Katrin Gutsche
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Tumor Suppressor Notch Inhibits Head and Neck Squamous Cell
The Texas Medical Center Library DigitalCommons@TMC The University of Texas MD Anderson Cancer Center UTHealth Graduate School of The University of Texas MD Anderson Cancer Biomedical Sciences Dissertations and Theses Center UTHealth Graduate School of (Open Access) Biomedical Sciences 12-2015 THE TUMOR SUPPRESSOR NOTCH INHIBITS HEAD AND NECK SQUAMOUS CELL CARCINOMA (HNSCC) TUMOR GROWTH AND PROGRESSION BY MODULATING PROTO-ONCOGENES AXL AND CTNNAL1 (α-CATULIN) Shhyam Moorthy Shhyam Moorthy Follow this and additional works at: https://digitalcommons.library.tmc.edu/utgsbs_dissertations Part of the Biochemistry, Biophysics, and Structural Biology Commons, Cancer Biology Commons, Cell Biology Commons, and the Medicine and Health Sciences Commons Recommended Citation Moorthy, Shhyam and Moorthy, Shhyam, "THE TUMOR SUPPRESSOR NOTCH INHIBITS HEAD AND NECK SQUAMOUS CELL CARCINOMA (HNSCC) TUMOR GROWTH AND PROGRESSION BY MODULATING PROTO-ONCOGENES AXL AND CTNNAL1 (α-CATULIN)" (2015). The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access). 638. https://digitalcommons.library.tmc.edu/utgsbs_dissertations/638 This Dissertation (PhD) is brought to you for free and open access by the The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences at DigitalCommons@TMC. It has been accepted for inclusion in The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences Dissertations and Theses (Open Access) by an authorized administrator of DigitalCommons@TMC. For more information, please contact [email protected]. THE TUMOR SUPPRESSOR NOTCH INHIBITS HEAD AND NECK SQUAMOUS CELL CARCINOMA (HNSCC) TUMOR GROWTH AND PROGRESSION BY MODULATING PROTO-ONCOGENES AXL AND CTNNAL1 (α-CATULIN) by Shhyam Moorthy, B.S. -

Lack of Rybp in Mouse Embryonic Stem Cells Impairs Cardiac Differentiation O
Page 1 of 43 1 Lack of Rybp in Mouse Embryonic Stem Cells Impairs Cardiac Differentiation O. Ujhelly1, V. Szabo2, G. Kovacs2, F. Vajda2, S. Mallok4, J. Prorok5, K. Acsai6, Z. Hegedus3, S. Krebs4, A. Dinnyes1,7 and M. K. Pirity2 * 1 BioTalentum Ltd, H-2100 Gödöllö, Hungary 2 Institute of Genetics, Biological Research Centre, Hungarian Academy of Sciences, H-6726 Szeged, Hungary 3 Institute of Biophysics, Biological Research Centre, Hungarian Academy of Sciences, H-6726 Szeged, Hungary 4 Laboratory for Functional Genome Analysis (LAFUGA), Gene Center, LMU Munich, Munich, Germany 5 Department of Pharmacology and Pharmacotherapy, University of Szeged, Szeged, Hungary 6 MTA-SZTE Research Group of Cardiovascular Pharmacology, Szeged, Hungary 7 Molecular Animal Biotechnology Laboratory, Szent Istvan University, Gödöllö, Hungary * Author for correspondence at Institute of Genetics, Biological Research Centre, Hungarian Academy of Sciences, H-6726 Szeged, Hungary Stem Cells and Development Ring1 and Yy1 Binding Protein (Rybp) has been implicated in transcriptional regulation, apoptotic signaling and as a member of the polycomb repressive complex 1 has important function in regulating pluripotency and differentiation of embryonic stem cells. Earlier, we have proven that Rybp plays essential role in mouse embryonic and central