Practical Aspects of Signal Detection in Pharmacovigilance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Safety in Translational Paediatric Research: Practical Points to Consider for Paediatric Safety Profiling and Protocol Development: a Scoping Review
pharmaceutics Review Drug Safety in Translational Paediatric Research: Practical Points to Consider for Paediatric Safety Profiling and Protocol Development: A Scoping Review Beate Aurich 1 and Evelyne Jacqz-Aigrain 1,2,* 1 Department of Pharmacology, Saint-Louis Hospital, 75010 Paris, France; [email protected] 2 Paris University, 75010 Paris, France * Correspondence: [email protected] Abstract: Translational paediatric drug development includes the exchange between basic, clinical and population-based research to improve the health of children. This includes the assessment of treatment related risks and their management. The objectives of this scoping review were to search and summarise the literature for practical guidance on how to establish a paediatric safety specification and its integration into a paediatric protocol. PubMed, Embase, Web of Science, and websites of regulatory authorities and learned societies were searched (up to 31 December 2020). Retrieved citations were screened and full texts reviewed where applicable. A total of 3480 publica- tions were retrieved. No article was identified providing practical guidance. An introduction to the practical aspects of paediatric safety profiling and protocol development is provided by combining health authority and learned society guidelines with the specifics of paediatric research. The paedi- atric safety specification informs paediatric protocol development by, for example, highlighting the Citation: Aurich, B.; Jacqz-Aigrain, E. need for a pharmacokinetic study prior to a paediatric trial. It also informs safety related protocol Drug Safety in Translational Paediatric Research: Practical Points sections such as exclusion criteria, safety monitoring and risk management. In conclusion, safety to Consider for Paediatric Safety related protocol sections require an understanding of the paediatric safety specification. -
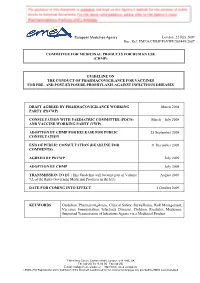
Guideline on the Conduct of Pharmacovigilance for Vaccines for Pre- and Post-Exposure Prophylaxis Against Infectious Diseases
European Medicines Agency London, 22 July 2009 Doc. Ref. EMEA/CHMP/PhVWP/503449/2007 COMMITTEE FOR MEDICINAL PRODUCTS FOR HUMAN USE (CHMP) GUIDELINE ON THE CONDUCT OF PHARMACOVIGILANCE FOR VACCINES FOR PRE- AND POST-EXPOSURE PROPHYLAXIS AGAINST INFECTIOUS DISEASES DRAFT AGREED BY PHARMACOVIGILANCE WORKING March 2008 PARTY (PhVWP) CONSULTATION WITH PAEDIATRIC COMMITTEE (PDCO) March – July 2008 AND VACCINE WORKING PARTY (VWP) ADOPTION BY CHMP FOR RELEASE FOR PUBLIC 25 September 2008 CONSULTATION END OF PUBLIC CONSULTATION (DEADLINE FOR 31 December 2008 COMMENTS) AGREED BY PhVWP July 2009 ADOPTION BY CHMP July 2009 TRANSMISSION TO EC (This Guideline will become part of Volume August 2009 9A of the Rules Governing Medicinal Products in the EU). DATE FOR COMING INTO EFFECT 1 October 2009 KEYWORDS Guideline, Pharmacovigilance, Clinical Safety, Surveillance, Risk Management, Vaccines, Immunisation, Infectious Diseases, Children, Paediatric Medicines, Suspected Transmission of Infectious Agents via a Medicinal Product 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) E-mail: [email protected] http://www.emea.europa.eu ©EMEA 2009 Reproduction and/or distribution of this document is authorised for non commercial purposes only provided the EMEA is acknowledged GUIDELINE ON THE CONDUCT OF PHARMACOVIGILANCE FOR VACCINES FOR PRE- AND POST-EXPOSURE PROPHYLAXIS AGAINST INFECTIOUS DISEASES TABLE OF CONTENTS EXECUTIVE SUMMARY_______________________________________________________ 3 1. Introduction ____________________________________________________________ -

Guidance for Industry E2E Pharmacovigilance Planning
Guidance for Industry E2E Pharmacovigilance Planning U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) April 2005 ICH Guidance for Industry E2E Pharmacovigilance Planning Additional copies are available from: Office of Training and Communication Division of Drug Information, HFD-240 Center for Drug Evaluation and Research Food and Drug Administration 5600 Fishers Lane Rockville, MD 20857 (Tel) 301-827-4573 http://www.fda.gov/cder/guidance/index.htm Office of Communication, Training and Manufacturers Assistance, HFM-40 Center for Biologics Evaluation and Research Food and Drug Administration 1401 Rockville Pike, Rockville, MD 20852-1448 http://www.fda.gov/cber/guidelines.htm. (Tel) Voice Information System at 800-835-4709 or 301-827-1800 U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) April 2005 ICH Contains Nonbinding Recommendations TABLE OF CONTENTS I. INTRODUCTION (1, 1.1) ................................................................................................... 1 A. Background (1.2) ..................................................................................................................2 B. Scope of the Guidance (1.3)...................................................................................................2 II. SAFETY SPECIFICATION (2) ..................................................................................... -

