ADRB2-Targeting Therapies for Prostate Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MONOCLONAL ANTI-VASOACTIVE INTESTINAL PEPTIDE RECEPTOR 1 (VIPR 1, VPAC1) Clone AS58 Purified Mouse Immunoglobulin
MONOCLONAL ANTI-VASOACTIVE INTESTINAL PEPTIDE RECEPTOR 1 (VIPR 1, VPAC1) Clone AS58 Purified Mouse Immunoglobulin Product Number V1631 Product Description Although structurally related, VIPR1 and VIPR2 exhibit Monoclonal Anti-Vasoactive Intestinal Peptide differences in expression and function and VIP has a Receptor 1 (VIPR1) (mouse IgG2a isotype) is derived 3-10 fold preference for VIPR1 over VIPR2 receptors. from the hybridoma produced by the fusion of mouse myeloma cells and splenocytes from a BALB/c mouse VIPR1 is expressed throughout the central nervous immunized with a unique peptide corresponding to a system (predominantly in the cerebral cortex and portion of human Vasoactive Intestinal Peptide hippocampus), in peripheral tissues including liver, lung Receptor 1 (VIPR1). The antibody was purified from and intestine and in T lymphocytes.14 VIPR1 mediates tissue culture supernatant using immobilized Protein G. suppression of chemotaxis and matrix metalloprotein- ase expression elicited by some cytokines and chemo- Monoclonal Anti-Vasoactive Intestinal Peptide kines, tumor cell migration induced by VIP, and vaso- Receptor 1 (VIPR1) recognizes VIPR1 protein from dilation. human and rat tissue by immunoblotting and by flow cytometric analysis of human cells using indirect VIPR2 is expressed throughout the central nervous immunofluorescence. The antibody does not recognize system, but to varying degrees. The highest expression VIPR2 protein. levels are in the thalamus and suprachiasmatic nucleus, but VIPR2 is also present in the hippocampus, -

Mouse Genotypes Drive the Liver and Adrenal Gland Clocks
www.nature.com/scientificreports OPEN Mouse genotypes drive the liver and adrenal gland clocks Rok Košir1,*, Uršula Prosenc Zmrzljak1,*, Anja Korenčič1, Peter Juvan1, Jure Ačimovič2 & Damjana Rozman1,2 Received: 15 November 2015 Circadian rhythms regulate a plethora of physiological processes. Perturbations of the rhythm can Accepted: 25 July 2016 result in pathologies which are frequently studied in inbred mouse strains. We show that the genotype Published: 18 August 2016 of mouse lines defines the circadian gene expression patterns. Expression of majority of core clock and output metabolic genes are phase delayed in the C56BL/6J line compared to 129S2 in the adrenal glands and the liver. Circadian amplitudes are generally higher in the 129S2 line. Experiments in dark – dark (DD) and light – dark conditions (LD), exome sequencing and data mining proposed that mouse lines differ in single nucleotide variants in the binding regions of clock related transcription factors in open chromatin regions. A possible mechanisms of differential circadian expression could be the entrainment and transmission of the light signal to peripheral organs. This is supported by the genotype effect in adrenal glands that is largest under LD, and by the high number of single nucleotide variants in the Receptor, Kinase and G-protein coupled receptor Panther molecular function categories. Different phenotypes of the two mouse lines and changed amino acid sequence of the Period 2 protein possibly contribute further to the observed differences in circadian gene expression. The majority of organisms on Earth have evolved a robust inner body circadian (circa = approximately, dian = day) clock that ticks away in most of their cells. -

G Protein-Coupled Receptors
S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2015/16: G protein-coupled receptors. British Journal of Pharmacology (2015) 172, 5744–5869 THE CONCISE GUIDE TO PHARMACOLOGY 2015/16: G protein-coupled receptors Stephen PH Alexander1, Anthony P Davenport2, Eamonn Kelly3, Neil Marrion3, John A Peters4, Helen E Benson5, Elena Faccenda5, Adam J Pawson5, Joanna L Sharman5, Christopher Southan5, Jamie A Davies5 and CGTP Collaborators 1School of Biomedical Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK, 2Clinical Pharmacology Unit, University of Cambridge, Cambridge, CB2 0QQ, UK, 3School of Physiology and Pharmacology, University of Bristol, Bristol, BS8 1TD, UK, 4Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK, 5Centre for Integrative Physiology, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2015/16 provides concise overviews of the key properties of over 1750 human drug targets with their pharmacology, plus links to an open access knowledgebase of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. The full contents can be found at http://onlinelibrary.wiley.com/doi/ 10.1111/bph.13348/full. G protein-coupled receptors are one of the eight major pharmacological targets into which the Guide is divided, with the others being: ligand-gated ion channels, voltage-gated ion channels, other ion channels, nuclear hormone receptors, catalytic receptors, enzymes and transporters. These are presented with nomenclature guidance and summary information on the best available pharmacological tools, alongside key references and suggestions for further reading. -

