Contingencies of UTX/KDM6A Action in Urothelial Carcinoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download (843Kb)
DIPLOMARBEIT Titel der Diplomarbeit ELFRIEDE OTT UND DIE SCHAUSPIELKUNST – Schauspieltechniken im Vergleich Verfasserin Corinna Pumm Angestrebter akademischer Grad Magistra der Philosophie (Mag.phil) Wien, 2015 Studienkennzahl lt. Studienblatt: A 317 Studienrichtung lt. Studienblatt: Theater- Film- und Medienwissenschaft Beutreuer: Mag. Dr. Monika Meister 1 Ehrenwörtliche Erklärung Ich erkläre ehrenwörtlich, dass ich die vorliegende wissenschaftliche Arbeit selbstständig angefertigt und die mit ihr unmittelbar verbundenen Tätigkeiten selbst erbracht habe. Ich erkläre weiters, dass ich keine anderen als die angegebenen Hilfsmittel benutzt habe. Alle ausgedruckten, ungedruckten oder dem Internet im Wortlaut oder im wesentlichen Inhalt übernommenen Formulierungen und Konzepte sind gemäß den Regeln für wissenschaftliche Arbeiten zitiert und durch Fußnoten bzw. durch andere genaue Quellenangaben gekennzeichnet. Die während des Arbeitsvorganges gewährte Unterstützung einschließlich signifikanter Betreuungshinweise ist vollständig angegeben. Die wissenschaftliche Arbeit ist noch keiner anderen Prüfungsbehörde vorgelegt worden. Diese Arbeit wurde in gedruckter und elektronischer Form abgegeben. Ich bin mir bewusst, dass eine falsche Erklärung rechtliche Folgen haben wird. Corinna Pumm Wien, 21. Mai 2014 2 Inhaltsverzeichnis 1. Einleitung ……………………………………………………………………. 7 2. Begriffsklärungen ........................................................................................................ 10 2.1. Geschichtliche Entwicklung des Theaters und -

Tag Des Barrierefreien Tourismus PROGRAMM
Tag des barrierefreien Tourismus Accessible Tourism Day PROGRAMM SCHEDULE 12.03.2021 10:15 – ca. 15:30 Online per Die Anmeldung zu dieser ZOOM Fachveranstaltung erfolgt unter: To register for this professional event, please visit: www.germany.travel/tdbt Supported by © DZT/Jens Wegener © DZT/Jens Anzeige•Advertisement Anzeige GRUSSWORT | A MESSAGE Leichter Reisen Barrierefreie Urlaubsziele in Deutschland Urlaub für Alle in zehn deutschen Regionen: Liebe Leserinnen Eifel und Leser, Erfurt Fränkisches Seenland Barrierefreiheit ist für etwa 10 Prozent der Bevölkerung unentbehrlich, aber für 100 Lausitzer Seenland Prozent der Reisenden komfortabel. Die Magdeburg Teilhabe aller Menschen am Tourismus ist Ostfriesland ein Element von Lebensqualität. „Reisen für Alle“ besitzt damit durchaus ökonomisches Rostock Potenzial für das Reiseland Deutschland. In Ruppiner Seenland den Eckpunkten für eine nationale Touris- musstrategie hat die Bundesregierung be- Sächsische Schweiz schlossen, dass Barrierefreiheit zu den stra- Südliche Weinstraße tegischen Zielen gehört, die wir weiterhin engagiert voranbringen wollen. Wir engagieren uns rund um Ihren Aufenthalt, damit Sie unsere Regionen genießen können. Nutzen Sie unsere barrierefreien Angebote. „Die Teilhabe aller Menschen www.leichter-reisen.info am Tourismus ist ein Element Urlaub für Alle von Lebensqualität.“ in zehn deutschen Regionen “Quality of life is enhanced if tourism is made accessible.” • • EIFEL ERFURT FRÄNKISCHES SEENLAND ROSTOCK THOMAS BAREIß MdB LAUSITZER SEENLAND • MAGDEBURG Dear reader, Parlamentarischer Staatssekretär • beim Bundesminister für Wirtschaft OSTFRIESLAND ROSTOCK OSTFRIESLAND und Energie und Beauftragter der RUPPINER SEENLAND • SÄCHSISCHE SCHWEIZ Accessibility is essential for around 10 per Bundesregierung für Tourismus und SÜDLICHE WEINSTRASSE RUPPINER SEENLAND cent of the population, but can make life für Mittelstand easier for every visitor. -

