[Product Monograph Template
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ipriflavone in the Treatment of Postmenopausal Osteoporosis a Randomized Controlled Trial
ORIGINAL CONTRIBUTION Ipriflavone in the Treatment of Postmenopausal Osteoporosis A Randomized Controlled Trial Peter Alexandersen, MD Context Data on the efficacy and safety of ipriflavone for prevention of postmeno- Anne Toussaint, MD pausal bone loss are conflicting. Claus Christiansen, MD, PhD Objectives To investigate the effect of oral ipriflavone on prevention of postmeno- pausal bone loss and to assess the safety profile of long-term treatment with iprifla- Jean-Pierre Devogelaer, MD, PhD vone in postmenopausal osteoporotic women. Christian Roux, MD, PhD Design and Setting Prospective, randomized, double-blind, placebo-controlled, 4-year Jacques Fechtenbaum, MD, PhD study conducted in 4 centers in Belgium, Denmark, and Italy from August 1994 to July 1998. Carlo Gennari, MD, PhD Participants Four hundred seventy-four postmenopausal white women, aged 45 Jean Yves Reginster, MD, PhD to 75 years, with bone mineral densities (BMDs) of less than 0.86 g/cm2. for the Ipriflavone Multicenter Interventions Patients were randomly assigned to receive ipriflavone, 200 mg 3 times European Fracture Study per day (n = 234), or placebo (n = 240); all received 500 mg/d of calcium. TUDIES OF IPRIFLAVONE, A SYN- Main Outcome Measures Efficacy measures included spine, hip, and forearm BMD thetic isoflavone derivative, have and biochemical markers of bone resorption (urinary hydroxyproline corrected for cre- atinine and urinary CrossLaps [Osteometer Biotech, Herlev, Denmark] corrected for suggested that it inhibits bone re- creatinine), assessed every 6 months. Laboratory safety measures and adverse events sorption and stimulates osteo- were recorded every 3 months. Sblast activity in vitro in cell cultures1,2 and Results Based on intent-to-treat analysis, after 36 months of treatment, the annual in vivo in experimental models of osteo- 3 percentage change from baseline in BMD of the lumbar spine for ipriflavone vs pla- porosis. -

Botanicals in Postmenopausal Osteoporosis
nutrients Review Botanicals in Postmenopausal Osteoporosis Wojciech Słupski, Paulina Jawie ´nand Beata Nowak * Department of Pharmacology, Wroclaw Medical University, ul. J. Mikulicza-Radeckiego 2, 50-345 Wrocław, Poland; [email protected] (W.S.); [email protected] (P.J.) * Correspondence: [email protected]; Tel.: +48-607-924-471 Abstract: Osteoporosis is a systemic bone disease characterized by reduced bone mass and the deterioration of bone microarchitecture leading to bone fragility and an increased risk of fractures. Conventional anti-osteoporotic pharmaceutics are effective in the treatment and prophylaxis of osteoporosis, however they are associated with various side effects that push many women into seeking botanicals as an alternative therapy. Traditional folk medicine is a rich source of bioactive compounds waiting for discovery and investigation that might be used in those patients, and therefore botanicals have recently received increasing attention. The aim of this review of literature is to present the comprehensive information about plant-derived compounds that might be used to maintain bone health in perimenopausal and postmenopausal females. Keywords: osteoporosis; menopause; botanicals; herbs 1. Introduction Women’s health and quality of life is modulated and affected strongly by hormone status. An oestrogen level that changes dramatically throughout life determines the Citation: Słupski, W.; Jawie´n,P.; development of women’s age-associated diseases. Age-associated hormonal imbalance Nowak, B. Botanicals in and oestrogen deficiency are involved in the pathogenesis of various diseases, e.g., obesity, Postmenopausal Osteoporosis. autoimmune disease and osteoporosis. Many female patients look for natural biological Nutrients 2021, 13, 1609. https:// products deeply rooted in folk medicine as an alternative to conventional pharmaceutics doi.org/10.3390/nu13051609 used as the prophylaxis of perimenopausal health disturbances. -

