1. the Origins of a Commitment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

From Track to Tarmac
Federation Faces and Introduction A guided walk around the streets and laneways Places of North Sydney focusing on our Federation connections, including the former residences of A walking tour of Federation Sir Joseph Palmer Abbott, Sir Edmund Barton faces and places in North and Dugald Thomson. Along the walk, view the Sydney changes in the North Sydney landscape since th Federation and the turn of the 20 century. Distance: 6 Km Approximate time: 4 hours At the turn of the year 1900 to 1901 the city of Grading: medium to high Sydney went mad with joy. For a few days hope ran so high that poets and prophets declared Australia to be on the threshold of a golden age… from early morning on the first of January 1901 trams, trains and ferry boats carried thousands of people into the city for the greatest day of their history: the inauguration of the Commonwealth of Australia. It was to be a people‟s festival. Manning Clark, Historian It was also a people‟s movement and 1901 was the culmination of many years of discussions, community activism, heated public debates, vibrant speeches and consolidated actions. In 1890 the Australasian Federal Conference was held in Melbourne and the following year in Sydney. In 1893 a meeting of the various federation groups, including the Australian Native Association was held at Corowa. A plan was developed for the election of delegates to a convention. In the mid to late 1890s it was very much a peoples‟ movement gathering groundswell support. In 1896 a People‟s Convention with 220 delegates and invited guests from all of the colonies took place at Bathurst - an important link in the Federation chain. -

Harbour Bridge to South Head and Clovelly
To NEWCASTLE BARRENJOEY A Harbour and Coastal Walk Personal Care This magnificent walk follows the south-east shoreline of Sydney Harbour The walk requires average fitness. Take care as it includes a variety of before turning southwards along ocean beaches and cliffs. It is part of one pathway conditions and terrain including hills and steps. Use sunscreen, of the great urban coast walks of the world, connecting Broken Bay in carry water and wear a hat and good walking shoes. Please observe official SYDNEY HARBOUR Sydney's north to Port Hacking to its south (see Trunk Route diagram), safety and track signs at all times. traversing the rugged headlands and sweeping beaches, bush, lagoons, bays, and harbours of coastal Sydney. Public Transport The walk covered in this map begins at the Circular Quay connection with Public transport is readily available at regular points along the way Harbour Bridge the Harbour Circle Walk and runs to just past coastal Bronte where it joins (see map). This allows considerable flexibility in entering and exiting the Approximate Walking Times in Hours and Minutes another of the series of maps covering this great coastal and harbour route. routes. Note - not all services operate every day. to South Head e.g. 1 hour 45 minutes = 1hr 45 The main 29 km Harbour Bridge (B3) to South Head (H1) and to Clovelly Bus, train and ferry timetables. G8) walk (marked in red on the map) is mostly easy but fascinating walk- Infoline Tel: 131-500 www.131500.com.au 0 8 ing. Cutting a 7km diagonal across the route between Rushcutters Bay (C5) and Clovelly kilometres and Clovelly, is part of the Federation Track (also marked in red) which, in Short Walks using Public Transport Brochure 1 To Manly NARRABEEN full, runs from Queensland to South Australia. -

List of Accredited Chest Clinics (By State)
ACT Health Clinical Placement Office 2016 List of Accredited Chest clinics (By State) ACT Canberra Hospital TB Services Department of Contact: 02 6244 2066/ 02 6244 2702 Thoracic Medicine The Canberra Hospital PO Box 11 Woden ACT 2606 New South Wales Central Coast Local Health District Gosford Hospital Contact: TB Prevention & Control Service (Chest Clinic) Appt: 4320 3388 PO Box 361 Gosford NSW 2250 Only Mon 8.30-3; Tues & Fri 8.30-4 Illawarra and Shoalhaven LHD The Wollongong Hospital Contact: 4253 4138 Department of Respiratory Medicine Crown Street Wollongong NSW 2500 Nepean Blue Mountains Local Health District Nepean Hospital Contact: 4734 2536 Chest Clinic Outpatients Department PO Box 63 Penrith NSW 2751 Northern Sydney Local Health District Hornsby Ku-ring-gai Hospital Contact: 9477 9318 Palmerston Road Hornsby NSW 2077 New Royal North Shore Hospital Contact: 9926 7905 Chest Clinic Level 8, Dept. of Respiratory Medicine St Leonards NSW 2065 Manly District Hospital Contact: 9976 9542 Chest Clinic Manly NSW 2095 South Eastern Sydney LHD - Northern Network Prince of Wales Hospital Contact: 9382 4643/ 9382 4672 Department of Respiratory Medicine Level 2 Dickinson Building Barker Street Randwick NSW 2031 Sydney Hospital Contact: 9382 7535 Chest Clinic Macquarie Street Sydney NSW 2000 St. Vincent's Hospital Contact: 8382 3150 Heart-Lung Ambulatory Care Level 4, Xavier Building 390 Victoria Street Darlinghurst NSW 2010 South Eastern Sydney LHD - Central Network ACT Health Clinical Placement Office 2016 St George Hospital Contact: 9113 -