Demarcating Dramaturgy
Demarcating Dramaturgy Mapping Theory onto Practice Jacqueline Louise Bolton Submitted in accordance with the requirements for the degree of Doctor of Philosophy The University of Leeds Workshop Theatre, School of English August 2011 The candidate confirms that the work submitted is his/her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. 11 Acknowledgements This PhD research into Dramaturgy and Literary Management has been conducted under the aegis of an Arts and Humanities Research Council Collaborative Doctoral Award; a collaboration between the University of Leeds and West Yorkshire Playhouse which commenced in September 2005. I am extremely grateful to Alex Chisholm, Associate Director (Literary) at West Yorkshire Playhouse, and Professor Stephen Bottoms and Dr. Kara McKechnie at the University of Leeds for their intellectual and emotional support. Special thanks to Professor Bottoms for his continued commitment over the last eighteen months, for the time and care he has dedicated to reading and responding to my work. I would like to take this opportunity to thank everybody who agreed to be interviewed as part of this research. Thanks in particular to Dr. Peter Boenisch, Gudula Kienemund, Birgit Rasch and Anke Roeder for their insights into German theatre and for making me so welcome in Germany. Special thanks also to Dr. Gilli Bush-Bailey (a.k.a the delightful Miss. Fanny Kelly), Jack Bradley, Sarah Dickenson and Professor Dan Rebellato, for their faith and continued encouragement. -

German Videos - (Last Update December 5, 2019) Use the Find Function to Search This List
German Videos - (last update December 5, 2019) Use the Find function to search this list Aguirre, The Wrath of God Director: Werner Herzog with Klaus Kinski. 1972, 94 minutes, German with English subtitles. A band of Spanish conquistadors travels into the Amazon jungle searching for the legendary city of El Dorado, but their leader’s obsessions soon turn to madness.LLC Library CALL NO. GR 009 Aimée and Jaguar DVD CALL NO. GR 132 Ali: Fear Eats the Soul Director: Rainer Werner Fassbinder. with Brigitte Mira, El Edi Ben Salem. 1974, 94 minutes, German with English subtitles. A widowed German cleaning lady in her 60s, over the objections of her friends and family, marries an Arab mechanic half her age in this engrossing drama. LLC Library CALL NO. GR 077 All Quiet on the Western Front DVD CALL NO. GR 134 A/B Alles Gute (chapters 1 – 4) CALL NO. GR 034-1 Alles Gute (chapters 13 – 16) CALL NO. GR 034-4 Alles Gute (chapters 17 – 20) CALL NO. GR 034-5 Alles Gute (chapters 21 – 24) CALL NO. GR 034-6 Alles Gute (chapters 25 – 26) CALL NO. GR 034-7 Alles Gute (chapters 9 – 12) CALL NO. GR 034-3 Alpen – see Berlin see Berlin Deutsche Welle – Schauplatz Deutschland, 10-08-91. [ Opening missing ], German with English subtitles. LLC Library Alpine Austria – The Power of Tradition LLC Library CALL NO. GR 044 Amerikaner, Ein – see Was heißt heir Deutsch? LLC Library Annette von Droste-Hülshoff CALL NO. GR 120 Art of the Middle Ages 1992 Studio Quart, about 30 minutes. -

Spielzeit 1961–1970
