Tuberculosis and Tuberculin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Genetic Basis of Interindividual Variability in the Course of Infection
Human genetic basis of interindividual variability in the course of infection Jean-Laurent Casanovaa,b,c,d,e,1 aSt. Giles Laboratory of Human Genetics of Infectious Diseases, Rockefeller Branch, The Rockefeller University, New York, NY 10065; bHoward Hughes Medical Institute, New York, NY 10065; cLaboratory of Human Genetics of Infectious Diseases, Necker Branch, Inserm U1163, Necker Hospital for Sick Children, 75015 Paris, France; dImagine Institute, Paris Descartes University, 75015 Paris, France; and ePediatric Hematology and Immunology Unit, Assistance Publique–Hôpitaux de Paris, Necker Hospital for Sick Children, 75015 Paris, France This contribution is part of the special series of Inaugural Articles by members of the National Academy of Sciences elected in 2015. Contributed by Jean-Laurent Casanova, November 2, 2015 (sent for review September 15, 2015; reviewed by Max D. Cooper and Richard A. Gatti) The key problem in human infectious diseases was posed at the immunity (cell-autonomous mechanisms), then of cell-extrinsic turn of the 20th century: their pathogenesis. For almost any given innate immunity (phagocytosis of pathogens by professional cells), virus, bacterium, fungus, or parasite, life-threatening clinical disease and, finally, of cell-extrinsic adaptive immunity (somatic di- develops in only a small minority of infected individuals. Solving this versification of antigen-specific cells). Understanding the patho- infection enigma is important clinically, for diagnosis, prognosis, genesis of infectious diseases, particularly -
The T-SPOT.TB Test Frequently Asked Questions
General tuberculosis information T-SPOT.TB Test description and Frequently asked performance questions T-SPOT.TB Test performance characteristics T-SPOT.TB advantages over tuberculin skin test T-SPOT.TB test results T-SPOT.TB methodology Screening control programs Contact investigations References References Table of contents General tuberculosis information Tuberculosis: Definition, infection and disease 1. What is the scale of the TB problem? 2. How is TB spread? 3. What is TB infection (Latent Tuberculosis Infection “LTBI” or “latent TB”)? 4. What is TB disease (“active TB”)? 5. Are certain groups of individuals at an increased risk of exposure to Mycobacterium tuberculosis? 6. Are certain individuals at an increased risk of progressing from latent TB infection to TB disease? 7. How important is treatment for TB disease? 8. Why is the treatment period for TB disease so long? 9. How important is treatment for TB infection (“LTBI” or “latent TB”)? TB detection 10. Is there a test for the detection of TB infection (“LTBI” or “latent TB”)? • Tuberculin Skin Test (TST) • Interferon-Gamma Release Assays (IGRA) 11. Is there a test for the detection of TB disease (“active TB”)? 12. What are the limitations of the TST? Bacille Calmette-Guérin (BCG) vaccination 13. What is the BCG vaccination? T-SPOT.TB test description and performance 14. What is the intended use of the T-SPOT.TB test? 15. Why does the T-SPOT.TB test measure interferon-gamma? 16. Does the T-SPOT.TB test differentiate between latent TB infection and TB disease? 17. What data is there to support the T-SPOT.TB test in clinical use? 18. -

Faqs 1. What Is a 2-Step TB Skin Test (TST)? Tuberculin Skin Test (TST
FAQs 1. What is a 2-step TB skin test (TST)? Tuberculin Skin Test (TST) is a screening method developed to evaluate an individual’s status for active Tuberculosis (TB) or Latent TB infection. A 2-Step TST is recommended for initial skin testing of adults who will be periodically retested, such as healthcare workers. A 2 step is defined as two TST’s done within 1month of each other. 2. What is the procedure for 2-step TB skin test? Both step 1 and step 2 of the 2 step TB skin test must be completed within 28 days. See the description below. STEP 1 Visit 1, Day 1 Administer first TST following proper protocol A dose of PPD antigen is applied under the skin Visit 2, Day 3 (or 48-72 hours after placement of PPD) The TST test is read o Negative - a second TST is needed. Retest in 1 to 3 weeks after first TST result is read. o Positive - consider TB infected, no second TST needed; the following is needed: - A chest X-ray and medical evaluation by a physician is necessary. If the individual is asymptomatic and the chest X-ray indicates no active disease, the individual will be referred to the health department. STEP 2 Visit 3, Day 7-21 (TST may be repeated 7-21 days after first TB skin test is re ad) A second TST is performed: another dose of PPD antigen is applied under the skin Visit 4, 48-72 hours after the second TST placement The second test is read. -