Golden Yearbook
Golden Yearbook Golden Yearbook Stories from graduates of the 1930s to the 1960s Foreword from the Vice-Chancellor and Principal ���������������������������������������������������������5 Message from the Chancellor ��������������������������������7 — Timeline of significant events at the University of Sydney �������������������������������������8 — The 1930s The Great Depression ������������������������������������������ 13 Graduates of the 1930s ���������������������������������������� 14 — The 1940s Australia at war ��������������������������������������������������� 21 Graduates of the 1940s ����������������������������������������22 — The 1950s Populate or perish ���������������������������������������������� 47 Graduates of the 1950s ����������������������������������������48 — The 1960s Activism and protest ������������������������������������������155 Graduates of the 1960s ���������������������������������������156 — What will tomorrow bring? ��������������������������������� 247 The University of Sydney today ���������������������������248 — Index ����������������������������������������������������������������250 Glossary ����������������������������������������������������������� 252 Produced by Marketing and Communications, the University of Sydney, December 2016. Disclaimer: The content of this publication includes edited versions of original contributions by University of Sydney alumni and relevant associated content produced by the University. The views and opinions expressed are those of the alumni contributors and do -

A Short Resumé of the History of Sydney Hospital
A SHORT RESUME OF THE HISTORY OF SYDNEY HOSPITAL, By ELSA MOORE, Sydney. When the first colony was founded in Street Girls' School. Macquarie chose the Australia it was at Dawes Point. The site for the Sydney Hospital, on an elevated barracks and houses were built around that ridge along which he formed a new street point, although the main town and ware• and named it after himself. The building houses were situated at Parramatta, The *was to stand in seven acres of ground and first hospital, which was called the Sydney to be of "noble proportions". He was cen• Infirmary, was built on the shores of sured for these plans, which were said to Sydney Cove, now Circular Quay, in 1788, be on far too large a scale for such a small by twelve convicts from the First Fleet. colony. The plans were really drawn up by When Governor Macquarie arrived in Mrs. Macquarie, who made a great hobby Sydney he ordered the Infirmary to be of architecture. It has also been said that moved to Dawes Point; the old brick build• she influenced the Governor in the selection ing is now used as classrooms by the Fort of the site for the hospital In those days HISTORY OF SYDNEY HOSPITAL 83 women were not supposed to take any part He and, later, Dr. Balmain, were also given in public affairs; hence her name was kept land grants which are now the suburbs in the background. Macquarie also was which bear their names. The non-medical prominently associated with the planning of staff consisted of an overseer, an atten• Parliament House and of the building dant who acted as clerk, a gate-keeper, a called The Mint. -

