Introducing Th E First Step-By-Step Rehabilitation Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Effects of Antipsychotic Treatment on Metabolic Function: a Systematic Review and Network Meta-Analysis
The effects of antipsychotic treatment on metabolic function: a systematic review and network meta-analysis Toby Pillinger, Robert McCutcheon, Luke Vano, Katherine Beck, Guy Hindley, Atheeshaan Arumuham, Yuya Mizuno, Sridhar Natesan, Orestis Efthimiou, Andrea Cipriani, Oliver Howes ****PROTOCOL**** Review questions 1. What is the magnitude of metabolic dysregulation (defined as alterations in fasting glucose, total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and triglyceride levels) and alterations in body weight and body mass index associated with short-term (‘acute’) antipsychotic treatment in individuals with schizophrenia? 2. Does baseline physiology (e.g. body weight) and demographics (e.g. age) of patients predict magnitude of antipsychotic-associated metabolic dysregulation? 3. Are alterations in metabolic parameters over time associated with alterations in degree of psychopathology? 1 Searches We plan to search EMBASE, PsycINFO, and MEDLINE from inception using the following terms: 1 (Acepromazine or Acetophenazine or Amisulpride or Aripiprazole or Asenapine or Benperidol or Blonanserin or Bromperidol or Butaperazine or Carpipramine or Chlorproethazine or Chlorpromazine or Chlorprothixene or Clocapramine or Clopenthixol or Clopentixol or Clothiapine or Clotiapine or Clozapine or Cyamemazine or Cyamepromazine or Dixyrazine or Droperidol or Fluanisone or Flupehenazine or Flupenthixol or Flupentixol or Fluphenazine or Fluspirilen or Fluspirilene or Haloperidol or Iloperidone -
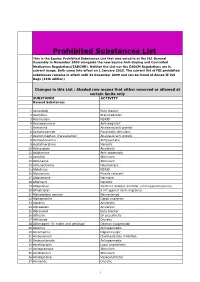
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Case Definitions
Case definitions Read code and drug code lists were compiled using standard methods (Dave and Petersen, 2009). Full code lists for all case definitions are available on request from the authors. SMI diagnoses Schizophrenia: schizophrenia, schizoaffective, paranoid schizophrenia Bipolar disorder: bipolar affective, psychotic depression, hypomanic psychoses, manic depressive, manic disorder, manic psychoses Individuals with other types of psychosis, or who only had a record indicating that they were on the SMI register, were not included in the study. Other SMI: non-organic psychoses, oneirophrenia, affective psychoses, depressive psychoses, paranoid states, reactive psychosis SMI register: severe mental illness register, national service framework mental health CVD events CVD events were identified from Read codes held in the medical records: CVD events were classified according to whether the Read code described a new (incident) or pre-existing (prevalent) condition as well as the type of condition (myocardial infarction (MI), unstable angina, angina, haemorrhagic stroke, ischaemic and unspecified stroke, transient ischaemic attack (TIA), surgery, unspecified coronary heart disease (CHD) or unspecified CVD). Records of death that were associated with a CVD diagnosis were identified from Read codes held in the cause of death field (1016500000) in the additional health records. In addition, Read codes for CVD that were recorded after the date of death were assumed to reflect fatal CVD events. Terms for identifying CVD included: MI: myocardial -

Thiopropazate Hydrochloride in Persistent Dyskinesia K
