Bisphosphonates Can Be Safely Given to Patients with Hypercalcemia And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

834FM.1 ZOLEDRONIC ACID and IBANDRONIC ACID for ADJUVANT TREATMENT in EARLY BREAST CANCER PATIENTS (Amber Initiation Guideline for Ibandronic Acid)
834FM.1 ZOLEDRONIC ACID AND IBANDRONIC ACID FOR ADJUVANT TREATMENT IN EARLY BREAST CANCER PATIENTS (Amber Initiation Guideline for Ibandronic Acid) This guideline provides prescribing and monitoring advice for oral ibandronic acid therapy which may or may not follow zoledronic acid infusions in secondary care. It should be read in conjunction with the Summary of Product Characteristics (SPC) available on www.medicines.org.uk/emc and the BNF. BACKGROUND FOR USE Bisphosphonates are indicated for reduction in the risk of developing bone metastases and risk of death from breast cancer in post-menopausal patients who have had curative treatment for breast cancer, i.e. this is an adjuvant treatment. A meta-analysis of individual participant data from 26 randomised controlled trials (RCTs) including 18,766 women with early breast cancer (the Early Breast Cancer Trialists' Collaborative Group [EBCTCG] meta- analysis 2015) has shown that at 10 years the absolute reductions in the risk of breast cancer mortality, bone recurrence and all-cause mortality in post-menopausal women were 3.3%, 2.2% and 2.3% respectively. Bone fractures were also reduced by 15%, which is highly relevant as many of the patients offered adjuvant bisphosphonates will also be recommended to have adjuvant aromatase inhibitor treatment that can cause loss of bone density and bone fractures. In line with cancer services in Oxfordshire and other areas, we have chosen to use zoledronic acid for intravenous administration and ibandronic acid for oral administration due to availability and relatively low cost. These medications are licensed for use in patients with osteoporosis and metastatic breast cancer. -

Zoledronic Acid Teva, INN-Zoledronic Acid
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Zoledronic Acid Teva 4 mg/5 ml concentrate for solution for infusion 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One vial with 5 ml concentrate contains 4 mg zoledronic acid (as monohydrate). One ml concentrate contains 0.8 mg zoledronic acid (as monohydrate). For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Concentrate for solution for infusion (sterile concentrate). Clear and colourless solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications - Prevention of skeletal related events (pathological fractures, spinal compression, radiation or surgery to bone, or tumour-induced hypercalcaemia) in adult patients with advanced malignancies involving bone. - Treatment of adult patients with tumour-induced hypercalcaemia (TIH). 4.2 Posology and method of administration Zoledronic Acid Teva must only be prescribed and administered to patients by healthcare professionals experienced in the administration of intravenous bisphosphonates. Posology Prevention of skeletal related events in patients with advanced malignancies involving bone Adults and older people The recommended dose in the prevention of skeletal related events in patients with advanced malignancies involving bone is 4 mg zoledronic acid every 3 to 4 weeks. Patients should also be administered an oral calcium supplement of 500 mg and 400 IU vitamin D daily. The decision to treat patients with bone metastases for the prevention of skeletal related events should consider that the onset of treatment effect is 2-3 months. Treatment of TIH Adults and older people The recommended dose in hypercalcaemia (albumin-corrected serum calcium ≥ 12.0 mg/dl or 3.0 mmol/l) is a single dose of 4 mg zoledronic acid. -