1 Conclusions and Recommendations from the Thirteenth Meeting of the WHO Advisory Committee on Safety of Medicinal Products (ACS
Conclusions and Recommendations from the Thirteenth Meeting of the WHO Advisory Committee on Safety of Medicinal Products (ACSoMP) Geneva, Switzerland 21 - 22 June 2016 The WHO Advisory Committee on Safety of Medicinal Products (ACSoMP) has been constituted to provide advice on pharmacovigilance (PV) policy and issues related to the safety and effectiveness of medicinal products. The conclusions and recommendations from the Tenth meeting of ACSoMP are presented below. Pharmacovigilance (PV) Priorities for World Health Organization (WHO): - Increasing access to essential, quality, safe and affordable medical products is a leadership priority for WHO. The ongoing WHO-reform process is to ensure that the organization is more effective, efficient, responsive, objective, transparent and accountable to its partners and stakeholders. The scope of the Safety and Vigilance (SAV) team within WHO includes: advocacy for safety and vigilance activities, establishing and consolidating partnerships for implementing and advancing the safety and safe use of medical products, strengthening infrastructure, active surveillance and training in pharmacovigilance (PV), and supporting the use of effective tools and systems for monitoring medical products of significant public health importance. - The 2016-2017 priorities for SAV/Medicines Safety are to focus on a few countries, to build capacity and support them through the full cycle of PV activities, from collecting PV data and information, to making regulatory decisions and therapeutic choices based on the collected information. The strategy would be to assess and to improve the quantitative and qualitative aspects of PV activities and outcomes in these countries. The long-term objective is to build comprehensive, sustainable, results-driven PV systems that improve our knowledge, power our decisions and promote the safe use of medicines. -

Ecological Impacts of Veterinary Pharmaceuticals: More Transparency – Better Protection of the Environment
Ecological Impacts of Veterinary Pharmaceuticals: More Transparency – Better Protection of the Environment Avoiding Environmental Pollution from Veterinary Pharmaceuticals To reduce the contamination of air, soil, and bodies of pharmaceuticals more stringently, monitoring systematically water caused by veterinary medicinal products used in their occurrence in the environment, converting animal hus- agriculture and livestock farming, effective measures bandry practices to preserve animals’ health with a minimal must be taken throughout the entire life cycle of these use of antibiotics, and enforcing legal regulations to ensure products – from production and authorisation to appli- implementation of all the measures outlined here. cation and disposal. In the context of the revision of veterinary medicinal products All stakeholders – whether they are farmers, veterinarians, legislation that is currently underway, this background paper consumers, or political decision makers – are called upon focuses on three measures that would contribute to mak- to contribute to reducing contamination of the environment ing information on the occurrence of veterinary drugs in the caused by pharmaceutical residues and to improving pro- environment and their eco-toxicological effects more widely tection of the environment and human health. Appropriate available and enhance protection of the environment from measures include establishing “clean” production plants, contamination with veterinary pharmaceuticals. developing pharmaceuticals with reduced environmental -

CRPT-113Hrpt565-Pt2.Pdf
113TH CONGRESS REPT. 113–565 " ! 2d Session HOUSE OF REPRESENTATIVES Part 2 IMPROVING REGULATORY TRANSPARENCY FOR NEW MEDICAL THERAPIES ACT SEPTEMBER 19, 2014.—Committed to the Committee of the Whole House on the State of the Union and ordered to be printed Mr. GOODLATTE, from the Committee on the Judiciary, submitted the following R E P O R T [To accompany H.R. 4299] [Including cost estimate of the Congressional Budget Office] The Committee on the Judiciary, to whom was referred the bill (H.R. 4299) to amend the Controlled Substances Act with respect to drug scheduling recommendations by the Secretary of Health and Human Services, and with respect to registration of manufac- turers and distributors seeking to conduct clinical testing, having considered the same, report favorably thereon with an amendment and recommend that the bill as amended do pass. CONTENTS Page The Amendment ...................................................................................................... 1 Purpose and Summary ............................................................................................ 2 Background and Need for the Legislation ............................................................. 2 Hearings ................................................................................................................... 3 Committee Consideration ........................................................................................ 3 Committee Votes ..................................................................................................... -