nervous system development. This work identifies Rybp, as a critical regulator of heart development. Rybp is readily detectable in the developing mouse heart from day 8.5 of embryonic development. Prominent Rybp expression persists during all embryonic stages and Rybp marks differentiated cell types of the heart. By utilizing rybp null embryonic stem cells (ESCs) in an in vitro cardiac Lack of Rybp in Mouse Embryonic Stem Cells Impairs Cardiac Differentiation (doi: 10.1089/scd.2014.0569) differentiation assay we found that rybp null ESCs do not form rhythmically beating cardiomyocytes. -

Brain-Region-Specific Contributions of Foxp1 to Autism And
BRAIN-REGION-SPECIFIC CONTRIBUTIONS OF FOXP1 TO AUTISM AND INTELLECTUAL DISABILITY PHENOTYPES Daniel John Araujo APPROVED BY SUPERVISORY COMMITTEE: Amelia J. Eisch, Ph.D. (Chair) _____________________________ Genevieve Konopka, Ph.D. (Mentor) _____________________________ Craig M. Powell, M.D., Ph.D. _____________________________ Lenora J. Volk, Ph.D. _____________________________ Jiang Wu, Ph.D. _____________________________ DEDICATION I would like to thank my thesis advisor Dr. Genevieve Konopka who has always pushed me to strive for excellence in my work. It’s been an honor to study neuroscience under her supervision and she will serve as an example for the rest of my scientific career. I would like to thank my wife Sarah Teresita Vega for her unwavering love and patience. Sarah has been my best friend for the past nine years and her encouragement has allowed me to face any challenge with grit. I also thank my thesis committee members for all of their suggestions on how to improve my research. I would like to thank Dr. Timothy Raabe and Dr. Nancy Street for their continuous support of both my undergraduate and graduate career. Finally, I dedicate this dissertation to my grandparents George Cuellar Araujo and Margarita Salinas Araujo who raised my two siblings and me. Any success I’ve had in life belongs to them. ii BRAIN-REGION-SPECIFIC CONTRIBUTIONS OF FOXP1 TO AUTISM AND INTELLECTUAL DISABILITY PHENOTYPES By DANIEL JOHN ARAUJO, B.S. DISSERTATION Presented to the Faculty of the Graduate School of Biomedical Sciences at The University of Texas Southwestern Medical Center In Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY The University of Texas Southwestern Medical Center Dallas, Texas August 11, 2017 iii Copyright By Daniel John Araujo, 2017 All Rights Reserved iv BRAIN-REGION-SPECIFIC CONTRIBUTIONS OF FOXP1 TO AUTISM AND INTELLECTUAL DISABILITY PHENOTPES Publication No. -

Lupus Nephritis Supp Table 5
Supplementary Table 5 : Transcripts and DAVID pathways correlating with the expression of CD4 in lupus kidney biopsies Positive correlation Negative correlation Transcripts Pathways Transcripts Pathways Identifier Gene Symbol Correlation coefficient with CD4 Annotation Cluster 1 Enrichment Score: 26.47 Count P_Value Benjamini Identifier Gene Symbol Correlation coefficient with CD4 Annotation Cluster 1 Enrichment Score: 3.16 Count P_Value Benjamini ILMN_1727284 CD4 1 GOTERM_BP_FAT translational elongation 74 2.50E-42 1.00E-38 ILMN_1681389 C2H2 zinc finger protein-0.40001984 INTERPRO Ubiquitin-conjugating enzyme/RWD-like 17 2.00E-05 4.20E-02 ILMN_1772218 HLA-DPA1 0.934229063 