22 BRITISH MEDICAL JOURNAL 2 OCTOBER 1971 One patient developed severe haematemesis needing inpatient aware of the unreliability of subjective estimates of the difference therapy and had to be withdrawn from the trial. In retrospect in movement of the two sides of the face, but the statistically it was clear that he should not have been admitted to the trial significant differences reported here are considerable and it is Br Med J: first published as 10.1136/bmj.4.5778.22 on 2 October 1971. Downloaded from because he had a history of peptic ulceration. unlikely that observer error is responsible. The actual assess- ments of recovery in the severely denervated patients receiving corticotrophin mentioned above were 10%, 15%, 10%, 10%, Discussion 15%, and 15%, while all who took prednisolone were assessed at 50% recovery or above. Controlled trials of treatment in Bell's palsy are difficult to We had hoped to show that corticotrophin injections gave perform because of delay in starting therapy which is likely to better results than oral prednisolone if only because a previous prejudice the result. For this reason the patients were subdivided trial of cortisone for Bell's palsy gave a negative result (Tavemer, into early and late groups. Sixty-six started treatment on the 1954). In retrospect it is clear that the 1954 trial was intade- first or second day of paralysis and 120 on the third or fourth quately planned to produce a reliable result. The treatment was days. The results of earlier treatment were indeed better, started far too late to be effective, the dose of cortisone was too though both groups showed benefit. -

Special Project
National Mental Health Benchmarking Project Forensic Forum Special Project Seclusion Medication Audit A joint Australian, State and Territory Government Initiative October 2007 National Benchmarking Project - Forensic Forum Seclusion Medication Audit In previous benchmarking work conducted by the National Benchmarking Project – Forensic Forum on reviewing the Australian Council of Health Care Standards (ACHS) seclusion indicators, significant variation in organisational performance was noted. Participants agreed to further explore, in detail, seclusion events. A detailed audit of seclusion was conducted by participating services in late 2006. Discussion of possible reasons for variation identified that there may be differing prescribing patterns of psychotropic medication. The aim of this sub-project was to better understand the reasons for variation in seclusion practices and prescribing patterns across participating organizations Method: Consumer level data to be submitted for each consumer who was an inpatient on 1st November 2005 for acute in-scope services. Same day admissions are not included in this collection. Detailed specifications for this project were developed by the Queensland Mental Health Benchmarking Unit (QMHBU) with advice and endorsement from the National Benchmarking Project Forensic Forum. Formulae for calculation of Chlorpromazine and Benzodiazepine (Valium) equivalent doses are included in the specifications. This report was compiled by the QMHBU on behalf of the National Benchmarking Project – Forensic Forum; it includes the findings of this sub-project. Service Profile A B C D Group Total number of consumers in census 44 43 40 28 155 Average number of days for consumers (Nov) 25 12 27 29 22 Data was collected for 155 consumers. Average length of stay during the month of data collection was the lowest for Org B (12 days), but was similar for the other participating services (25-29 days). -
Sensory Phenomena in Movement Disorders
Sensory Phenomena in Movement Disorders Muhammad M. Nashatizadeh, M.D. Neurology/Neurosurgery Grand Rounds KU School of Medicine Friday, January 27, 2017 Disclosures • I have not received any financial, professional or personal benefit from any third-party entity regarding any of the topics I will be discussing today. • Some of the treatments discussed today are considered off-label usage by the Food and Drug Administration (FDA). Objectives • Increase awareness of sensory disturbances found in various movement disorders to offer appropriate treatment. • Demonstrate familiarity with treatment options