MAXIM GORKI THEATER 1961 - 1970 Intendant Maxim Vallentin (von 1952 bis 1968) noch Spielzeit 1960/61 DER ZERBROCHENE KRUG von Heinrich von Kleist Regie: Maxim Vallentin Ausstattung: Dieter Berge Musik: Günter Hauk mit Alfred Müller (Walter, Gerichtsrat), Kurt Steingraf (Adam, Dorfrichter), Willi Narloch (Licht), Friedel Nowack (Frau Marthe Rull), Ursula Karusseit (Eve), Manfred Borges (Ruprecht), Lotte Loebinger (Frau Brigitte), Kurt Böwe (Ein Bedienter) u. a. Premiere am 17.02.1961 DIE SPIELDOSE von Georg Kaiser Regie: Horst Schönemann Ausstattung: Dieter Berge mit Albert Hetterle (Pierre Chaudraz), Heinz Scholz (Parmelin), Ruth-Maria Kemper (Noelle), Uwe-Detlev Jessen (Paul Chaudraz) Premiere am 06.06.1961 Spielzeit 1961/62 RUMMELPLATZ von Ewan McColl Regie: Hans Dieter Mäde Ausstattung: Dieter Berge Musik: Günter Hauk mit Hellmut Müller-Lankow (Turk), Jochen Thomas (Moran), Kurt Böwe (Ernie Flowers), Jutta Hoffmann (Sandra), Sabine Krug (Moll), Willi Narloch (Joe), Lotte Loebinger (Turks Mutter), Marga Legal (Stella) u. a. Uraufführung am 12.10.1961 SCHATTEN EINES MÄDCHENS von Rainer Kerndl Regie: Horst Schönemann Ausstattung: Eva Stengel mit Kurt Steingraf (Karl Heilmann), Friedel Nowack (Frau Heilmann), Alfred Müller (Dieter), Uwe-Detlev Jessen (Ulrich), Maika Joseph (Frau Senefeld), Erik S. Klein(Maneczki), Ruth-Maria Kemper (Halina) Uraufführung am 21.10.1961 NACHTASYL von Maxim Gorki (Neuinszenierung) Regie: Maxim Vallentin Bühnenbild und Kostüme: Gerhard Schade/Dieter Berge mit Otfried Knorr (Kostylew), Brigitte Lindenberg (Wassilissa), -

Norman Schenk
Norman Schenk http://www.normanschenk.de/ Agentur Mosblech Andreas Denker Phone: +49 172 3018 349 Email: [email protected] Website: http://www.agenturmosblech.de © studiofaktum Information Acting age 32 - 45 years Nationality German Year of birth 1969 Languages German: native-language Height (cm) 172 English: basic Weight (in kg) 68 Russian: basic Eye color blue Dialects Saxon Hair color Blond Berlin German Hair length Medium Instruments Guitar: medium Stature athletic / training Sport Sailing, Fencing (sports) Place of residence Berlin Profession Actor Housing options Dresden, Köln, Leipzig, Pitch Baritone München, Osterburg, Berlin Other Education & Training 1990 –… Schauspielstudium Theaterhochschule "Hans Otto", Leipzig Film 2011 Die Männer der Emden Role: Supporting role Director: Berengar Pfahl 2011 Magier Role: Leading role Director: Tom Schildberg Kurzfilm in 3D 2007 Der Baader Meinhof Komplex Role: Supporting role Director: Uli Edel Distribution: Constantin Film 2007 Narrenspiel Role: Leading role Director: Markus F. Adrian Distribution: HFF "Konrad Wolf"& ARTE 2000 Die Unberührbare Role: Supporting role Director: Oskar Roehler Distribution: Distant Dreams Produktion 1998 Der Liebhaber Role: Supporting role Director: Claudia Bachmann Distribution: DffB Television Vita Norman Schenk by www.castupload.com — As of: 2021-09-06 Page 1 of 3 2009 Der Westflug - Eine Entführung aus Liebe Role: Supporting role Director: Thomas Jauch TV Channel: RTL 2008 Mörder kennen keine Grenzen Role: Supporting role Director: Jorgo Papavassiliou TV Channel: Sat.1 2008 Polizeiruf 110 "Verdammte Sehnsucht" Role: Supporting role Director: Bodo Fürneisen TV Channel: ARD RBB 2001 Liebes Au, die andere Heimat Role: durchgehende Rolle (Serie/Reihe) (LR) Director: Wolfgang Panzer TV Channel: ZDF 1999 Eden Role: Leading role Director: Riccardo Signorell SF DRS 1997 Das ewige Lied Role: Leading role Director: Franz X. -

COVID – 19 European Measures Version 11