SP_PIR_KEYWORDS ribosome 60 2.00E-41 4.60E-39 ILMN_1768954 RIBC1 -0.400186083 SMART UBCc 14 1.00E-04 3.50E-02 ILMN_1778977 TYROBP 0.933302249 KEGG_PATHWAY Ribosome 65 3.80E-35 6.60E-33 ILMN_1699190 SORCS1 -0.400223681 SP_PIR_KEYWORDS ubl conjugation pathway 81 1.30E-04 2.30E-02 ILMN_1689655 HLA-DRA 0.915891173 SP_PIR_KEYWORDS protein biosynthesis 91 4.10E-34 7.20E-32 ILMN_3249088 LOC93432 -0.400285215 GOTERM_MF_FAT small conjugating protein ligase activity 35 1.40E-04 4.40E-02 ILMN_3228688 HLA-DRB1 0.906190291 SP_PIR_KEYWORDS ribonucleoprotein 114 4.80E-34 6.70E-32 ILMN_1680436 CSH2 -0.400299744 SP_PIR_KEYWORDS ligase 54 1.50E-04 2.00E-02 ILMN_2157441 HLA-DRA 0.902996561 GOTERM_CC_FAT cytosolic ribosome 59 3.20E-33 2.30E-30 ILMN_1722755 KRTAP6-2 -0.400334007 GOTERM_MF_FAT acid-amino acid ligase activity 40 1.60E-04 4.00E-02 ILMN_2066066 HLA-DRB6 0.901531942 SP_PIR_KEYWORDS -

Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

Us 2018 / 0305689 A1
US 20180305689A1 ( 19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2018 /0305689 A1 Sætrom et al. ( 43 ) Pub . Date: Oct. 25 , 2018 ( 54 ) SARNA COMPOSITIONS AND METHODS OF plication No . 62 /150 , 895 , filed on Apr. 22 , 2015 , USE provisional application No . 62/ 150 ,904 , filed on Apr. 22 , 2015 , provisional application No. 62 / 150 , 908 , (71 ) Applicant: MINA THERAPEUTICS LIMITED , filed on Apr. 22 , 2015 , provisional application No. LONDON (GB ) 62 / 150 , 900 , filed on Apr. 22 , 2015 . (72 ) Inventors : Pål Sætrom , Trondheim (NO ) ; Endre Publication Classification Bakken Stovner , Trondheim (NO ) (51 ) Int . CI. C12N 15 / 113 (2006 .01 ) (21 ) Appl. No. : 15 /568 , 046 (52 ) U . S . CI. (22 ) PCT Filed : Apr. 21 , 2016 CPC .. .. .. C12N 15 / 113 ( 2013 .01 ) ; C12N 2310 / 34 ( 2013. 01 ) ; C12N 2310 /14 (2013 . 01 ) ; C12N ( 86 ) PCT No .: PCT/ GB2016 /051116 2310 / 11 (2013 .01 ) $ 371 ( c ) ( 1 ) , ( 2 ) Date : Oct . 20 , 2017 (57 ) ABSTRACT The invention relates to oligonucleotides , e . g . , saRNAS Related U . S . Application Data useful in upregulating the expression of a target gene and (60 ) Provisional application No . 62 / 150 ,892 , filed on Apr. therapeutic compositions comprising such oligonucleotides . 22 , 2015 , provisional application No . 62 / 150 ,893 , Methods of using the oligonucleotides and the therapeutic filed on Apr. 22 , 2015 , provisional application No . compositions are also provided . 62 / 150 ,897 , filed on Apr. 22 , 2015 , provisional ap Specification includes a Sequence Listing . SARNA sense strand (Fessenger 3 ' SARNA antisense strand (Guide ) Mathew, Si Target antisense RNA transcript, e . g . NAT Target Coding strand Gene Transcription start site ( T55 ) TY{ { ? ? Targeted Target transcript , e . -

Universidade Estadual De Campinas Instituto De Biologia