Bisphosphonates Can Be Safely Given to Patients with Hypercalcemia And
Clinical Research in Practice: The Journal of Team Hippocrates Volume 5 | Issue 1 Article 11 2019 Bisphosphonates can be safely given to patients with hypercalcemia and renal insufficiency secondary to multiple myeloma Matthew .J Miller Wayne State University School of Medicine, [email protected] Follow this and additional works at: https://digitalcommons.wayne.edu/crp Part of the Endocrinology, Diabetes, and Metabolism Commons, Medical Education Commons, Nephrology Commons, and the Translational Medical Research Commons Recommended Citation MILLER MJ. Bisphosphonates can be safely given to patients with hypercalcemia and renal insufficiency secondary to multiple myeloma. Clin. Res. Prac. 2019 Mar 14;5(1):eP1846. doi: 10.22237/crp/1552521660 This Critical Analysis is brought to you for free and open access by the Open Access Journals at DigitalCommons@WayneState. It has been accepted for inclusion in Clinical Research in Practice: The ourJ nal of Team Hippocrates by an authorized editor of DigitalCommons@WayneState. VOL 5 ISS 1 / eP1846 / MARCH 14, 2019 doi: 10.22237/crp/1552521660 Bisphosphonates can be safely given to patients with hypercalcemia and renal insufficiency secondary to multiple myeloma MATTHEW J. MILLER, B.S., Wayne State University School of Medicine, [email protected] ABSTRACT A critical appraisal and clinical application of Itou K, Fukuyama T, Sasabuchi Y, et al. Safety and efficacy of oral rehydration therapy until 2 h before surgery: a multicenter randomized controlled trial. Journal of Anesthesia. 2012;26(1):20-27. doi: 10.1007/s00540-011-1261-x. Keywords: bisphosphonates, nephrotoxicity, safety, renal insufficiency, renal failure, multiple myeloma, pamidronate, ibandronate, zaledronic acid Clinical Context An 83-year-old African-American female with a history of multiple vertebral compression fractures and gastritis presented for the second time in two weeks with symptoms of hypercalcemia. -

Nutriceuticals: Over-The-Counter Products and Osteoporosis
serum calcium levels are too low, and adequate calcium is not provided by the diet, calcium is taken from bone. Osteoporosis: Clinical Updates Long- term dietary calcium deficiency is a known risk Osteoporosis Clinical Updates is a publication of the National factor for osteo porosis. The recommended daily cal- Osteoporosis Foundation (NOF). Use and reproduction of this publication for educational purposes is permitted and cium intake from diet and supplements combined is encouraged without permission, with proper citation. This 1000 mg/day for people aged 19 to 50 and 1200 mg/ publication may not be used for commercial gain. NOF is a day for people older than 50. For all ages, the tolerable non-profit, 501(c)(3) educational organization. Suggested upper limit is 2500 mg calcium per day. citation: National Osteoporosis Foundation. Osteoporosis Clinical Updates. Issue Title. Washington, DC; Year. Adequate calcium intake is necessary for attaining peak bone mass in early life (until about age 30) and for Please direct all inquiries to: National Osteoporosis slowing the rate of bone loss in later life.3 Although Foundation 1150 17th Street NW Washington, DC 20037, calcium alone (or with vitamin D) has not been shown USA Phone: 1 (202) 223-2226 to prevent estrogen-related bone loss, multiple stud- Fax: 1 (202) 223-1726 www.nof.org ies have found calcium consumption between 650 mg Statement of Educational Purpose and over 1400 mg/day reduces bone loss and increases Osteoporosis Clinical Updates is published to improve lumbar spine BMD.4-6 osteoporosis patient care by providing clinicians with state-of-the-art information and pragmatic strategies on How to take calcium supplements: prevention, diagnosis, and treatment that they may apply in Take calcium supplements with food. -