COVID – 19 European measures Version 11. Date: 27-05-2020 Contents Introduction 03 Albania 05 Austria 09 Belgium 11 Bosnia and Herzegovina 14 Bulgaria 20 Croatia 23 Czech Republic 26 Finland 29 France 31 Germany 34 Hungary 40 Ireland 42 Italy 45 Kosovo 48 Lithuania 50 Netherlands 52 Norway 53 Poland 56 Portugal 59 Romania 64 Serbia 69 Slovakia 72 Slovenia 74 Sweden 76 Switzerland 78 United Kingdom 81 All countries information is updated until 27.05.2020 (The information relating to the UK measures is as of 20 May 2020) Country Contacts Serbia Switzerland Albania Croatia Hungary Netherlands Dejan Mrakovic Juerg Birri Olindo Shehu Tarja Krehic Laszlo Winkler Peter Kits Email: [email protected] Email: [email protected] Email: [email protected] Email: [email protected] Email: [email protected] Email: [email protected] Stefan Antonic Christine Bassanello Sabina Lalaj Mihaly Harcos Frederieke Leeflang Email: [email protected] Email: [email protected] Email: [email protected] Email: [email protected] Email: [email protected] Czech Republic Igor Dencic Email: [email protected] Martin Bohuslav United Kingdom Austria Email: [email protected] Ireland Norway Rachel Hossack Alexander Lang Joanne Whelan Mari Wetlesen Slovakia Email: [email protected] Email: [email protected] Email: [email protected] Email: [email protected] Finland Lubica Dumitrescu Bernhard Köck Peder Brondmo Email: [email protected] Email: [email protected] Vesa Karvonen Email: [email protected] -

Nathan Der Weise Gotthold Ephraim Lessing (1729-1781)
1/6 Data Nathan der Weise Gotthold Ephraim Lessing (1729-1781) Langue : Allemand Genre ou forme de l’œuvre : Œuvres textuelles Date : 1779 Note : Pièce de théâtre philosophique sur le thème de la tolérance Domaines : Littératures Autres formes du titre : Natán el Sabio (espagnol; castillan) Nathan le Sage (français) Éditions de Nathan der Weise (36 ressources dans data.bnf.fr) Livres (27) G. E. Lessing. Nathan der , Gotthold Ephraim Lessing Nathan le sage, drame en , Gotthold Ephraim Lessing Weise (1729-1781), Zürich, cinq actes (1729-1781), (S. l. n. d.) Schulthess , (s. d.). In-16 (190 x 130), 151 p. [Don 338682] -XcTh- Nathan le sage , Gotthold Ephraim Lessing Natán el Sabio. - de Gothold Ephraim Lessing. - [1] (2006) (1729-1781), [Paris] : (2003) Gallimard , impr. 2006 Nathan der Weise , Gotthold Ephraim Lessing Nathan le Sage , Gotthold Ephraim Lessing (1998) (1729-1781), Stuttgart : P. (1997) (1729-1781), Arles : Actes Reclam jun. , 1998 Sud , 1997 Nathan le Sage , Gotthold Ephraim Lessing Nathan der weise. - [3] (1997) (1729-1781), Paris : (1993) Flammarion , 1997 Nathan le Sage , Gotthold Ephraim Lessing Nathan le Sage , Gotthold Ephraim Lessing (1993) (1729-1781), Paris : Aubier (1991) (1729-1781), Paris : J. Corti , 1993 , 1991 Nathan der Weise.. - [1] Nathan le Sage , Gotthold Ephraim Lessing (1979) (1954) (1729-1781), Paris : Aubier , DL 1954 data.bnf.fr 2/6 Data Nathan der Weise, ein , Gotthold Ephraim Lessing Nathan der Weise, ein , Gotthold Ephraim Lessing dramatisches gedicht. (1729-1781), Offenburg : dramatisches Gedicht in (1729-1781), Berlin, Volk Herausgeber : Direction de Lehrmittel-Verlag , [1948] fünf Aufzügen und Wissen ; (Leipzig, l'Education publique (1946) Druck von Fischer und G.M.Z.F.O. -
2005 Next Wave Festival