Zoledronic Acid Injection Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use Zoledronic Acid Injection safely and effectively. See full prescribing information for Zoledronic Acid Injection. • Adequately rehydrate patients with hypercalcemia of malignancy Zoledronic Acid Injection prior to administration of Zoledronic Acid Injection and monitor electrolytes during treatment. (5.2) for intravenous use • Renal toxicity may be greater in patients with renal impairment. Do Initial U.S. Approval: 2001 not use doses greater than 4 mg. Treatment in patients with severe renal impairment is not recommended. Monitor serum creatinine -------------------------RECENT MAJOR CHANGES--------------------- before each dose. (5.3) • Osteonecrosis of the jaw has been reported. Preventive dental exams Warnings and Precautions, Osteonecrosis of the Jaw (5.4) 06/2015 should be performed before starting Zoledronic Acid Injection. Avoid invasive dental procedures. (5.4) -------------------------INDICATIONS AND USAGE------------------------ • Severe incapacitating bone, joint, and/or muscle pain may occur. Zoledronic Acid Injection is a bisphosphonate indicated for the Discontinue Zoledronic Acid Injection if severe symptoms occur. treatment of: (5.5) • Hypercalcemia of malignancy. (1.1) • Zoledronic Acid Injection can cause fetal harm. Women of • Patients with multiple myeloma and patients with documented bone childbearing potential should be advised of the potential hazard to metastases from solid tumors, in conjunction with standard the fetus and to avoid becoming pregnant. (5.9, 8.1) antineoplastic therapy. Prostate cancer should have progressed after • Atypical subtrochanteric and diaphyseal femoral fractures have been treatment with at least one hormonal therapy. (1.2) reported in patients receiving bisphosphonate therapy. These Important limitation of use: The safety and efficacy of Zoledronic Acid fractures may occur after minimal or no trauma. -
The Role of Bone Modifying
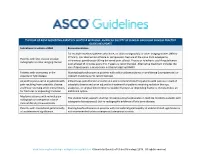
THE ROLE OF BONE MODIFYING AGENTS IN MULTIPLE MYELOMA: AMERICAN SOCIETY OF CLINICAL ONCOLOGY CLINICAL PRACTICE GUIDELINE UPDATE Indications to initiate a BMA Recommendation For multiple myeloma patients who have, on plain radiograph(s) or other imaging studies (MRI or CT Scan), lytic destruction of bone or compression fracture of the spine from osteopenia, Patients with lytic disease on plain intravenous pamidronate 90 mg delivered over at least 2 hours or zoledronic acid 4 mg delivered radiographs or other imaging studies over at least 15 minutes every 3 to 4 weeks is recommended. Alternative treatment includes the use of denosumab, a monoclonal antibody targeting RANKL. Patients with osteopenia in the Starting bisphosphonates in patients with solitary plasmacytoma or smoldering (asymptomatic) or absence of lytic disease indolent myeloma is not recommended. Adjunct to pain control in patients with Intravenous pamidronate or zoledronic acid is recommended for patients with pain as a result of pain resulting from osteolytic disease osteolytic disease and as an adjunctive treatment for patients receiving radiation therapy, and those receiving other interventions analgesics, or surgical intervention to stabilize fractures or impending fractures. Denosumab is an for fractures or impending fractures additional option. Myeloma patients with normal plain The Update Panel supports starting intravenous bisphosphonates in multiple myeloma patients with radiograph or osteopenia in bone osteopenia (osteoporosis) but no radiographic evidence of lytic bone disease. mineral density measurements Patients with monoclonal gammopathy Starting bisphosphonates in patients with monoclonal gammopathy of undetermined significance is of undetermined significance not recommended unless osteopenia (osteoporosis) exists. www.asco.org/hematologic-malignancies-guidelines ©American Society of Clinical Oncology 2018. -

PRODUCT MONOGRAPH Pr Zoledronic Acid
PRODUCT MONOGRAPH Pr Zoledronic Acid - A (zoledronic acid injection) 5 mg/100 mL solution for intravenous infusion Bone Metabolism Regulator Sandoz Canada Inc. Date of Revision: 145 Jules-Léger June 01, 2016 Boucherville, QC, Canada J4B 7K8 Control No. : TBD Zoledronic Acid – A Page 1 of 62 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ............................................................ 3 SUMMARY PRODUCT INFORMATION ........................................................................... 3 INDICATIONS AND CLINICAL USE ................................................................................. 3 CONTRAINDICATIONS ....................................................................................................... 4 WARNINGS AND PRECAUTIONS ..................................................................................... 4 ADVERSE REACTIONS ..................................................................................................... 10 DOSAGE AND ADMINISTRATION ................................................................................. 25 OVERDOSAGE ..................................................................................................................... 27 ACTION AND CLINICAL PHARMACOLOGY............................................................... 27 STORAGE AND STABILITY ............................................................................................. 30 SPECIAL HANDLING INSTRUCTIONS .......................................................................... 30 -