UNIVERSIDADE ESTADUAL DE CAMPINAS INSTITUTO DE BIOLOGIA CAROLINE BRANDÃO TELES EMPREGANDO A PROTEÔMICA PARA COMPREENDER OS MECANISMOS DE AÇÃO DOS ANTIPSICÓTICOS EM OLIGODENDRÓCITOS HUMANOS EMPLOYING PROTEOMICS TO UNDERSTAND THE MECHANISMS OF ACTION OF ANTIPSYCHOTICS IN HUMAN OLIGODENDROCYTES CAMPINAS 2018 CAROLINE BRANDÃO TELES EMPREGANDO A PROTEÔMICA PARA COMPREENDER OS MECANISMOS DE AÇÃO DOS ANTIPSICÓTICOS EM OLIGODENDRÓCITOS HUMANOS EMPLOYING PROTEOMICS TO UNDERSTAND THE MECHANISMS OF ACTION OF ANTIPSYCHOTICS IN HUMAN OLIGODENDROCYTES Dissertação apresentada ao Instituto de Biologia da Universidade Estadual de Campinas como parte dos requisitos exigidos para a obtenção do título de Mestra em Biologia Funcional e Molecular, na área de Bioquímica Dissertation presented to the Biology Institute of the University of Campinas as part of the requisites required to obtain of Master's degree in Functional and Molecular Biology in the area of Biochemistry ESTE ARQUIVO DIGITAL CORRESPONDE À VERSÃO FINAL DA DISSERTAÇÃO DEFENDIDA PELA ALUNA CAROLINE BRANDÃO TELES, E ORIENTADA PELO PROF. DR. DANIEL MARTINS DE SOUZA E CO- ORIENTADA PELA PROF. DRª JULIANA SILVA CASSOLI Orientador: PROF. DR. DANIEL MARTINS DE SOUZA Coorientador: DRª. JULIANA SILVA CASSOLI CAMPINAS 2018 Agência(s) de fomento e nº(s) de processo(s): FAPESP, 2015/23049-0 Ficha catalográfica Universidade Estadual de Campinas Biblioteca do Instituto de Biologia Mara Janaina de Oliveira - CRB 8/6972 Brandão-Teles, Caroline, 1990- B733e Empregando a proteômica para compreender os mecanismos de ação dos antipsicóticos em oligodendrócitos humanos / Caroline Brandão Teles. – Campinas, SP : [s.n.], 2018. Orientador: Daniel Martins de Souza. Coorientador: Juliana Silva Cassoli. Dissertação (mestrado) – Universidade Estadual de Campinas, Instituto de Biologia. 1. Esquizofrenia. -

Attachment PDF Icon
Gene Name Name of Protein (UniProtID_SPECIES, protein name, origin species, gene name) Peptide Count in IP Peptide Count in IgG Fold Enrichment ACTB P60709|ACTB_HUMAN Actin, cytoplasmic 1 OS=Homo sapiens GN=ACTB PE=1 SV=1 7 0 Not in IgG control TCOF1 Q13428|TCOF_HUMAN Treacle protein OS=Homo sapiens GN=TCOF1 PE=1 SV=3 7 0 Not in IgG control MKI67 P46013|KI67_HUMAN Proliferation marker protein Ki-67 OS=Homo sapiens GN=MKI67 PE=1 SV=2 6 0 Not in IgG control DSP P15924|DESP_HUMAN Desmoplakin OS=Homo sapiens GN=DSP PE=1 SV=3 5 0 Not in IgG control COL1A1 P02452|CO1A1_HUMAN Collagen alpha-1(I) chain OS=Homo sapiens GN=COL1A1 PE=1 SV=5 5 0 Not in IgG control PRKDC P78527|PRKDC_HUMAN DNA-dependent protein kinase catalytic subunit OS=Homo sapiens GN=PRKDC PE=1 SV=3 5 0 Not in IgG control C4A P0C0L4|CO4A_HUMAN Complement C4-A OS=Homo sapiens GN=C4A PE=1 SV=2 3 0 Not in IgG control HSPA8 P11142|HSP7C_HUMAN Heat shock cognate 71 kDa protein OS=Homo sapiens GN=HSPA8 PE=1 SV=1 3 0 Not in IgG control MCM6 Q14566|MCM6_HUMAN DNA replication licensing factor MCM6 OS=Homo sapiens GN=MCM6 PE=1 SV=1 2 0 Not in IgG control No_GeneID A0A0U1RRH7|A0A0U1RRH7_HUMAN Histone H2A OS=Homo sapiens PE=3 SV=1 2 0 Not in IgG control MDC1 Q14676|MDC1_HUMAN Mediator of DNA damage checkpoint protein 1 OS=Homo sapiens GN=MDC1 PE=1 SV=3 2 0 Not in IgG control DSG1 Q02413|DSG1_HUMAN Desmoglein-1 OS=Homo sapiens GN=DSG1 PE=1 SV=2 2 0 Not in IgG control HIST1H4A P62805|H4_HUMAN Histone H4 OS=Homo sapiens GN=HIST1H4A PE=1 SV=2 2 0 Not in IgG control HSP90AB1 P08238|HS90B_HUMAN -

Table S12: Genes Identified on GISTIC on the SNP-FASST2 Segmentation Algorithm