Prior Tuberculin Skin Testing Does Not Boost Quantiferon-TB Results in Paediatric Contacts
REFERENCES 4 Aaron SD, Vandemheen KL, Fergusson D, et al. Tiotropium 1 Suissa S, Ernst P, Vandemheen KL, Aaron SD. in combination with placebo, salmeterol, or fluticasone– Methodological issues in therapeutic trials of COPD. Eur salmeterol for treatment of chronic obstructive pulmonary Respir J 2008; 31: 927–933. disease: a randomized trial. Ann Intern Med 2007; 146: 2 Sin DD, Wu L, Anderson JA, et al. Inhaled corticosteroids 545–555. 5 Wedzicha JA, Calverley PM, Seemungal TA, et al. The and mortality in chronic obstructive pulmonary disease. prevention of chronic obstructive pulmonary disease exacer- Thorax 2005; 60: 992–997. bations by salmeterol/fluticasone propionate or tiotropium 3 Calverley PM, Anderson JA, Celli B, et al. Salmeterol and bromide. Am J Respir Crit Care Med 2008; 177: 19–26. fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007; 356: 775–789. DOI: 10.1183/09031936.00030508 Prior tuberculin skin testing does not boost QuantiFERON-TB results in paediatric contacts To the Editors: children were evaluated with TST and QFT-GIT. At the first visit, 63 (77.8%) contacts were QFT-GIT negative, eight (9.9%) We read with interest the paper by LEYTEN et al. [1], which were QFT-GIT positive and 10 (12.3%) had an undetermined appeared in the June 2007 issue of the European Respiratory QFT-GIT. Of those initially negative children, only one became Journal (ERJ). LEYTEN et al. [1] showed that prior tuberculin skin QFT-GIT positive after TST. The mean IFN-c antigen-specific 1 tests (TST) do not induce false-positive QuantiFERON -TB production did not change 11 weeks after skin testing (ESAT-6/ Gold in-tube (QFT-GIT) assay results when evaluated in the CFP-10/TB7.7 difference -0.030 IU?mL-1,p50.281). -

Xii World Asthma, Allergy & Copd Forum
XII WORLD ASTHMA, ALLERGY & COPD FORUM Saint Petersburg, Russia June 29–July 2, 2019 SAINT PETERSBURG SAINT PROGRAM World Immunopathology XIII WORLD ASTHMA, Organization (WIPO) ALLERGY & COPD FORUM Saint-Petersburg, Russia July 2–5, 2020 General Information St. Pet The World Immunopathology Organization (WIPO) is a professional, non-profit organization. WIPO was created in December 2002, at the I World Congress on Immunopathology in Singapore. During these years, WIPO successfully organized many international congresses and regional and national meetings throughout See you in Saint Petersburg in 2020! the world all promoting basic and clinical research and giving an opportunity for exchanging ideas. WIPO is aimed at collecting and disseminating scientific information and providing training and continuous education in various fields of immunopathology. Aims and Mission Nowadays, immunopathology has become a multidisciplinary problem. The WIPO global mission is to promote through education and research activities worldwide: – basic and clinical research in experimental and clinical immunology, allergy and asthma, autoimmunity, immunodeficiency, AIDS, immunobiotechnology, – prevention and treatment of different manifestations of immunopathology—immune-associated disorders, – excellence in patient care in this very important area of medicine and to establish communication between specialists in various fields of medical science and practice. e We encourage to join WIPO national and regional societies as well as individual members—doctors -

The Decline in Mortality in Philadelphia from 1870 to 1930: the Role of Municipal Services
The Decline in Mortality in Philadelphia from 1870 to 1930: The Role of Municipal Services HE CHRISTMAS SEASON of 1880 should have been a happy occasion for Charles and Caroline Kautz. Charles, a German T immigrant in his mid-forties, had operated a three-person bakery in the Moyamensing section of Philadelphia over a decade. Caroline, several years his junior and his wife of over fifteen years, had married him during her teens and soon assumed the responsibilities of parenthood. Though Pennsylvania born, Caroline also came from German stock and, with her husband, worshipped at a loc&l German Lutheran church. Caroline and Charles Kautz and their three sons and three daughters must have eagerly anticipated a joyous holiday cele- bration. But it was not their fate to enjoy this Christmas. In three and one-half weeks from late November to mid-December, smallpox took the lives of five of the six Kautz children. Six-year-old Clara died on November 20, followed by Albert (aged 2) two weeks later, then Edward (aged 4) on December 10, Charles (aged 8) on December 11, and Bertha (aged 10) on December 14. Only twelve-year-old Sophia survived. Burial in the Lutheran church cemetery followed each of the deaths in numbing succession. The tragedies that befell the Kautzes over a century ago illustrate in a concrete way part of the enormous gap separating the twentieth and the nineteenth centuries in America. Epidemic diseases, childhood death, and low adult life expectancies dominated life. Indeed, in the space of a decade, the Kautzes had witnessed smallpox epidemics in Philadelphia in 1871-72 and 1876 prior to the 1880-81 epidemic that devastated their family. -