The Role of BMP Signaling in Osteoclast Regulation
Journal of Developmental Biology Review The Role of BMP Signaling in Osteoclast Regulation Brian Heubel * and Anja Nohe * Department of Biological Sciences, University of Delaware, Newark, DE 19716, USA * Correspondence: [email protected] (B.H.); [email protected] (A.N.) Abstract: The osteogenic effects of Bone Morphogenetic Proteins (BMPs) were delineated in 1965 when Urist et al. showed that BMPs could induce ectopic bone formation. In subsequent decades, the effects of BMPs on bone formation and maintenance were established. BMPs induce proliferation in osteoprogenitor cells and increase mineralization activity in osteoblasts. The role of BMPs in bone homeostasis and repair led to the approval of BMP 2 by the Federal Drug Administration (FDA) for anterior lumbar interbody fusion (ALIF) to increase the bone formation in the treated area. However, the use of BMP 2 for treatment of degenerative bone diseases such as osteoporosis is still uncertain as patients treated with BMP 2 results in the stimulation of not only osteoblast mineralization, but also osteoclast absorption, leading to early bone graft subsidence. The increase in absorption activity is the result of direct stimulation of osteoclasts by BMP 2 working synergistically with the RANK signaling pathway. The dual effect of BMPs on bone resorption and mineralization highlights the essential role of BMP-signaling in bone homeostasis, making it a putative therapeutic target for diseases like osteoporosis. Before the BMP pathway can be utilized in the treatment of osteoporosis a better understanding of how BMP-signaling regulates osteoclasts must be established. Keywords: osteoclast; BMP; osteoporosis Citation: Heubel, B.; Nohe, A. The Role of BMP Signaling in Osteoclast Regulation. -

[Product Monograph Template
PRODUCT MONOGRAPH Pr ZOLEDRONIC ACID INJECTION 5 mg / 100 mL zoledronic acid (as zoledronic acid monohydrate) Solution for intravenous infusion Bone Metabolism Regulator Manufacturer: Dr. Reddy’s Laboratories Limited Bachupally 500 090 – INDIA Imported/Distributed By: Date of Revision: August 1, 2019 Dr. Reddy’s Laboratories Canada Inc. Mississauga, ON L4W 4Y1 Canada Submission Control Number: 228238 1 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ..................................................................... 3 SUMMARY PRODUCT INFORMATION .................................................................................... 3 INDICATIONS AND CLINICAL USE ......................................................................................... 3 CONTRAINDICATIONS ............................................................................................................... 4 WARNINGS AND PRECAUTIONS ............................................................................................. 4 ADVERSE REACTIONS ............................................................................................................. 10 DRUG INTERACTIONS.............................................................................................................. 24 DOSAGE AND ADMINISTRATION ......................................................................................... 25 OVERDOSAGE ............................................................................................................................ 27 ACTION AND CLINICAL -