Table S12: Genes identified on GISTIC on the SNP-FASST2 Segmentation Algorithm Gene Symbol Chromosome Start End Length STPG1 chr1 24683488 24741587 58100 NIPAL3 chr1 24742244 24799473 57230 RCAN3AS chr1 24822822 24828850 6029 RCAN3 chr1 24828840 24863510 34671 NCMAP chr1 24882566 24935818 53253 SRRM1 chr1 24969593 24999772 30180 CLIC4 chr1 25071759 25170815 99057 RUNX3 chr1 25226001 25291501 65501 SYF2 chr1 25548766 25559013 10248 C1orf63 chr1 25568739 25573985 5247 RHD chr1 25598980 25656936 57957 TMEM50A chr1 25664788 25688852 24065 RHCE chr1 25688739 25747363 58625 TMEM57 chr1 25757387 25826698 69312 LDLRAP1 chr1 25870075 25895377 25303 MAN1C1 chr1 25943958 26111258 167301 SEPN1 chr1 26126666 26144713 18048 LOC646471 chr1 26146444 26150097 3654 FAM54B chr1 26146396 26159433 13038 AUNIP chr1 26160496 26185848 25353 PAQR7 chr1 26187974 26197744 9771 STMN1 chr1 26210676 26233368 22693 MIR3917 chr1 26232852 26232945 94 PAFAH2 chr1 26286257 26324648 38392 EXTL1 chr1 26348270 26362954 14685 SLC30A2 chr1 26364513 26372604 8092 TRIM63 chr1 26377795 26394125 16331 PDIK1L chr1 26437655 26452039 14385 FAM110D chr1 26485510 26489119 3610 ZNF593 chr1 26496387 26497364 978 CNKSR1 chr1 26503980 26516375 12396 CATSPER4 chr1 26517118 26529033 11916 CEP85 chr1 26560692 26605299 44608 SH3BGRL3 chr1 26606212 26608013 1802 UBXN11 chr1 26608772 26644756 35985 CD52 chr1 26644410 26647014 2605 AIM1L chr1 26648349 26680621 32273 ZNF683 chr1 26688124 26699266 11143 LIN28A chr1 26737268 26756219 18952 DHDDS chr1 26758772 26797795 39024 HMGN2 chr1 26798901 26803133 -

Identifying Biomarkers for Non-Invasive Diagnosis of Endometriosis
Identifying biomarkers for non-invasive diagnosis of endometriosis Stella Irungu Department of Women’s Cancer Institute for Women’s Health University College London PhD in Biomarker Discovery and Proteomics This thesis is submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy from University College London I, Stella Irungu confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated. 2 Abstract Endometriosis is a gynaecological disorder occurring when endometrial cells are shed through the fallopian tubes and implant on surfaces in the abdomen and pelvis. There they form lesions that respond to hormones of the cycle and stimulate inflammation. Women with endometriosis experience painful debilitating periods, pain on intercourse and defecation, and may have difficulties conceiving. It is a common disorder, affecting 5-10% of women of reproductive age. Diagnosis of endometriosis is difficult and is often delayed by 5-11 years. Symptoms do not correlate with disease severity and imaging techniques are only sensitive for diagnosing ovarian endometriomas. Definitive diagnosis is surgical, requiring laparoscopy under general anaesthetic, exposing patients to potentially serious complications. With these facts in mind, the aim of this project was to identify biomarkers for the non-invasive diagnosis of endometriosis. This was achieved by defining the protein expression profiles of tissue samples collected from women diagnosed with endometriosis and from control patients who underwent surgery for investigation of chronic pelvic pain or who underwent prophylactic surgery because of familial cancer history. Discovery work involved the use of complementary, quantitative proteomic profiling by 2D difference gel electrophoresis and multiplex mass tagging linked to liquid chromatography-based separation and tandem mass spectrometry. -