AIA REGISTER Jan 2015
AUSTRALIAN INSTITUTE OF ARCHITECTS REGISTER OF SIGNIFICANT ARCHITECTURE IN NSW BY SUBURB Firm Design or Project Architect Circa or Start Date Finish Date major DEM Building [demolished items noted] No Address Suburb LGA Register Decade Date alterations Number [architect not identified] [architect not identified] circa 1910 Caledonia Hotel 110 Aberdare Street Aberdare Cessnock 4702398 [architect not identified] [architect not identified] circa 1905 Denman Hotel 143 Cessnock Road Abermain Cessnock 4702399 [architect not identified] [architect not identified] 1906 St Johns Anglican Church 13 Stoke Street Adaminaby Snowy River 4700508 [architect not identified] [architect not identified] undated Adaminaby Bowling Club Snowy Mountains Highway Adaminaby Snowy River 4700509 [architect not identified] [architect not identified] circa 1920 Royal Hotel Camplbell Street corner Tumut Street Adelong Tumut 4701604 [architect not identified] [architect not identified] 1936 Adelong Hotel (Town Group) 67 Tumut Street Adelong Tumut 4701605 [architect not identified] [architect not identified] undated Adelonia Theatre (Town Group) 84 Tumut Street Adelong Tumut 4701606 [architect not identified] [architect not identified] undated Adelong Post Office (Town Group) 80 Tumut Street Adelong Tumut 4701607 [architect not identified] [architect not identified] undated Golden Reef Motel Tumut Street Adelong Tumut 4701725 PHILIP COX RICHARDSON & TAYLOR PHILIP COX and DON HARRINGTON 1972 Akuna Bay Marina Liberator General San Martin Drive, Ku-ring-gai Akuna Bay Warringah -

The New South Wales Parliament Under Siege
‘Build your House of Parliament upon the River’: The New South Wales Parliament under siege Gareth Griffith and Mark Swinson * You must build your House of Parliament upon the river . the populace cannot exact their demands by sitting down round you. — The Duke of Wellington This piece of advice is attributed to the Duke of Wellington, a man who knew about such things as pickets and blockades, but also about Parliament and its ways. On Tuesday 19 June 2001, a part of the populace associated with the trade union movement, determined to have its demands satisfied, massed round the New South Wales Parliament House. For those who do not know it, the New South Wales Parliament is not built on a river, or a harbour for that matter, but on the crest of a modest rise, fronted by Macquarie Street to the west and, at the rear, by Hospital Road and beyond that by a spacious open area called the Domain. To the north side is the State Library building; to the other, Sydney Hospital. At its height, in the early afternoon of 19 June, the Parliament was surrounded by a demonstration estimated to be 1,000 strong. The Premier called it a ‘blockade’. 1 Unionists called it a ‘picket’. 2 Some press reports referred to it as a ‘riot’. 3 * Gareth Griffith is a Senior Research Officer with the New South Wales Parliamentary Library; Mark Swinson is Deputy Clerk of the Legislative Assembly, Parliament of New South Wales. 1 L. McIIveen, ‘House is shut down by union blockade’, The Sydney Morning Herald , 20 June 2001; G. -

BROOKLYN ESTUARY PROCESS STUDY (VOLUME I of II) By
BROOKLYN ESTUARY PROCESS STUDY (VOLUME I OF II) by Water Research Laboratory Manly Hydraulics Laboratory The Ecology Lab Coastal and Marine Geosciences The Centre for Research on Ecological Impacts of Coastal Cities Edited by B M Miller and D Van Senden Technical Report 2002/20 June 2002 (Issued October 2003) THE UNIVERSITY OF NEW SOUTH WALES SCHOOL OF CIVIL AND ENVIRONMENTAL ENGINEERING WATER RESEARCH LABORATORY BROOKLYN ESTUARY PROCESS STUDY WRL Technical Report 2002/20 June 2002 by Water Research Laboratory Manly Hydraulics Laboratory The Ecology Lab Coastal and Marine Geosciences The Centre for Research on Ecological Impacts of Coastal Cities Edited by B M Miller D Van Senden (Issued October 2003) - i - Water Research Laboratory School of Civil and Environmental Engineering Technical Report No 2002/20 University of New South Wales ABN 57 195 873 179 Report Status Final King Street Date of Issue October 2003 Manly Vale NSW 2093 Australia Telephone: +61 (2) 9949 4488 WRL Project No. 00758 Facsimile: +61 (2) 9949 4188 Project Manager B M Miller Title BROOKLYN ESTUARY PROCESS STUDY Editor(s) B M Miller, D Van Senden Client Name Hornsby Shire Council Client Address PO Box 37 296 Pacific Highway HORNSBY NSW 1630 Client Contact Jacqui Grove Client Reference Major Involvement by: Brett Miller (WRL), David van Senden (MHL), William Glamore (WRL), Ainslie Fraser (WRL), Matt Chadwick (WRL), Peggy O'Donnell (TEL), Michele Widdowson (MHL), Bronson McPherson (MHL), Sophie Diller (TEL), Charmaine Bennett (TEL), John Hudson (CMG), Theresa Lasiak (CEICC) and Tony Underwood (CEICC). The work reported herein was carried out at the Water Research Laboratory, School of Civil and Environmental Engineering, University of New South Wales, acting on behalf of the client. -