Multi-Functionality of Proteins Involved in GPCR and G Protein Signaling: Making Sense of Structure–Function Continuum with In
Cellular and Molecular Life Sciences (2019) 76:4461–4492 https://doi.org/10.1007/s00018-019-03276-1 Cellular andMolecular Life Sciences REVIEW Multi‑functionality of proteins involved in GPCR and G protein signaling: making sense of structure–function continuum with intrinsic disorder‑based proteoforms Alexander V. Fonin1 · April L. Darling2 · Irina M. Kuznetsova1 · Konstantin K. Turoverov1,3 · Vladimir N. Uversky2,4 Received: 5 August 2019 / Revised: 5 August 2019 / Accepted: 12 August 2019 / Published online: 19 August 2019 © Springer Nature Switzerland AG 2019 Abstract GPCR–G protein signaling system recognizes a multitude of extracellular ligands and triggers a variety of intracellular signal- ing cascades in response. In humans, this system includes more than 800 various GPCRs and a large set of heterotrimeric G proteins. Complexity of this system goes far beyond a multitude of pair-wise ligand–GPCR and GPCR–G protein interactions. In fact, one GPCR can recognize more than one extracellular signal and interact with more than one G protein. Furthermore, one ligand can activate more than one GPCR, and multiple GPCRs can couple to the same G protein. This defnes an intricate multifunctionality of this important signaling system. Here, we show that the multifunctionality of GPCR–G protein system represents an illustrative example of the protein structure–function continuum, where structures of the involved proteins represent a complex mosaic of diferently folded regions (foldons, non-foldons, unfoldons, semi-foldons, and inducible foldons). The functionality of resulting highly dynamic conformational ensembles is fne-tuned by various post-translational modifcations and alternative splicing, and such ensembles can undergo dramatic changes at interaction with their specifc partners. -

Immunobiology of VPAC2 Receptor
Aus der Medizinischen Poliklinik-Innenstadt der Ludwig-Maximilians-Universität München Direktor: Professor Dr. med. M. Reincke Immunobiology of the VPAC2 Receptor Dissertation zum Erwerb des Doktorgrades der Medizin an der Medizinischen Fakultät der Ludwig-Maximilians-Universität zu München Vorgelegt von Carola Grinninger aus München 2010 Mit Genehmigung der Medizinischen Fakultät der Universität München Berichterstatter: Prof. Dr. med. S. Schewe Mitberichterstatter: PD Dr. B. Bachmeier Prof. Dr. H. Kellner Prof. Dr. U. Gresser Betreuung durch den promovierten Mitarbeiter: PD Dr. P. J. Nelson Dekan: Prof. Dr. med. Dr. h.c. M. Reiser, FACR, FRCR Tag der mündlichen Prüfung: 07.10.2010 2 CONTENTS Contents……………………………………………………………………….…3 Summary…………………………………………………………………………5 1. Introduction……………………………………………………………………10 1.1 General introduction……………………………………………………...10 1.2 G-Protein-coupled Receptors…………………………………………….10 1.3 G-protein-coupled signalling…………………………………………….13 1.4 Molecularbiology and structure of VPAC Receptors………………...….15 1.5 Vasoactive Intestinal Peptide (VIP)……………………………………...22 1.5.1 Biochemical structure of vasoactive intestinal peptide………...............22 1.6 VIP and intracellular signaling…………………………………………...25 1.7 VIP and rheumatoid arthritis…………………………………..…………26 1.8 Hypothesis………………………………………………………………..29 2. Materials……………………………………………………..………………31 2.1 Bacteria ……………………………………………………………….…31 2.2 Vectors……………………………………………………………….…..31 2.3 Cells………………………………………………………………….…..32 2.4 Mice……………………………………………………………….….….33 2.5 Oligonucleotides………………………………………………….….…..33 -