SKU# Product Description TP300009 Recombinant Protein of Human
SKU# Product description TP300009 Recombinant protein of human protein phosphatase methylesterase 1 (PPME1) TP300010 Recombinant protein of human small nuclear ribonucleoprotein 25kDa (U11/U12) (SNRNP25) TP300016 Recombinant protein of human chromosome 14 open reading frame 166 (C14orf166) TP300018 Recombinant protein of human leucine carboxyl methyltransferase 1 (LCMT1), transcript variant 1 TP300019 Recombinant protein of human HMP19 protein (HMP19) TP300033 Recombinant protein of human mitochondrial ribosomal protein L11 (MRPL11), nuclear gene encoding mitochondrial protein, transcript variant 1 TP300035 Recombinant protein of human exosome component 3 (EXOSC3), transcript variant 1 TP300036 Recombinant protein of human hypothetical protein HSPC152 (HSPC152) TP300049 Recombinant protein of human transmembrane protein 208 (TMEM208) TP300051 Recombinant protein of human dynein, light chain, roadblock-type 1 (DYNLRB1) TP300052 Recombinant protein of human mitochondrial ribosomal protein L18 (MRPL18), nuclear gene encoding mitochondrial protein TP300054 Recombinant protein of human ribosomal protein L36 (RPL36), transcript variant 2 TP300055 Recombinant protein of human methyltransferase like 11A (METTL11A) TP300071 Recombinant protein of human spastic paraplegia 21 (autosomal recessive, Mast syndrome) (SPG21), transcript variant 1 TP300076 Recombinant protein of human dysbindin (dystrobrevin binding protein 1) domain containing 2 (DBNDD2), transcript variant 1 TP300079 Recombinant protein of human SCAN domain containing 1 (SCAND1), transcript -
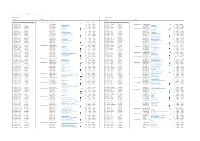
Lupus Nephritis Supp Table 7
Supplementary Table 7 : Transcripts and DAVID pathways correlating with expression of CD3 in lupus kidney biopsies Positive correlation Negative correlation Transcripts Pathways Transcripts Pathways Identifier Gene Symbol Correlation coefficient with CD3 Annotation Cluster 1 Enrichment Score: 11.22 Count P_Value Benjamini Identifier Gene Symbol Correlation coefficient with CD3 ILMN_2325837 CD3D 1 SP_PIR_KEYWORDS ribosome 42 5.40E-21 1.20E-18 ILMN_1726667 LOC728758 -0.40000032 Annotation Cluster 1 Enrichment Score: 8.3 Count P_Value Benjamini ILMN_2061043 CD48 0.905183649 GOTERM_BP_FAT translational elongation 49 2.00E-18 8.60E-15 ILMN_1767032 DDI1 -0.400066325 SP_PIR_KEYWORDS oxidoreductase 98 1.10E-11 3.90E-09 ILMN_2261416 CD3D 0.880984568 GOTERM_CC_FAT cytosolic ribosome 42 3.50E-17 2.30E-14 ILMN_3307863 TAOK3 -0.400088253 GOTERM_BP_FAT oxidation reduction 105 3.70E-10 1.40E-06 ILMN_1886655 TCRVB 0.875380574 SP_PIR_KEYWORDS protein biosynthesis 64 1.10E-16 1.00E-14 ILMN_1840934 AJ420430 -0.400098378 GOTERM_MF_FAT electron carrier activity 40 3.10E-05 5.90E-03 ILMN_1659800 BCL11A 0.861258356 KEGG_PATHWAY Ribosome 44 6.90E-15 1.10E-12 ILMN_3235584 TRIM66 -0.400113232 Annotation Cluster 2 Enrichment Score: 7.1 Count P_Value Benjamini ILMN_2098126 CCL5 0.853134526 GOTERM_CC_FAT cytosolic part 55 8.50E-14 1.80E-11 ILMN_2145760 YIPF4 -0.400116748 SP_PIR_KEYWORDS mitochondrion 143 3.20E-16 2.30E-13 ILMN_1716651 RUNX2 0.839003672 GOTERM_CC_FAT ribosomal subunit 48 8.70E-13 1.40E-10 ILMN_2146648 PRB3 -0.400169733 GOTERM_CC_FAT mitochondrion 176