Act Three: Scene One the View from Above
Act Three: The View from Above Scene One The DMR observer in the helicopter was Hal Gregge. He describes what it was like looking down from above: “Anything on a main road is our responsibility, so with a thing like the ferries, the buck stops with us. The helicopter pilot was called Noel and the fellow we were reporting to was Bill McIntyre who was running the workshop at Granville. That was our central workshop - we had all trades and 400 people working there then. We used to support all the ferries from there - they had riggers and people like that and we’d overhaul the ferry engines there. We used to have the patterns to cast the spider wheels, even. It’s all closed down now, though. Bill was organising ground support. He’s retired now. “By the time the helicopter got up to Wisemans, we found noth- ing there. Noel is a very good pilot. He did his training all over the world and has been under fire and everything, so we were able to fly quite low at times when we needed to. We zoomed in around Webbs Creek. There was a set of piers there that they normally tie the ferry to, but of course they were empty. We went around the corner to the piles for the other two ferries, but they’d gone, too. So we just followed the river down at a reasonable height. It wasn’t a bad day on the Tuesday - the flood was well up, but the cloud and rain were gone. -

Sydney Eye Hospital
Br J Ophthalmol: first published as 10.1136/bjo.66.10.617 on 1 October 1982. Downloaded from British Journal ofOphthalmology, 1982, 66, 617-621 Sydney Eye Hospital LENNOX PRICE From Sydney Eye Hospital, Sir John Young Crescent, Woolloomooloo 2011, New South Wales, Australia SUMMARY This year, 1982, marks the centenary of the Sydney Eye Hospital, originally the ophthalmic department of the old Sydney Infirmary, which was founded with the settlement of the Colony in 1788. Established in 1882, the hospital was transferred to its present site 60 years ago, and it still provides ward accommodation. After alternating periods of stagnation and progress the new hospital (stage 1) was completed in 1974, with modern clinic and research facilities. It is now the largest eye hospital in the southern hemisphere and is a first-class referral centre with an annual attendance of 75000. The Department of Ophthalmology, University of Sydney, is based at the hospital, providing undergraduate instruction and a comprehensive postgraduate training programme for Australian ophthalmologists and others in more distant continents. This year the Sydney Eye Hospital celebrates its New South Wales and even neighbouring colonies' centenary. The early history of the hospital is closely (Sydney Hospital Annual Report, 1877). Forty years linked to that of its parent institution, the old Sydney later (1922) the population of Sydney had increased Infirmary, which was founded by Governor Philip, to over three-quarters of a million. The original who set foot on the shores of Sydney Cove on 26 buildings of the Eye Hospital had become January 1788, and proceeded to establish a convict dilapidated, and the board determined that it should settlement 'in the reign of his most sacred majesty be moved to a fresh site a short distance across http://bjo.bmj.com/ George the Third' (Fig. -