1 Supplemental Material Maresin 1 Activates LGR6 Receptor
Supplemental Material Maresin 1 Activates LGR6 Receptor Promoting Phagocyte Immunoresolvent Functions Nan Chiang, Stephania Libreros, Paul C. Norris, Xavier de la Rosa, Charles N. Serhan Center for Experimental Therapeutics and Reperfusion Injury, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts 02115, USA. 1 Supplemental Table 1. Screening of orphan GPCRs with MaR1 Vehicle Vehicle MaR1 MaR1 mean RLU > GPCR ID SD % Activity Mean RLU Mean RLU + 2 SD Mean RLU Vehicle mean RLU+2 SD? ADMR 930920 33283 997486.5381 863760 -7% BAI1 172580 18362 209304.1828 176160 2% BAI2 26390 1354 29097.71737 26240 -1% BAI3 18040 758 19555.07976 18460 2% CCRL2 15090 402 15893.6583 13840 -8% CMKLR2 30080 1744 33568.954 28240 -6% DARC 119110 4817 128743.8016 126260 6% EBI2 101200 6004 113207.8197 105640 4% GHSR1B 3940 203 4345.298244 3700 -6% GPR101 41740 1593 44926.97349 41580 0% GPR103 21413 1484 24381.25067 23920 12% NO GPR107 366800 11007 388814.4922 360020 -2% GPR12 77980 1563 81105.4653 76260 -2% GPR123 1485190 46446 1578081.986 1342640 -10% GPR132 860940 17473 895885.901 826560 -4% GPR135 18720 1656 22032.6827 17540 -6% GPR137 40973 2285 45544.0809 39140 -4% GPR139 438280 16736 471751.0542 413120 -6% GPR141 30180 2080 34339.2307 29020 -4% GPR142 105250 12089 129427.069 101020 -4% GPR143 89390 5260 99910.40557 89380 0% GPR146 16860 551 17961.75617 16240 -4% GPR148 6160 484 7128.848113 7520 22% YES GPR149 50140 934 52008.76073 49720 -1% GPR15 10110 1086 12282.67884 -

VIP-Seasonal-Encoding-SCN.Pdf
European Journal of Neuroscience European Journal of Neuroscience, Vol. 35, pp. 1466–1474, 2012 doi:10.1111/j.1460-9568.2012.08054.x BEHAVIORAL NEUROSCIENCE Role of vasoactive intestinal peptide in seasonal encoding by the suprachiasmatic nucleus clock Eliane A. Lucassen,1 Hester C. van Diepen,1 Thijs Houben,1 Stephan Michel,1 Christopher S. Colwell1,2,* and Johanna H. Meijer1,* 1Laboratory of Neurophysiology, Department of Molecular Cell Biology, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, The Netherlands 2Laboratory of Circadian and Sleep Medicine, Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles, CA, USA Keywords: circadian, electrophysiology, mouse, photoperiod Abstract The neuropeptide vasoactive intestinal peptide (VIP) is critical for the proper functioning of the neural circuit that generates circadian rhythms. Mice lacking VIP show profound deficits in the ability to generate many behavioral and physiological rhythms. To explore how the loss of VIP impacts on the intact circadian system, we carried out in vivo multiunit neural activity (MUA) recordings from the suprachiasmatic nucleus of freely moving VIP knockout (KO) mice. The MUA rhythms were largely unaltered in the VIP KO mice, with no significant differences being seen in the amplitude or phase of the rhythms in light–dark conditions. Robust differences between the genotypes were revealed when the mice were transferred from light–dark to constant darkness conditions. In addition, the ability of the VIP KO mice to encode changes in photoperiod was examined. Strikingly, the behavioral and physiological rhythms of VIP KO mice showed no adaptation to short or long photoperiods. The data indicate that the intact circadian system can compensate for some of the consequences of the loss of VIP, whereas this peptide is indispensable for endogenous encoding of seasonal information. -