834FM.1 ZOLEDRONIC ACID and IBANDRONIC ACID for ADJUVANT TREATMENT in EARLY BREAST CANCER PATIENTS (Amber Initiation Guideline for Ibandronic Acid)
834FM.1 ZOLEDRONIC ACID AND IBANDRONIC ACID FOR ADJUVANT TREATMENT IN EARLY BREAST CANCER PATIENTS (Amber Initiation Guideline for Ibandronic Acid) This guideline provides prescribing and monitoring advice for oral ibandronic acid therapy which may or may not follow zoledronic acid infusions in secondary care. It should be read in conjunction with the Summary of Product Characteristics (SPC) available on www.medicines.org.uk/emc and the BNF. BACKGROUND FOR USE Bisphosphonates are indicated for reduction in the risk of developing bone metastases and risk of death from breast cancer in post-menopausal patients who have had curative treatment for breast cancer, i.e. this is an adjuvant treatment. A meta-analysis of individual participant data from 26 randomised controlled trials (RCTs) including 18,766 women with early breast cancer (the Early Breast Cancer Trialists' Collaborative Group [EBCTCG] meta- analysis 2015) has shown that at 10 years the absolute reductions in the risk of breast cancer mortality, bone recurrence and all-cause mortality in post-menopausal women were 3.3%, 2.2% and 2.3% respectively. Bone fractures were also reduced by 15%, which is highly relevant as many of the patients offered adjuvant bisphosphonates will also be recommended to have adjuvant aromatase inhibitor treatment that can cause loss of bone density and bone fractures. In line with cancer services in Oxfordshire and other areas, we have chosen to use zoledronic acid for intravenous administration and ibandronic acid for oral administration due to availability and relatively low cost. These medications are licensed for use in patients with osteoporosis and metastatic breast cancer. -

Zoledronic Acid Teva, INN-Zoledronic Acid
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Zoledronic Acid Teva 4 mg/5 ml concentrate for solution for infusion 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One vial with 5 ml concentrate contains 4 mg zoledronic acid (as monohydrate). One ml concentrate contains 0.8 mg zoledronic acid (as monohydrate). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Concentrate for solution for infusion (sterile concentrate). Clear and colourless solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications - Prevention of skeletal related events (pathological fractures, spinal compression, radiation or surgery to bone, or tumour-induced hypercalcaemia) in adult patients with advanced malignancies involving bone. - Treatment of adult patients with tumour-induced hypercalcaemia (TIH). 4.2 Posology and method of administration Zoledronic Acid Teva must only be prescribed and administered to patients by healthcare professionals experienced in the administration of intravenous bisphosphonates. Posology Prevention of skeletal related events in patients with advanced malignancies involving bone Adults and older people The recommended dose in the prevention of skeletal related events in patients with advanced malignancies involving bone is 4 mg zoledronic acid every 3 to 4 weeks. Patients should also be administered an oral calcium supplement of 500 mg and 400 IU vitamin D daily. The decision to treat patients with bone metastases for the prevention of skeletal related events should consider that the onset of treatment effect is 2-3 months. Treatment of TIH Adults and older people The recommended dose in hypercalcaemia (albumin-corrected serum calcium ≥ 12.0 mg/dl or 3.0 mmol/l) is a single dose of 4 mg zoledronic acid. -

Ipriflavone: an Important Bone-Building Isoflavone
Ipriflavone: An Important Bone-Building Isoflavone Kathleen A. Head, N.D. Abstract Ipriflavone, an isoflavone synthesized from the soy isoflavone daidzein, holds great promise in the prevention and treatment of osteoporosis and other metabolic bone diseases. It has been widely studied in humans and found effective for inhibiting bone resorption and enhancing bone formation, the net result being an increase in bone density and a decrease in fracture rates in osteoporotic women. While ipriflavone appears to enhance estrogen’s effect, it does not possess intrinsic estrogenic activity, making it an attractive adjunct or alternative to conventional hormone replacement therapy. Preliminary studies have also found ipriflavone effective in preventing bone loss associated with chronic steroid use, immobility, ovariectomy, renal osteodystro- phy, and gonadotrophin hormone-releasing hormone agonists. In addition, it holds prom- ise for the treatment of other metabolic diseases affecting the bones, including Paget’s disease of the bone, hyperparathyroidism, and tinnitus caused by otosclerosis. (Altern Med Rev 1999;4(1):10-22) Introduction Ipriflavone (chemical structure: 7-isopropoxyisoflavone), derived from the soy isoflavone, daidzein, holds great promise for osteoporosis prevention and treatment (see Figure 1). Ipriflavone (IP) was discovered in the 1930s but has only recently begun to be embraced by the medical community in this country. Over 150 studies on safety and effective- ness, both animal and human, have been conducted in Italy, Hungary, and Japan. As of 1997, 2,769 patients had been treated a total of 3,132 patient years.1 Pharmacokinetics IP is metabolized mainly in the liver and excreted in the urine. Food appears to enhance its absorption. -