History of Tuberculosis and Tuberculosis Control Program in Turkey
In Focus History of tuberculosis and tuberculosis control program in Turkey Indian) and 4 (X, Haarlem, LAM [Latin-American Mediterranean]). In Turkey, the latest evolved lineage 4 has been most dominant. Current evidence might suggest migratory movements over the past 35,000–89,000 years from Africa spread four main lineages into Eurasia, while the remaining two phylogenetically ‘ancient’ lineages Cengiz Cavu¸ so¸ glu stayed in Africa. These lineages were later spread to the Sub-Indian Ege University Faculty of Medicine Department of Medical Microbiology continent and from there into Europe, sub-Saharan Africa and Mycobacteriology Laboratory America, following a wave of reverse Homo sapiens migrations and Bornova, Izmir,_ Turkey Email: [email protected] conquests. Analysis of known mutation rates of the M. tuberculosis reveals that the differences among strains started to appear 250– 1000 years ago3–9. Tuberculosis (TB) is debatably the most infectious disease Tuberculosis was initially documented over 5000 years ago in with highest rate of causalities throughout human history. Ancient Egypt; characteristic Pott deformations of TB were detected The Ottoman Empire also had the profound effect of the in mummies, and even represented in Ancient Egyptian art. disease; however, following the establishment of the Repub- Recently, DNA of M. tuberculosis was amplified from mummy lic of Turkey in 1923 effective TB control programs were tissues providing confirmatory evidence. There are documents implemented at times jointly with the WHO. From 1949 dating back 3300 years in India, and 2300 years in China and onwards, significant reduction in disease incidence and archaeological evidence from the Andes also confirm the existence death rates in Turkey was recorded due to the significant of pre-Columbian tuberculosis. -

GLOBAL TUBERCULOSIS REPORT 2018 Global Tuberculosis Report 2018
global TUBERCULOSIS REPORT 2018 GLOBAL TUBERCULOSIS REPORT 2018 Global Tuberculosis Report 2018 ISBN 978-92-4-156564-6 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY- NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Global tuberculosis report 2018. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. To submit requests for commercial use and queries on rights and licensing, see http://www.who.int/about/licensing. -
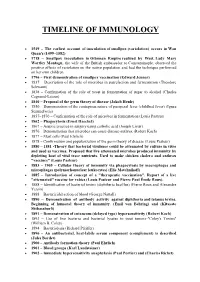
Timeline of Immunology
TIMELINE OF IMMUNOLOGY 1549 – The earliest account of inoculation of smallpox (variolation) occurs in Wan Quan's (1499–1582) 1718 – Smallpox inoculation in Ottoman Empire realized by West. Lady Mary Wortley Montagu, the wife of the British ambassador to Constantinople, observed the positive effects of variolation on the native population and had the technique performed on her own children. 1796 – First demonstration of smallpox vaccination (Edward Jenner) 1837 – Description of the role of microbes in putrefaction and fermentation (Theodore Schwann) 1838 – Confirmation of the role of yeast in fermentation of sugar to alcohol (Charles Cagniard-Latour) 1840 – Proposal of the germ theory of disease (Jakob Henle) 1850 – Demonstration of the contagious nature of puerperal fever (childbed fever) (Ignaz Semmelweis) 1857–1870 – Confirmation of the role of microbes in fermentation (Louis Pasteur) 1862 – Phagocytosis (Ernst Haeckel) 1867 – Aseptic practice in surgery using carbolic acid (Joseph Lister) 1876 – Demonstration that microbes can cause disease-anthrax (Robert Koch) 1877 – Mast cells (Paul Ehrlich) 1878 – Confirmation and popularization of the germ theory of disease (Louis Pasteur) 1880 – 1881 -Theory that bacterial virulence could be attenuated by culture in vitro and used as vaccines. Proposed that live attenuated microbes produced immunity by depleting host of vital trace nutrients. Used to make chicken cholera and anthrax "vaccines" (Louis Pasteur) 1883 – 1905 – Cellular theory of immunity via phagocytosis by macrophages and microphages (polymorhonuclear leukocytes) (Elie Metchnikoff) 1885 – Introduction of concept of a "therapeutic vaccination". Report of a live "attenuated" vaccine for rabies (Louis Pasteur and Pierre Paul Émile Roux). 1888 – Identification of bacterial toxins (diphtheria bacillus) (Pierre Roux and Alexandre Yersin) 1888 – Bactericidal action of blood (George Nuttall) 1890 – Demonstration of antibody activity against diphtheria and tetanus toxins. -