October 2005 2005 Next Wave Festival Mary Heilmann, Last Chance for Gas Study (delail), 2005 BAM 2005 Next Wave Festival is sponsored by: The PerformingNeonEArts Magazine Altria 2005 ~ext Wa~e EeslliLaL Brooklyn Academy of Music Alan H. Fishman William I. Campbell Chairman of the Board Vice Chairman of the Board Karen Brooks Hopkins Joseph V. Melillo President Executive Prod ucer presents Emilia Gaiotti Approxi mate BAM Harvey Theater running time: Oct 12-15, 2005 at 7:30pm 1 hour, 15 minutes, no By Gotthold Ephraim Lessing interm ission Deutsches Theater Berlin Director Michael Thalheimer Set &costumes Olaf Altmann Music* Bert Wrede Viol in Steffen Tast Dramaturge Hans Nadolny Engl ish titles by Chris Bergen *based on "Yumei's Theme" by S. Umebayashi from Wong Kar Wai's movie, In the Mood for Love Cast Emilia Gaiotti Regine Zimmermann Odoardo Gaiotti, Emilia's Father Peter Pagel Claudia Gaiotti, Emilia's Mother Katrin Klein Hettore Gonzaga, Prince of Guastalla Sven Lehmann Marinelli, Gonzaga's Chamberlain Ingo Hulsmann Count Appiani, Emilia's Fiance Henning Vogt Countess Orsina, Gonzaga's Mistress Nina Hoss BAM 2005 Next Wave Festival is sponsored by Altria Group, Inc. Leadership support for BAM Theater is provided by The Shubert Foundation, with additional support from The SHS Foundation, The Harold and Mimi Steinberg Charitable Trust, and The Francena T. Harrison Foundation Trust. Emilia Galottj'--- _ Assistant directors Jarn Weisbrodt, Malte Lamprecht Stage manager Frank Ulbig Prompter Marion Rommel Technical director Olaf Grambow Technical equipment Jarg Luxath Lighting Thomas Langguth Sou nd Wolfgang Ritter Production of the sets and costumes through the stage service of the Berlin Opera Foundation. -
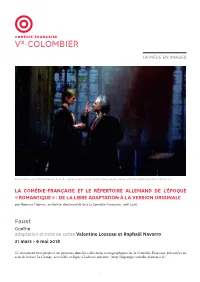
La Pièce En Images
LA PIÈCE EN IMAGES Anna Cervinka et Laurent Natrella dans Faust de Goethe, adaptation et mise en scène Valentine Losseau et Raphaël Navarro, 2018, photographie de répétition © Vincent Pontet LA COMÉDIE-FRANÇAISE ET LE RÉPERTOIRE ALLEMAND DE L’ÉPOQUE « ROMANTIQUE » : DE LA LIBRE ADAPTATION À LA VERSION ORIGINALE par Florence Thomas, archiviste-documentaliste à la Comédie-Française, avril 2018. Faust Goethe adaptation et mise en scène Valentine Losseau et Raphaël Navarro 21 mars > 6 mai 2018 Ce document vous propose un parcours dans les collections iconographiques de la Comédie-Française présentées au sein de la base La Grange, accessible en ligne à l’adresse suivante : http://lagrange.comedie-francaise.fr/ 1 LA COMÉDIE-FRANÇAISE ET LE RÉPERTOIRE ALLEMAND DE L’ÉPOQUE « ROMANTIQUE » : DE LA LIBRE ADAPTATION À LA VERSION ORIGINALE Le Sturm und Drang ou « Tempête et élan », mouvement Pendant la première moitié du XIXe siècle, le théâtre littéraire né vers 1770 en Allemagne en réaction à la allemand, alors connu par des traductions du milieu philosophie des Lumières et à la tragédie française, du XVIIIe siècle et très en vogue après la Révolution, nourrit le courant romantique qui gagne rapidement est un des principaux répertoires étrangers joué à la l’Europe au début du XIXe siècle. De nouveaux horizons Comédie-Française, et cela dans de libres adaptations, s’ouvrent aux auteurs et spectateurs qui découvrent passage obligé pour entrer au répertoire. Bien qu’il ait les dramaturges grâce aux échanges littéraires et été hostile tant au classicisme qu’au romantisme, August humains et, plus précisément, grâce aux adaptations. von Kotzebue est l’un des premiers auteurs allemands Leur histoire à la Comédie-Française est révélatrice de de la période dite romantique à être en 1799 présenté à l’attention portée au public du XIXe siècle à nos jours. -
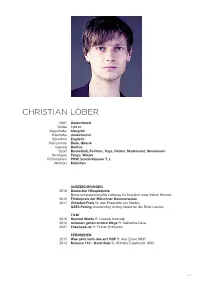
Christian Löber