Kenneth Martin Rosenberg Email: [email protected], [email protected] 660 West Redwood Street, Howard Hall Room 332D, Baltimore, MD, 21201
The impact of the non-immune chemiome on T cell activation Item Type dissertation Authors Rosenberg, Kenneth Publication Date 2020 Abstract T cells are critical organizers of the immune response and rigid control over their activation is necessary for balancing host defense and immunopathology. It takes 3 signals provided by dendritic cells (DC) to fully activate a T cell response – T ce... Keywords signaling; T cell; T-Lymphocytes--immunology Download date 02/10/2021 13:41:58 Link to Item http://hdl.handle.net/10713/14477 Kenneth Martin Rosenberg Email: [email protected], [email protected] 660 West Redwood Street, Howard Hall Room 332D, Baltimore, MD, 21201 EDUCATION MD, University of Maryland, Baltimore, MD Expected May 2022 PhD, University of Maryland, Baltimore, MD December 2020 Graduate Program: Molecular Microbiology and Immunology (MMI) BS, University of Maryland, College Park, MD May 2013 Major: Bioengineering, cum laude University Honors Citation, Gemstone Citation RESEARCH EXPERIENCE UMSOM Microbiology and Immunology Baltimore, MD July 2016-present PhD Candidate Principal Investigator: Dr. Nevil Singh Thesis: The impact of the non-immune chemiome on T cell activation Examined environmental stimuli from classically “non-immune” sources – growth factors, hormones, neurotransmitters, etc. – act to modulate T cell signaling pathways and the functional effects of activating encounters with dendritic cells. UMSOM Anatomy and Neurobiology Baltimore, MD May-August 2015 Rotating student Principal Investigator: Dr. Asaf Keller Studied the role of descending modulation pathways on affective pain transmission. Performed tract- tracing experiments using targeted injection of Cholera toxin subunit B into the lateral parabrachial nucleus and ventrolateral periaqueductal gray of anesthetized transgenic mice. -
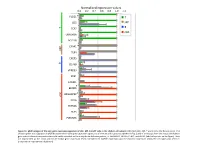
Normalized Expression Values *
Normalized expression values 0.0 0.2 0.4 0.6 0.8 1.0 1.2 PLCG1 * T CD5 MP T B TCF7 cDC UBASH3A BCL11B C5AR1 * MP TLR4 CXCR5 B CD79B VPREB3 XCR1 CADM1 BEND5 * ARGHAP22 * cDC CIITA ZBTB46 FLT3 PLEKHA5 Figure S1. qPCR analysis of the core gene expression signature of cDC, MP, B and T cells in the chicken cell suBsets. RNA from cDC, MP, T and B cells of 2 disUnct pools of 4 chicken spleen was subjected to qPCR detecUon of the core gene expression signatures of immune cell subsets established in Fig. 3 and of transcripts from the mouse and human gene subset selected compendia that could not be detected on the array due to defecUve probes, i.e. ARGHAP22, BEND5, C5AR1, and PLCG1 (labeled by a star on the figure). Data are represented as the mean and SD of relave gene expression levels normalized to GAPDH expression and the maximal expression across the cell types was set to 1 (independent experimental duplicates). B cell T cell cDC Monocyte/MP Chicken Human Mouse Figure S2. Unsupervised hierarchical clustering of orthologous immune response genes across chicken, human and mouse reveals globally conserved clusters of lymphoïd- specific and myeloïd- specific genes. Heatmap of cross-normalized expression profiles for immune response genes present on all three species arrays and regulated at least 2 folds across all cell suBsets, including chicken B cells (c_B), T cells (c_CD3), MP (c_MP) and cDC (c_cDC), human B cells (h_B), T cells (h_CD4_T and h_CD8_T), monocyte-derived MP (h_MoMP), peripheral blood mononucleated cell-derived MP (h_PBMC_MP), non-classical monocytes (h_non- classical_MO), classical monocytes (h_classical_MO), BDCA3+ cDC (h_BDCA3), BDCA1+ cDC (h_BDCA1), murine B cells (m_B), T cells (m_CD4_T and m_CD8_T), peritoneal cavity MP (m_PC_MPII-480HI), lung MP (m_LU_MP), non-classical monocytes (m_non-classical_MO), classical monocytes (m_classical_MO), splenic CD8α+ cDC (m_SP_DC1), suBcutaneous lymph node CD8α+ cDC (m_LN_DC1), splenic CD11B+ cDC (m_SP_DC2), suBcutaneous lymph node CD11B+ cDC (m_LN_DC2). -

Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Amy Sue Bogard University of Tennessee Health Science Center
University of Tennessee Health Science Center UTHSC Digital Commons Theses and Dissertations (ETD) College of Graduate Health Sciences 12-2013 Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Amy Sue Bogard University of Tennessee Health Science Center Follow this and additional works at: https://dc.uthsc.edu/dissertations Part of the Medical Cell Biology Commons, and the Medical Molecular Biology Commons Recommended Citation Bogard, Amy Sue , "Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells" (2013). Theses and Dissertations (ETD). Paper 330. http://dx.doi.org/10.21007/etd.cghs.2013.0029. This Dissertation is brought to you for free and open access by the College of Graduate Health Sciences at UTHSC Digital Commons. It has been accepted for inclusion in Theses and Dissertations (ETD) by an authorized administrator of UTHSC Digital Commons. For more information, please contact [email protected]. Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Document Type Dissertation Degree Name Doctor of Philosophy (PhD) Program Biomedical Sciences Track Molecular Therapeutics and Cell Signaling Research Advisor Rennolds Ostrom, Ph.D. Committee Elizabeth Fitzpatrick, Ph.D. Edwards Park, Ph.D. Steven Tavalin, Ph.D. Christopher Waters, Ph.D. DOI 10.21007/etd.cghs.2013.0029 Comments Six month embargo expired June 2014 This dissertation is available at UTHSC Digital Commons: https://dc.uthsc.edu/dissertations/330 Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells A Dissertation Presented for The Graduate Studies Council The University of Tennessee Health Science Center In Partial Fulfillment Of the Requirements for the Degree Doctor of Philosophy From The University of Tennessee By Amy Sue Bogard December 2013 Copyright © 2013 by Amy Sue Bogard. -