of sensory phenomena relevant to movement disorders. Outline • Review of somatosensory input • Feedback from sensory input to motor output • Examples of sensory disturbance in movement disorders • Assessment and rating scales • Treatment of akathisia, tics and restless legs syndrome Somatosensory Input Courtesy: Clinicalgate.com • first order neuron • trigeminal nerve ganglion, dorsal root ganglion of spinal nerve • connects peripheral face and body with second order neuron Somatosensory Input Courtesy: Clinicalgate.com • second order neuron • brainstem nuclei, spinal nuclei • connects first order neuron with ventral posterior nucleus (VPN) of the thalamus Somatosensory Input Courtesy: Clinicalgate.com • third order neuron • connects VPN to the post-central gyrus (parietal lobe) Sensorimotor Integration Patel N et al. (2014) Lancet Neurol 13:100-112. Sensorimotor Integration • patients with Parkinson’s disease depend on external sensory cues to initiate and execute movement especially visual and kinesthetic input • impairment in proprioception likely plays a role in postural instability and limited body awareness in Parkinson’s disease • when moving both arms simultaneously, there is a tendency for a patient with Parkinson’s disease to overestimate affected limb movement Georgiou N et al. -

Electronic Search Strategies
Appendix 1: electronic search strategies The following search strategy will be applied in PubMed: ("Antipsychotic Agents"[Mesh] OR acepromazine OR acetophenazine OR amisulpride OR aripiprazole OR asenapine OR benperidol OR bromperidol OR butaperazine OR Chlorpromazine OR chlorproethazine OR chlorprothixene OR clopenthixol OR clotiapine OR clozapine OR cyamemazine OR dixyrazine OR droperidol OR fluanisone OR flupentixol OR fluphenazine OR fluspirilene OR haloperidol OR iloperidone OR levomepromazine OR levosulpiride OR loxapine OR lurasidone OR melperone OR mesoridazine OR molindone OR moperone OR mosapramine OR olanzapine OR oxypertine OR paliperidone OR penfluridol OR perazine OR periciazine OR perphenazine OR pimozide OR pipamperone OR pipotiazine OR prochlorperazine OR promazine OR prothipendyl OR quetiapine OR remoxipride OR risperidone OR sertindole OR sulpiride OR sultopride OR tiapride OR thiopropazate OR thioproperazine OR thioridazine OR tiotixene OR trifluoperazine OR trifluperidol OR triflupromazine OR veralipride OR ziprasidone OR zotepine OR zuclopenthixol ) AND ("Randomized Controlled Trial"[ptyp] OR "Controlled Clinical Trial"[ptyp] OR "Multicenter Study"[ptyp] OR "randomized"[tiab] OR "randomised"[tiab] OR "placebo"[tiab] OR "randomly"[tiab] OR "trial"[tiab] OR controlled[ti] OR randomized controlled trials[mh] OR random allocation[mh] OR double-blind method[mh] OR single-blind method[mh] OR "Clinical Trial"[Ptyp] OR "Clinical Trials as Topic"[Mesh]) AND (((Schizo*[tiab] OR Psychosis[tiab] OR psychoses[tiab] OR psychotic[tiab] OR disturbed[tiab] OR paranoid[tiab] OR paranoia[tiab]) AND ((Child*[ti] OR Paediatric[ti] OR Pediatric[ti] OR Juvenile[ti] OR Youth[ti] OR Young[ti] OR Adolesc*[ti] OR Teenage*[ti] OR early*[ti] OR kids[ti] OR infant*[ti] OR toddler*[ti] OR boys[ti] OR girls[ti] OR "Child"[Mesh]) OR "Infant"[Mesh])) OR ("Schizophrenia, Childhood"[Mesh])). -

Tardive Dyskinesia
Task Force Reports This is the eighteenth in a series of reports approved by the Board of Trustees of the American Psychiatric Association to give wider dissemination to the findings of APA's many commissions, committees, and task forces that are called upon to evaluate the state of the art in a problem area of current concern to the profession, to related disciplines, and to the public. The findings, opinions, and conclusions of the report do not necessarily represent the views of the officers, trustees, or all members of the Association. Each report, however, does represent