizziness, insomnia, and headache Sardinha Case report; n=1 man (17 Cognitive-behavioural therapy: Patient’s reports: At the end of treatment: 11 (23.9%) et al. assessment years); vestibular cognitive interventions, making frequency and no more dizziness, (2009) points: before neuritis and plans for the future, information intensity of dizziness increased activities and and during subsequently PPV about associations between episodes, anxiety, well-being treatment avoidance / hypervigilance and mood, well -being, problem maintenance, increase of activities activities, exposure to avoided activities; duration: 18 weeks (one session per week) a The quality assessment rating score (Moncrieff et al., 2001) could range between 0 (very poor study quality) and 46 (excellent study quality); in parentheses the proportion (in per cent) is reported. Abbreviations: AT=autogenic training; ATHQ=Attitudes Towards Heights Questionnaire; BPV=benign positional vertigo; CAQ=Cohen Acrophobia Questionnaire; CBT=Cognitive-behavioural therapy; CMI=Cornell Medical Index; IIRS=Illness Intrusiveness Ratings Scale; DHI=Dizziness Handicap Inventory; MAS=Manifest Anxiety Scale; MI=Mobility Inventory; MOCI=Maudsley Obsessional-Compulsive Inventory; PPV=Phobic postural vertigo; SitQ=Situational Characteristics Questionnaire; SDS=Self-rating Depression Scale; STAI(-t)=State-Trait Anxiety Inventory (trait form); VHS=Vertigo Handicap Scale; VR=vestibular rehabilitation; Y-G=Yatabe-Guilford personality test
3 Table II. Summary of Reviewed Psychotherapy or Follow-up Studies.
Study Study design Sample, diagnoses Control Intervention, duration Measurements Results Quality group assessment ratinga Huppert et Follow-up N=303 were sent a No Initial: self-controlled Self-reported Symptom-free or 21 (45.7%) al. (2005) study; questionnaire behavioural therapy: changes: considerably assessment n=106 (35%) explanation of PPV; symptom-free / improved: 75%, points: before completed it (n=42 decoupling of catastrophic considerably independently of treatment; women, n=64 men; thoughts; exposure to improved, no age, sex, prior follow-up: 5 to mean age 44.3 vertigo triggering change organic vertigo, or 15 years years); PPV situations; regular other subsequent physical activity; therapies; duration: 2-3 sessions; most improvement During follow-up within the first year period: psychotherapy after initial (not specified); treatment; pharmacotherapy, physiotherapy; alternative therapies; Heinrichs et Psychotherap Initially: n=398 No CBT (individualized): Questionnaires: After 6 weeks: 21.5 (46.7%) al. (2003) y study (natural (n=266 women, Information about the BAI, BDI, BSQ, improvement in all design); n=132 men; mean disorder and therapy ACQ, MI, SCL-90-R measurements; assessment age 35.5 years); procedure; intensive in- After one year: points: before vertigo and vivo exposure with anxiety effects remained treatment; agoraphobia triggering stimuli up to 12 stable follow-ups: 6 6 weeks post: hours daily; self-control weeks and one n=398 (100%) period; duration: > 3 year One year post: weeks n=300 (75.4%) a The quality assessment rating score (Moncrieff et al., 2001) could range between 0 (very poor study quality) and 46 (excellent study quality); in parentheses the proportion (in per cent) is reported. Abbreviations: ACQ=Agoraphobic Cognitions Questionnaire; BAI=Beck Anxiety Inventory; BDI=Beck Depression Inventory; BSQ=Body Sensation Questionnaire; CBT=Cognitive-behavioural therapy; MI=Mobility Inventory; PPV=Phobic postural vertigo; SCL-90(-R)=Symptom Checklist 90 (revised);
4