Developmental Regulation of Melanopsin- Containing Retinal Ganglion Cells and Its Effects on Circadian Function
DEVELOPMENTAL REGULATION OF MELANOPSIN- CONTAINING RETINAL GANGLION CELLS AND ITS EFFECTS ON CIRCADIAN FUNCTION by Linda Ruggiero A DISSERTATION Presented to the Neuroscience Graduate Program and the Oregon Health & Science University School of Medicine in partial fulfillment of the requirements for the degree of Doctor of Philosophy October 2008 TABLE OF CONTENTS ACKNOWLEDGEMENTS . .iv LIST OF FIGURES . v ABSTRACT . vii CHAPTER 1 Introduction . 1 Circadian systems and photoentrainment . 2 The Clock . 2 Entrainment . 5 Measuring circadian rhythms . 9 Photoentrainment and the retina . 13 Classical photoreceptive pathways . 14 Photoentrainment and retinal degeneration . 17 Discovery of melanopsin . 21 Melanopsin-containing RGCs and the development of retinal architecture . 24 Development of RGCs . 28 Retinal innervation . 30 Interaction among Photoreceptors . 32 Potential regulation of ipRGCs . 32 SCN organization and retinal input . 34 “Core” and “shell” . 35 Vasoactive Intestinal Peptide . 37 Vasopressin . 38 Additional molecules . 39 SCN outputs . 41 Course of Thesis . 43 CHAPTER 2 The development of melanopsin-containing retinal ganglion cells in mice with early retinal degeneration . 44 Abstract . 46 i Introduction . 47 Materials and Methods . 49 Animals . 49 Wheel-running experiments . 49 Tissue preparation . 50 Characterizing retinal degeneration . 50 Dendritic stratification . 51 Cell numbers and distribution . 52 Pupillometry . 53 Statistics . 53 Results . 54 Light entrainment is altered in CBA/J mice . 54 Time course of retinal degeneration in CBA/J mice . 55 Dendritic stratification of ipRGCs is unaffected by loss of photoreceptors . 55 Potential control of ipRGC number and distribution by photoreceptors . 56 PLR is intact at high light intensities in CBA/J mice . 57 Discussion . 58 CHAPTER 3 Circadian behavior and central processing in mice with early postnatal retinal degeneration . -
Oxygenated Fatty Acids Enhance Hematopoiesis Via the Receptor GPR132
Oxygenated Fatty Acids Enhance Hematopoiesis via the Receptor GPR132 The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Lahvic, Jamie L. 2017. Oxygenated Fatty Acids Enhance Hematopoiesis via the Receptor GPR132. Doctoral dissertation, Harvard University, Graduate School of Arts & Sciences. Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:42061504 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Oxygenated Fatty Acids Enhance Hematopoiesis via the Receptor GPR132 A dissertation presented by Jamie L. Lahvic to The Division of Medical Sciences in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the subject of Developmental and Regenerative Biology Harvard University Cambridge, Massachusetts May 2017 © 2017 Jamie L. Lahvic All rights reserved. Dissertation Advisor: Leonard I. Zon Jamie L. Lahvic Oxygenated Fatty Acids Enhance Hematopoiesis via the Receptor GPR132 Abstract After their specification in early development, hematopoietic stem cells (HSCs) maintain the entire blood system throughout adulthood as well as upon transplantation. The processes of HSC specification, renewal, and homing to the niche are regulated by protein, as well as lipid signaling molecules. A screen for chemical enhancers of marrow transplant in the zebrafish identified the endogenous lipid signaling molecule 11,12-epoxyeicosatrienoic acid (11,12-EET). EET has vasodilatory properties, but had no previously described function on HSCs.