Guidance for Industry Postmarketing Safety Reporting for Human Drug and Biological Products Including Vaccines
Guidance for Industry Postmarketing Safety Reporting for Human Drug and Biological Products Including Vaccines DRAFT GUIDANCE This guidance document is being distributed for comment purposes only. Comments and suggestions regarding this draft document should be submitted within 60 days of publication in the Federal Register of the notice announcing the availability of the draft guidance. Submit comments to Dockets Management Branch (HFA-305), Food and Drug Administration, 5630 Fishers Lane, rm. 1061, Rockville, MD 20857. All comments should be identified with the docket number listed in the notice of availability that publishes in the Federal Register. For questions on the content of the draft document contact (CDER) Min Chen, 301-827- 3169 (phone); 301-827-5190 (fax), or (CBER) Miles Braun, 301-827-3974 (phone); 301- 827-3529 (fax). U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) March 2001 G:\4177dft.doc Guidance for Industry Postmarketing Safety Reporting for Human Drug and Biological Products Including Vaccines Additional copies are available from: Drug Information Branch (HFD-210) Center for Drug Evaluation and Research (CDER) 5600 Fishers Lane, Rockville, MD 20857 (Tel) 301-827-4570 Internet at http://www.fda.gov/cder/guidance/index.htm or Office of Communication, Training and Manufacturers Assistance (HFM-40) Center for Biologics Evaluation and Research (CBER) 1401 Rockville Pike, Rockville, MD 20852-1448 (Fax) 1-888-CBERFAX or 301-827-3844 (Voice Information) 1-800-835-4709 or 301-827-1800 Internet at http://www.fda.gov/cber/guidelines.htm U.S. -

Unlocking the Power of Pharmacovigilance* an Adaptive Approach to an Evolving Drug Safety Environment
Unlocking the power of pharmacovigilance* An adaptive approach to an evolving drug safety environment PricewaterhouseCoopers’ Health Research Institute Contents Executive summary 01 Background 02 The challenge to the pharmaceutical industry 02 Increased media scrutiny 02 Greater regulatory and legislative scrutiny 04 Investment in pharmacovigilance 05 The reactive nature of pharmacovigilance 06 Unlocking the power of pharmacovigilance 07 Organizational alignment 07 Operations management 07 Data management 08 Risk management 10 The three strategies of effective pharmacovigilance 11 Strategy 1: Align and clarify roles, responsibilities, and communications 12 Strategy 2: Standardize pharmacovigilance processes and data management 14 Strategy 3: Implement proactive risk minimization 20 Conclusion 23 Endnotes 24 Glossary 25 Executive summary The idea that controlled clinical incapable of addressing shifts in 2. Standardize pharmacovigilance trials can establish product safety public expectations and regulatory processes and data management and effectiveness is a core principle and media scrutiny. This reality has • Align operational activities across of the pharmaceutical industry. revealed issues in the four areas departments and across sites Neither the clinical trials process involved in patient safety operations: • Implement process-driven standard nor the approval procedures of the organizational alignment, operations operating procedures, work U.S. Food and Drug Administration management, data management, and instructions, and training -

Causality in Pharmacoepidemiology and Pharmacovigilance: a Theoretical Excursion
DOI: 10.1590/1980-5497201700030010 ARTIGO ORIGINAL / ORIGINAL ARTICLE Causalidade em farmacoepidemiologia e farmacovigilância: uma incursão teórica Causality in Pharmacoepidemiology and Pharmacovigilance: a theoretical excursion Daniel Marques MotaI,II, Ricardo de Souza KuchenbeckerI RESUMO: O artigo teceu algumas considerações sobre causalidade em farmacoepidemiologia e farmacovigilância. Inicialmente, fizemos uma breve introdução sobre a importância do tema, ressaltando que o entendimento da relação causal é considerado como uma das maiores conquistas das ciências e que tem sido, ao longo dos tempos, uma preocupação contínua e central de filósofos e epidemiologistas. Na sequência, descrevemos as definições e os tipos de causas, demonstrando suas influências no pensamento farmacoepidemiológico. Logo a seguir, apresentamos o modelo multicausal de Rothman como um dos fundantes para a explicação da causalidade múltipla, e o tema da determinação da causalidade. Concluímos com alguns comentários e reflexões sobre causalidade na perspectiva da vigilância sanitária, particularmente, para as ações de regulação em farmacovigilância. Palavras-chave: Aplicações da epidemiologia. Causalidade. Efeitos colaterais e reações adversas relacionados a medicamentos. Farmacoepidemiologia. Farmacovigilância. Vigilância sanitária. IPrograma de Pós-Graduação em Epidemiologia, Faculdade de Medicina, Universidade Federal do Rio Grande do Sul – Porto Alegre (RS), Brasil. IIAgência Nacional de Vigilância Sanitária – Brasília (DF), Brasil. Autor correspondente: Daniel Marques Mota. Programa de Pós-Gradução em Epidemiologia da Faculdade de Medicina da Universidade Federal do Rio Grande do Sul. Rua Ramiro Barcelos, 2.400, 2º andar, CEP: 90035-003, Porto Alegre, RS, Brasil. E-mail: [email protected] Conflito de interesses: nada a declarar – Fonte de financiamento: nenhuma. 475 REV BRAS EPIDEMIOL JUL-SET 2017; 20(3): 475-486 MOTA, D.M., KUCHENBECKER, R.S. -