CHRISTIAN LÖBER 1983* Deutschland Größe 1,91 m Augenfarbe blaugrün Haarfarbe dunkelblond Sprachen Englisch Instrumente Bass, Gitarre Gesang Bariton Sport Basketball, Fechten, Yoga, Reiten, Skateboard, Snowboard Sonstiges Tango, Walzer Führerschein PKW, Sonderklassen T, L Wohnort München AUSZEICHNUNGEN 2016 Deutscher Hörspielpreis Beste schauspielerische Leistung für Draußen unter freiem Himmel 2015 Förderpreis der Münchner Kammerspiele 2011 Vontobel-Preis für das Ensemble von Helden GATS Peking Outstanding Acting Award für die Rolle Leonce FILM 2016 Beyond Words R: Urszula Antoniak 2010 Ameisen gehen andere Wege R: Catharina Deus 2007 Fakebook.de R: Florian Schneider FERNSEHEN 2015 Was geht mich das an? RAF R: Ana Zirner WDR 2013 Monaco 110 - Hotel Bubi R: Wilhelm Engelhardt ARD 1/2 CHRISTIAN LÖBER THEATER Auswahl seit 2012 Münchner Kammerspiele Die Selbstmord-Schwestern R: Susanne Kennedy Der Kirschgarten R: Nicolas Stemann Hot Pepper, Air Conditioner and the Farewell Speech R: Toshiki Okada 50 Grades of Shame R: She She Pop Mutter Courage und ihre Kinder R: Thomas Schmauser Nichts von euch auf Erden R: Felix Rothenhäusler Rocco und seine Brüder R: Simon Stone Jagdszenen aus Niederbayern R: Martin Kušej The Rest is Noise R: Johan Simons Country Kitchen R: Erik de Quero Totally happy R: Tian Gebing Liliom R: Stephan Kimmig Seltsames Intermezzo Gorden Evans R: Ivo van Hove 2015, 2014, 2013 Theatertreffen Berlin / Münchner Kammerspiele Warum läuft Herr R. Amok? R: Susanne Kennedy Fegefeuer in Ingolstadt R: Susanne Kennedy Orpheus steigt herab R: Sebastian Nübling Franziska R: Andreas Kriegenburg 2012 Kunstfestspiele Herrenhausen Geometrie der Liebe Pietro R: Alexander Charim Hans Otto Theater Potsdam Das Spiel von Liebe und Zufall Dorante R: Jutta Hoffman 2010, 2011 Bat Studiotheater Berlin Leonce & Lena Leonce R: Alexander Lang Helden David R: Roscha A. -

Article Contingencies of UTX/KDM6A Action in Urothelial Carcinoma
Article Contingencies of UTX/KDM6A Action in Urothelial Carcinoma Alexander Lang 1, Merve Yilmaz 1, Christiane Hader 1, Sammy Murday 1, Xenia Kunz 1, Nicholas Wagner 1, Constanze Wiek 2, Patrick Petzsch 3, Karl Köhrer 3, Julian Koch 4, Michéle J. Hoffmann 1, Annemarie Greife 4 and Wolfgang A. Schulz 1,* 1 Department of Urology, Medical Faculty, Heinrich Heine University, 40225 Düsseldorf, Germany; [email protected] (A.L.); [email protected] (M.Y.); [email protected] (C.H.); [email protected] (S.M.); [email protected] (X.K.); [email protected] (N.W.); [email protected] (M.J.H.) 2 Department of Otolaryngology, Medical Faculty, Heinrich Heine University Düsseldorf, 40225 Düsseldorf, Germany; [email protected] 3 Biological and Medical Research Centre (BMFZ), Heinrich Heine University Düsseldorf, 40225 Düsseldorf, Germany; [email protected] (P.P.); [email protected] (K.K.) 4 Chair for Molecular Physical Chemistry, Heinrich Heine University Düsseldorf, 40225 Düsseldorf, Germany; [email protected] (J.K.); [email protected] (A.G.) * Correspondence: [email protected]; Tel.: +49-211-81-15845 Received: 28 February 2019; Accepted: 2 April 2019; Published: 4 April 2019 Abstract: The histone demethylase Ubiquitously Transcribed Tetratricopeptide Repeat Protein X- Linked (UTX/KDM6A) demethylates H3K27me2/3 at genes and enhancers and is often inactivated by mutations in urothelial carcinoma (UC). The consequences of its inactivation are however poorly understood. We have investigated the consequences of moderate UTX overexpression across a range of UC cell lines with or without mutations in KDM6A or its interaction partners and in a normal control cell line.