the thoughtful judgment and findings of the task force of experts who composed it. These reports are considered a substantive contribution to the ongoing analysis and evaluation of problems, programs, issues, and practices in a given area of concern. Alan A. Stone, M.D. President, APA, 1979-80 Library of Congress Catalogue No. 80-65372 Copyright 1980 by the American Psychiatric Association 1400 K Street, N.W., Washington, D.C. 20005 Printed in U.S.A. 2nd Printing October, 1983 TARDIVE DYSKINESIA Report of the American Psychiatric Association Task Force on Late Neurological Effects of Antipsychotic Drugs Ross J. Baldessarini, M.D., Chairperson Jonathan O. Cole, M.D. John M. Davis, M.D. George Gardos, M.D., Consultant Sheldon H. Preskorn, M.D., Falk Fellow George M. Simpson, M.D. Daniel Tarsy, M.D., Invited Neurologist Approved for Publication by the Council on Research and Development John M. Davis, M.D., Chairperson Charles Gaitz, M.D. Edward Joel Sachar, M.D. George Winokur, M.D. -

2021 Equine Prohibited Substances List
2021 Equine Prohibited Substances List . Prohibited Substances include any other substance with a similar chemical structure or similar biological effect(s). Prohibited Substances that are identified as Specified Substances in the List below should not in any way be considered less important or less dangerous than other Prohibited Substances. Rather, they are simply substances which are more likely to have been ingested by Horses for a purpose other than the enhancement of sport performance, for example, through a contaminated food substance. LISTED AS SUBSTANCE ACTIVITY BANNED 1-androsterone Anabolic BANNED 3β-Hydroxy-5α-androstan-17-one Anabolic BANNED 4-chlorometatandienone Anabolic BANNED 5α-Androst-2-ene-17one Anabolic BANNED 5α-Androstane-3α, 17α-diol Anabolic BANNED 5α-Androstane-3α, 17β-diol Anabolic BANNED 5α-Androstane-3β, 17α-diol Anabolic BANNED 5α-Androstane-3β, 17β-diol Anabolic BANNED 5β-Androstane-3α, 17β-diol Anabolic BANNED 7α-Hydroxy-DHEA Anabolic BANNED 7β-Hydroxy-DHEA Anabolic BANNED 7-Keto-DHEA Anabolic CONTROLLED 17-Alpha-Hydroxy Progesterone Hormone FEMALES BANNED 17-Alpha-Hydroxy Progesterone Anabolic MALES BANNED 19-Norandrosterone Anabolic BANNED 19-Noretiocholanolone Anabolic BANNED 20-Hydroxyecdysone Anabolic BANNED Δ1-Testosterone Anabolic BANNED Acebutolol Beta blocker BANNED Acefylline Bronchodilator BANNED Acemetacin Non-steroidal anti-inflammatory drug BANNED Acenocoumarol Anticoagulant CONTROLLED Acepromazine Sedative BANNED Acetanilid Analgesic/antipyretic CONTROLLED Acetazolamide Carbonic Anhydrase Inhibitor BANNED Acetohexamide Pancreatic stimulant CONTROLLED Acetominophen (Paracetamol) Analgesic BANNED Acetophenazine Antipsychotic BANNED Acetophenetidin (Phenacetin) Analgesic BANNED Acetylmorphine Narcotic BANNED Adinazolam Anxiolytic BANNED Adiphenine Antispasmodic BANNED Adrafinil Stimulant 1 December 2020, Lausanne, Switzerland 2021 Equine Prohibited Substances List . Prohibited Substances include any other substance with a similar chemical structure or similar biological effect(s). -

Fluphenazine Decanoate (Depot) and Enanthate for Schizophrenia (Review)
Fluphenazine decanoate (depot) and enanthate for schizophrenia (Review) Maayan N, Quraishi SN, David A, Jayaswal A, Eisenbruch M, Rathbone J, Asher R, Adams CE This is a reprint of a Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2015, Issue 2 http://www.thecochranelibrary.com Fluphenazine decanoate (depot) and enanthate for schizophrenia (Review) Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 SUMMARY OF FINDINGS FOR THE MAIN COMPARISON . ..... 4 BACKGROUND .................................... 6 OBJECTIVES ..................................... 6 METHODS ...................................... 6 RESULTS....................................... 11 Figure1. ..................................... 