Zoledronic Acid Injection Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use Zoledronic Acid Injection safely and effectively. See full prescribing information for Zoledronic Acid Injection. • Adequately rehydrate patients with hypercalcemia of malignancy Zoledronic Acid Injection prior to administration of Zoledronic Acid Injection and monitor electrolytes during treatment. (5.2) for intravenous use • Renal toxicity may be greater in patients with renal impairment. Do Initial U.S. Approval: 2001 not use doses greater than 4 mg. Treatment in patients with severe renal impairment is not recommended. Monitor serum creatinine -------------------------RECENT MAJOR CHANGES--------------------- before each dose. (5.3) • Osteonecrosis of the jaw has been reported. Preventive dental exams Warnings and Precautions, Osteonecrosis of the Jaw (5.4) 06/2015 should be performed before starting Zoledronic Acid Injection. Avoid invasive dental procedures. (5.4) -------------------------INDICATIONS AND USAGE------------------------ • Severe incapacitating bone, joint, and/or muscle pain may occur. Zoledronic Acid Injection is a bisphosphonate indicated for the Discontinue Zoledronic Acid Injection if severe symptoms occur. treatment of: (5.5) • Hypercalcemia of malignancy. (1.1) • Zoledronic Acid Injection can cause fetal harm. Women of • Patients with multiple myeloma and patients with documented bone childbearing potential should be advised of the potential hazard to metastases from solid tumors, in conjunction with standard the fetus and to avoid becoming pregnant. (5.9, 8.1) antineoplastic therapy. Prostate cancer should have progressed after • Atypical subtrochanteric and diaphyseal femoral fractures have been treatment with at least one hormonal therapy. (1.2) reported in patients receiving bisphosphonate therapy. These Important limitation of use: The safety and efficacy of Zoledronic Acid fractures may occur after minimal or no trauma. -
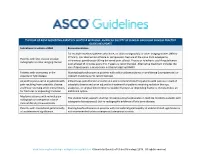
The Role of Bone Modifying
THE ROLE OF BONE MODIFYING AGENTS IN MULTIPLE MYELOMA: AMERICAN SOCIETY OF CLINICAL ONCOLOGY CLINICAL PRACTICE GUIDELINE UPDATE Indications to initiate a BMA Recommendation For multiple myeloma patients who have, on plain radiograph(s) or other imaging studies (MRI or CT Scan), lytic destruction of bone or compression fracture of the spine from osteopenia, Patients with lytic disease on plain intravenous pamidronate 90 mg delivered over at least 2 hours or zoledronic acid 4 mg delivered radiographs or other imaging studies over at least 15 minutes every 3 to 4 weeks is recommended. Alternative treatment includes the use of denosumab, a monoclonal antibody targeting RANKL. Patients with osteopenia in the Starting bisphosphonates in patients with solitary plasmacytoma or smoldering (asymptomatic) or absence of lytic disease indolent myeloma is not recommended. Adjunct to pain control in patients with Intravenous pamidronate or zoledronic acid is recommended for patients with pain as a result of pain resulting from osteolytic disease osteolytic disease and as an adjunctive treatment for patients receiving radiation therapy, and those receiving other interventions analgesics, or surgical intervention to stabilize fractures or impending fractures. Denosumab is an for fractures or impending fractures additional option. Myeloma patients with normal plain The Update Panel supports starting intravenous bisphosphonates in multiple myeloma patients with radiograph or osteopenia in bone osteopenia (osteoporosis) but no radiographic evidence of lytic bone disease. mineral density measurements Patients with monoclonal gammopathy Starting bisphosphonates in patients with monoclonal gammopathy of undetermined significance is of undetermined significance not recommended unless osteopenia (osteoporosis) exists. www.asco.org/hematologic-malignancies-guidelines ©American Society of Clinical Oncology 2018. -