Mdr Tb Exposure Screening and Treatment Recommendations
Screening and Treatment Recommendations for People Exposed to Multidrug Resistant TB All people at increased risk of tuberculosis (TB) infection should be screened for TB infection per United States Preventive Services Task Force [1] and Centers for Disease Control and Prevention guidelines [2]. This document provides specific guidance for screening and post- screening management of all people who have been identified through public health investigations as having been exposed to multidrug resistant tuberculosis (MDR TB). Recommendations for symptomatic contacts, children less than 5 years of age and those who are highly immunocompromised (see step 1B) are different from other groups. Step 1: Initial Screening A. Assess contacts for symptoms of active TB disease ▪ Cough lasting 3 weeks or longer ▪ Contacts reporting cough of less than 3 weeks duration at the time of screening should have follow-up to determine if the cough has resolved. If they have a persistent cough for greater than or equal to 3 weeks, further evaluation is indicated. ▪ Hemoptysis (coughing up blood) ▪ Chest pain ▪ Night sweats ▪ Fevers or chills ▪ Unintentional weight loss ▪ Loss of appetite ▪ Fatigue B. Obtain a medical history including prior TB screening and TB treatment information ▪ Contacts with prior positive tuberculin skin test (TST) or interferon-gamma release assay (IGRA) results (documentation of previous testing is recommended) do not need a new TST or IGRA performed; they should be considered to have a positive TB screening test. In the event a person with a past positive TST or IGRA has a new TST or IGRA performed and it is negative, the significance of the new screening test is uncertain. -

White Plague, White City: Landscape and the Racialization of Tuberculosis in Washington, D.C
W&M ScholarWorks Undergraduate Honors Theses Theses, Dissertations, & Master Projects 4-2019 White Plague, White City: Landscape and the Racialization of Tuberculosis in Washington, D.C. from 1846 to 1960 Ivie Orobaton Follow this and additional works at: https://scholarworks.wm.edu/honorstheses Part of the African American Studies Commons, Social History Commons, and the United States History Commons Recommended Citation Orobaton, Ivie, "White Plague, White City: Landscape and the Racialization of Tuberculosis in Washington, D.C. from 1846 to 1960" (2019). Undergraduate Honors Theses. Paper 1378. https://scholarworks.wm.edu/honorstheses/1378 This Honors Thesis is brought to you for free and open access by the Theses, Dissertations, & Master Projects at W&M ScholarWorks. It has been accepted for inclusion in Undergraduate Honors Theses by an authorized administrator of W&M ScholarWorks. For more information, please contact [email protected]. 1 TABLE OF CONTENTS Page Introduction: Why Tuberculosis? Why Washington, D.C.?......................................................3-7 Chapter 1: The Landscape of Washington, D.C. and the Emergence of Tuberculosis in the City …………………………………………………………………………………………………8-21 Chapter 2: Practical Responses to the Tuberculosis Issue (1846-1910)…………………….22-37 Chapter 3: Ideological Debates Around the Practical Responses to Tuberculosis (1890-1930) …….………………………………………………………………………………………….38-56 Conclusion: The Passing of the Debate and the End of Tuberculosis in the City (1930-1960) ………………………………………….…………………………………………………….57-58 -

Hans Asperger, National Socialism, and “Race Hygiene” in Nazi-Era Vienna Herwig Czech
Czech Molecular Autism _#####################_ https://doi.org/10.1186/s13229-018-0208-6 RESEARCH Open Access Hans Asperger, National Socialism, and “race hygiene” in Nazi-era Vienna Herwig Czech Abstract Background: Hans Asperger (1906–1980) first designated a group of children with distinct psychological characteristics as ‘autistic psychopaths’ in 1938, several years before Leo Kanner’s famous 1943 paper on autism. In 1944, Asperger published a comprehensive study on the topic (submitted to Vienna University in 1942 as his postdoctoral thesis), which would only find international acknowledgement in the 1980s. From then on, the eponym ‘Asperger’s syndrome’ increasingly gained currency in recognition of his outstanding contribution to the conceptualization of the condition. At the time, the fact that Asperger had spent pivotal years of his career in Nazi Vienna caused some controversy regarding his potential ties to National Socialism and its race hygiene policies. Documentary evidence was scarce, however, and over time a narrative of Asperger as an active opponent of National Socialism took hold. The main goal of this paper is to re-evaluate this narrative, which is based to a large extent on statements made by Asperger himself and on a small segment of his published work. Methods: Drawing on a vast array of contemporary publications and previously unexplored archival documents (including Asperger’s personnel files and the clinical assessments he wrote on his patients), this paper offers a critical examination of Asperger’s life, politics, and career before and during the Nazi period in Austria. Results: Asperger managed to accommodate himself to the Nazi regime and was rewarded for his affirmations of loyalty with career opportunities.