Annual Report 03/04
Services and facilities Addresses and telephone numbers of Department of Health and selected services 205 Map and profiles of Metropolitan Area Health Services 206 Map and profiles of Rural Area Health Services 210 Profiles of Statewide Services 213 Glossary of terms 214 Compliance index 216 Index 217 Annual report production costs 225 NSW Department of Health Annual Report 203 Services and facilities 204 NSW Department of Health Annual Report ADDRESSES AND TELEPHONE NUMBERS OF DEPARTMENT OF HEALTH AND SELECTED SERVICES Department of Health Pharmaceutical Services Branch Selected services North Sydney Office Building 20 NSW Multicultural Health 73 Miller Street Gladesville Hospital Campus Communication Service North Sydney NSW 2060 Victoria Road Level 1 (Locked Mail Bag 961 Gladesville NSW 1675 North Block North Sydney NSW 2059) (PO Box 103 Sydney Hospital Gladesville NSW 1675) Tel. 9391 9000 Macquarie Street Fax. 9391 9101 Tel. 9879 3214 Sydney NSW 2000 Fax. 9859 5165 (GPO Box 1614 Director-General Robyn Kruk Sydney NSW 2001) Methadone Program Business hours 9.00am–5.00pm Tel. 9382 7516 Tel. 9879 5246 Monday to Friday Fax. 9382 7517 Fax. 9859 5170 Foveaux Street Site Manager Peter Todard Enquires relating to 28 Foveaux Street authorities to prescribe Business hours 8.30am–5.00pm Surry Hills NSW 2010 other drugs of addiction Monday to Friday Business hours 8.30am–5.00pm Tel. 9879 5239 Department of Forensic Medicine Monday to Friday Fax. 9859 5175 50 Parramatta Road Glebe NSW 2037 Better Health Centre Chief Pharmacist and Director (PO Box 90 Publications Warehouse John Lumby (Locked Mail Bag 5003 Glebe NSW 2037) Business hours 8.30am–5.30pm Gladesville NSW 2111) Tel. -
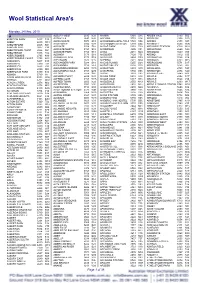
Wool Statistical Area's
Wool Statistical Area's Monday, 24 May, 2010 A ALBURY WEST 2640 N28 ANAMA 5464 S15 ARDEN VALE 5433 S05 ABBETON PARK 5417 S15 ALDAVILLA 2440 N42 ANCONA 3715 V14 ARDGLEN 2338 N20 ABBEY 6280 W18 ALDERSGATE 5070 S18 ANDAMOOKA OPALFIELDS5722 S04 ARDING 2358 N03 ABBOTSFORD 2046 N21 ALDERSYDE 6306 W11 ANDAMOOKA STATION 5720 S04 ARDINGLY 6630 W06 ABBOTSFORD 3067 V30 ALDGATE 5154 S18 ANDAS PARK 5353 S19 ARDJORIE STATION 6728 W01 ABBOTSFORD POINT 2046 N21 ALDGATE NORTH 5154 S18 ANDERSON 3995 V31 ARDLETHAN 2665 N29 ABBOTSHAM 7315 T02 ALDGATE PARK 5154 S18 ANDO 2631 N24 ARDMONA 3629 V09 ABERCROMBIE 2795 N19 ALDINGA 5173 S18 ANDOVER 7120 T05 ARDNO 3312 V20 ABERCROMBIE CAVES 2795 N19 ALDINGA BEACH 5173 S18 ANDREWS 5454 S09 ARDONACHIE 3286 V24 ABERDEEN 5417 S15 ALECTOWN 2870 N15 ANEMBO 2621 N24 ARDROSS 6153 W15 ABERDEEN 7310 T02 ALEXANDER PARK 5039 S18 ANGAS PLAINS 5255 S20 ARDROSSAN 5571 S17 ABERFELDY 3825 V33 ALEXANDRA 3714 V14 ANGAS VALLEY 5238 S25 AREEGRA 3480 V02 ABERFOYLE 2350 N03 ALEXANDRA BRIDGE 6288 W18 ANGASTON 5353 S19 ARGALONG 2720 N27 ABERFOYLE PARK 5159 S18 ALEXANDRA HILLS 4161 Q30 ANGEPENA 5732 S05 ARGENTON 2284 N20 ABINGA 5710 18 ALFORD 5554 S16 ANGIP 3393 V02 ARGENTS HILL 2449 N01 ABROLHOS ISLANDS 6532 W06 ALFORDS POINT 2234 N21 ANGLE PARK 5010 S18 ARGYLE 2852 N17 ABYDOS 6721 W02 ALFRED COVE 6154 W15 ANGLE VALE 5117 S18 ARGYLE 3523 V15 ACACIA CREEK 2476 N02 ALFRED TOWN 2650 N29 ANGLEDALE 2550 N43 ARGYLE 6239 W17 ACACIA PLATEAU 2476 N02 ALFREDTON 3350 V26 ANGLEDOOL 2832 N12 ARGYLE DOWNS STATION6743 W01 ACACIA RIDGE 4110 Q30 ALGEBUCKINA