PRODUCT MONOGRAPH Pr Zoledronic Acid
PRODUCT MONOGRAPH Pr Zoledronic Acid - A (zoledronic acid injection) 5 mg/100 mL solution for intravenous infusion Bone Metabolism Regulator Sandoz Canada Inc. Date of Revision: 145 Jules-Léger June 01, 2016 Boucherville, QC, Canada J4B 7K8 Control No. : TBD Zoledronic Acid – A Page 1 of 62 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ............................................................ 3 SUMMARY PRODUCT INFORMATION ........................................................................... 3 INDICATIONS AND CLINICAL USE ................................................................................. 3 CONTRAINDICATIONS ....................................................................................................... 4 WARNINGS AND PRECAUTIONS ..................................................................................... 4 ADVERSE REACTIONS ..................................................................................................... 10 DOSAGE AND ADMINISTRATION ................................................................................. 25 OVERDOSAGE ..................................................................................................................... 27 ACTION AND CLINICAL PHARMACOLOGY............................................................... 27 STORAGE AND STABILITY ............................................................................................. 30 SPECIAL HANDLING INSTRUCTIONS .......................................................................... 30 -

Current and Potential Future Drug Treatments for Osteoporosis
700 Annals ofthe Rheumatic Diseases 1996;55:700-714 REVIEW Ann Rheum Dis: first published as 10.1136/ard.55.10.700 on 1 October 1996. Downloaded from Current and potential future drug treatments for osteoporosis Sanjeev Patel Osteoporosis is the most common metabolic ture risk increases by a factor of 1.5 to 3.0.6 bone disease in the developed world and is Other determinants of osteoporotic fracture increasingly recognised as an important public are shown in table 1. health problem.' There is marked worldwide Drugs active on bone can be simplistically variation in its incidence. It is predicted that classified as those that inhibit bone resorption the incidence of hip fractures caused by or those that stimulate bone formation (table osteoporosis will increase, particularly in 2). The effects of these drugs on bone mineral developing countries.2 The human burden of density are summarised in fig 1. Drugs that osteoporosis is considerable, with increased stimulate bone formation lead to a direct morbidity and mortality, especially following increase in bone mineral density, whereas those osteoporotic hip fractures.' The current finan- that inhibit bone resorption result in limited cial burden is substantial, with estimated yearly increases in bone mineral density by costs of £750 million in the UK,' $10 billion in uncoupling bone turnover and allowing forma- the USA, and FF3.7 billion in France.3 The tion to continue in excess of resorption. This ability to measure bone mineral density and leads to an increase in bone mineral density thereby monitor response to intervention has due to filling in of the remodelling space (the been vital in the development ofpharmacologi- remodelling transient).7 It has been suggested cal treatments. -

The Role of BMP Signaling in Osteoclast Regulation
Journal of Developmental Biology Review The Role of BMP Signaling in Osteoclast Regulation Brian Heubel * and Anja Nohe * Department of Biological Sciences, University of Delaware, Newark, DE 19716, USA * Correspondence: [email protected] (B.H.); [email protected] (A.N.) Abstract: The osteogenic effects of Bone Morphogenetic Proteins (BMPs) were delineated in 1965 when Urist et al. showed that BMPs could induce ectopic bone formation. In subsequent decades, the effects of BMPs on bone formation and maintenance were established. BMPs induce proliferation in osteoprogenitor cells and increase mineralization activity in osteoblasts. The role of BMPs in bone homeostasis and repair led to the approval of BMP 2 by the Federal Drug Administration (FDA) for anterior lumbar interbody fusion (ALIF) to increase the bone formation in the treated area. However, the use of BMP 2 for treatment of degenerative bone diseases such as osteoporosis is still uncertain as patients treated with BMP 2 results in the stimulation of not only osteoblast mineralization, but also osteoclast absorption, leading to early bone graft subsidence. The increase in absorption activity is the result of direct stimulation of osteoclasts by BMP 2 working synergistically with the RANK signaling pathway. The dual effect of BMPs on bone resorption and mineralization highlights the essential role of BMP-signaling in bone homeostasis, making it a putative therapeutic target for diseases like osteoporosis. Before the BMP pathway can be utilized in the treatment of osteoporosis a better understanding of how BMP-signaling regulates osteoclasts must be established. Keywords: osteoclast; BMP; osteoporosis Citation: Heubel, B.; Nohe, A. The Role of BMP Signaling in Osteoclast Regulation.