Guidance for Industry
Assessing User Fees Under the Prescription Drug User Fee Amendments of 2017 Guidance for Industry U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) November 2020 User Fees Assessing User Fees Under the Prescription Drug User Fee Amendments of 2017 Guidance for Industry Additional copies are available from: Office of Communications, Division of Drug Information Center for Drug Evaluation and Research Food and Drug Administration 10001 New Hampshire Ave., Hillandale Bldg., 4th Floor Silver Spring, MD 20993-0002 Phone: 855-543-3784 or 301-796-3400; Fax: 301-431-6353 Email: [email protected] https://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm and/or Office of Communication, Outreach and Development Center for Biologics Evaluation and Research Food and Drug Administration 10903 New Hampshire Ave., Bldg. 71, Room 3128 Silver Spring, MD 20993-0002 Phone: 800-835-4709 or 240-402-8010 Email: [email protected] https://www.fda.gov/vaccines-blood-biologics/guidance-compliance-regulatory-information-biologics/biologics- guidances U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) November 2020 User Fees Contains Nonbinding Recommendations TABLE OF CONTENTS I. INTRODUCTION............................................................................................................ -

Consulting the Controlled Substance Staff on Drug Abuse Potential and Labeling, Drug Scheduling, Dependence Liability and Drug Abuse Risks to the Public Health
MANUAL OF POLICIES AND PROCEDURES CENTER FOR DRUG EVALUATION AND RESEARCH MAPP 4200.3 Rev. 1 POLICY AND PROCEDURES OFFICE OF THE CENTER DIRECTOR Consulting the Controlled Substance Staff on Drug Abuse Potential and Labeling, Drug Scheduling, Dependence Liability and Drug Abuse Risks to the Public Health Table of Contents PURPOSE ..............................................................................1 BACKGROUND ...................................................................1 POLICY .................................................................................2 PROCEDURES .....................................................................4 REFERENCES ......................................................................6 DEFINITIONS ......................................................................6 CHANGE CONTROL TABLE ............................................8 PURPOSE This MAPP establishes responsibilities and procedures in the Center for Drug Evaluation and Research (CDER) for consulting the Controlled Substance Staff (CSS) regarding the evaluation of drug abuse potential and labeling, drug scheduling, dependence liability, and drug abuse risks to the public health. This MAPP also provides a description of the role of CSS in the drug abuse assessment and the drug scheduling process within CDER. BACKGROUND CSS provides expertise to the Food and Drug Administration (FDA) Centers and CDER Offices and Divisions as part of the review process in assessing drugs for abuse potential and dependence liability. CSS fulfills -

Prandin (Repaglinide) Tablets
DEPARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 NDA 020741/S-044 SUPPLEMENT APPROVAL Clinipace, Inc. Agent for Gemini Laboratories, LLC Attention: Catherine Kessler Vice President 4840 Pearl E Cir, Ste 201E Boulder, CO 80301 Dear Ms. Kessler: Please refer to your Supplemental New Drug Application (sNDA) dated and received June 29, 2018, and your amendments, submitted under section 505(b) of the Federal Food, Drug, and Cosmetic Act (FDCA) for Prandin (repaglinide) tablets. This Prior Approval supplemental new drug application provides for revisions to the prescribing information (PI) to conform to the Pregnancy and Lactation Labeling Rule (PLLR). APPROVAL & LABELING We have completed our review of this supplemental application, as amended. It is approved, effective on the date of this letter, for use as recommended in the enclosed, agreed-upon labeling text with the minor editorial revisions, listed below, and reflected in the enclosed labeling. • In the HIGHLIGHTS OF PRESCRIBING INFORMATION, the date has been revised to 1/2019. • The footer on all pages has been deleted. WAIVER OF ½ PAGE LENGTH REQUIREMENT FOR HIGHLIGHTS We are waiving the requirements of 21 CFR 201.57(d)(8) regarding the length of Highlights of Prescribing Information. This waiver applies to all future supplements containing revised labeling unless we notify you otherwise. Reference ID: 4378916 NDA 020741/S-044 Page 2 CONTENT OF LABELING As soon as possible, but no later than 14 days from the date of this letter, submit the content of labeling [21 CFR 314.50(l)] in structured product labeling (SPL) format using the FDA automated drug registration and listing system (eLIST), as described at http://www.fda.gov/ForIndustry/DataStandards/StructuredProductLabeling/default.htm.