13 Figure2. ..................................... 16 Figure3. ..................................... 17 ADDITIONALSUMMARYOFFINDINGS . 24 DISCUSSION ..................................... 30 AUTHORS’CONCLUSIONS . 32 ACKNOWLEDGEMENTS . 33 REFERENCES ..................................... 33 CHARACTERISTICSOFSTUDIES . 50 DATAANDANALYSES. 160 Analysis 1.1. Comparison 1 FLUPHENAZINE DECANOATE vs PLACEBO, Outcome 1 Death. 170 Analysis 1.2. Comparison 1 FLUPHENAZINE DECANOATE vs PLACEBO, Outcome 2 Global state: 1. Relapse. 171 Analysis 1.3. Comparison 1 FLUPHENAZINE DECANOATE vs PLACEBO, Outcome 3 Global state: 2. GAS (short term -

Drug/Substance Trade Name(S)
A B C D E F G H I J K 1 Drug/Substance Trade Name(s) Drug Class Existing Penalty Class Special Notation T1:Doping/Endangerment Level T2: Mismanagement Level Comments Methylenedioxypyrovalerone is a stimulant of the cathinone class which acts as a 3,4-methylenedioxypyprovaleroneMDPV, “bath salts” norepinephrine-dopamine reuptake inhibitor. It was first developed in the 1960s by a team at 1 A Yes A A 2 Boehringer Ingelheim. No 3 Alfentanil Alfenta Narcotic used to control pain and keep patients asleep during surgery. 1 A Yes A No A Aminoxafen, Aminorex is a weight loss stimulant drug. It was withdrawn from the market after it was found Aminorex Aminoxaphen, Apiquel, to cause pulmonary hypertension. 1 A Yes A A 4 McN-742, Menocil No Amphetamine is a potent central nervous system stimulant that is used in the treatment of Amphetamine Speed, Upper 1 A Yes A A 5 attention deficit hyperactivity disorder, narcolepsy, and obesity. No Anileridine is a synthetic analgesic drug and is a member of the piperidine class of analgesic Anileridine Leritine 1 A Yes A A 6 agents developed by Merck & Co. in the 1950s. No Dopamine promoter used to treat loss of muscle movement control caused by Parkinson's Apomorphine Apokyn, Ixense 1 A Yes A A 7 disease. No Recreational drug with euphoriant and stimulant properties. The effects produced by BZP are comparable to those produced by amphetamine. It is often claimed that BZP was originally Benzylpiperazine BZP 1 A Yes A A synthesized as a potential antihelminthic (anti-parasitic) agent for use in farm animals. -
Ep 2301628 A1
(19) & (11) EP 2 301 628 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 30.03.2011 Bulletin 2011/13 A61P 37/06 (2006.01) (21) Application number: 10013062.4 (22) Date of filing: 13.10.2004 (84) Designated Contracting States: • Manivasakam, Palaniyandi AT BE BG CH CY CZ DE DK EE ES FI FR GB GR West Roxbury HU IE IT LI LU MC NL PL PT RO SE SI SK TR MA 02132 (US) Designated Extension States: • Hurst, Nicole AL HR LT LV MK Boston MA 02132 (US) (30) Priority: 15.10.2003 US 512415 P • Foley, Michael A. Chestnut Hill (62) Document number(s) of the earlier application(s) in MA (US) accordance with Art. 76 EPC: • Slavonic, Michael S. 09002049.6 / 2 070 550 Quincy 04809944.4 / 1 680 121 MA 02169 (US) • Smith, Brendan (71) Applicant: Zalicus Inc. Sommerville Cambridge, MA 02142 (US) MA 02118 (US) • Auspitz, Benjamin A. (72) Inventors: Cambridge • Keith, Curtis MA 02139 (US) Boston MA 02118 (US) (74) Representative: Bösl, Raphael Konrad • Borisy, Alexis Isenbruck Bösl Hörschler LLP Arlington Patentanwälte MA 02476 (US) Prinzregentenstrasse 68 • Zimmermann, Grant R. 81675 München (DE) Winchester MA 01890 (US) Remarks: •Jost-Price, Edward Roydon This application was filed on 01-20-2010 as a West Roxbury divisional application to the application mentioned MA 02132 (US) under INID code 62. (54) Methods and reagents for the treatment of immunoinflammatory disorders (57) The invention features, among others, a tetra- stituted pyrimidopyrimidine and a corticosteroid for use substituted pyrimidopyrimidine and a corticosteroid for ina method for treating an immunoinflammatory disorder.