Bisphosphonate IV Therapy Zoledronic Acid (Zometa ) and Pamidronate (Aredia )
Bisphosphonate IV Therapy Zoledronic Acid (Zometa®) and Pamidronate (Aredia®) Bisphosphonates (biss FOSS fo nates) are a class of drug that include zoledronic (zoe leh DRAWN ik) acid, under the brand name Zometa® (zoh METTA) and pamidronate (pamih DRO nayt), under the brand name Aredia®. This medicine is used to make bones stronger and prevent bone fractures. These medicines are given directly into a vein through an IV (intravenous) therapy treatment. This way of giving medicine is called an infusion. The first dose of zoledronic acid or pamidronate is given in the hospital. Your child will stay overnight so the nurse can record the response to the medicine. Before Starting this Medicine A blood test will be done before the first dose of this medicine and from time to time during the treatment. Tell your child’s doctor about all medicines your child is taking. Include any changes in medicines. Tell your child’s doctor if she could be pregnant. If your child is allergic to bisphosphonates, he or she should not take this medicine. Possible Side Effects Side effects often lessen over the course of treatment. Side effects may include: . Flu-like symptoms such as fever or pain in bones or joints . Signs of low calcium like muscle cramps, muscle spasms, numbness or tingling . Signs of low phosphorous like muscle weakness or mental changes . Allergic reaction (see the section When to Call for Emergency Help on page 2) A rare side effect of this medicine is osteonecrosis of the jaw (part of the jaw bone dies ). This is usually seen only in adults who have dental problems. -

Renal Complications from Bisphosphonate Treatment
REVIEW CURRENT OPINION Renal complications from bisphosphonate treatment Raimund Hirschberg Purpose of review More than 10 years ago evidence emerged that bisphosphonate therapy especially in malignant bone diseases is associated with renal complications. The nature of renal injury from bisphosphonates has become clearer in recent years. Recent findings Pamidronate can rarely cause (collapsing) focal segmental glomerular sclerosis with the nephrotic syndrome and renal insufficiency. This renal complication has also been observed with other bisphosphonates but only in isolated cases. Other types of renal injury include transient but self-limited rises in creatinine, and, very rarely, acute tubular necrosis causing acute renal failure. The frequency of the latter two complications appears to follow the potency of different bisphosphonates. Although thus far no tubular transport for bisphosphonates has been identified (renal excretion appears to be only by glomerular ultrafiltration), the occurrence of tubular cell injury gives rise for the possibility that these cells can take up bisphosphonates. In patients receiving bisphosphonates monitoring of serum creatinine before and after intravenous (i.v.) dosing or periodically with oral bisphosphonates is advised. Summary Renal complications with bisphosphonates are rare but creatinine monitoring, especially with i.v. bisphosphonates is strongly advised. The mechanisms by which bisphosphonates can cause renal insufficiency are still elusive and opportunities for research include the discovery of potential mechanisms of tubular cell uptake of bisphosphonates. Keywords acute kidney injury, nephrotic syndrome, renal handling of bisphosphonates INTRODUCTION cause apoptosis (Table 1) [1]. Nitrogenic bisphosph- Bisphosphonates are chemically related to pyro- onates have additional actions once internalized phosphate but contain a carbon with two side into osteoclasts (Table 1). -

Prolonged Zoledronic Acid-Induced Hypocalcemia in Hypercalcemia of Malignancy
CaseCommunity Report Report Prolonged zoledronic acid-induced hypocalcemia in hypercalcemia of malignancy Shraddha Narechania, MD,a Nirosshan Tiruchelvam, MD,a Chetan Lokhande, MD,b Gaurav Kistangari, MD,c and Hamed Daw, MDd aDepartment of Internal Medicine, bOutcomes Research, cDepartment of Hospital Medicine, and dDepartment of Hematology and Oncology, Fairview Hospital, Cleveland, Ohio oledronic acid is a parenteral long-acting value, <2 pmol/L), PTH of 10 pg/ml (normal range, bisphosphonate that has been shown to 15-65 pg/ml), creatinine of 1.1 mg/dL, and creati- Zbe more efective than other bisphospho- nine clearance of approximately 65 ml/min (normal nates in treating hypercalcemia of malignancy. It is range, 88-128 ml/min). Testing for her vitamin D important to be aware of its ability to induce pro- level was not done. longed and severe hypocalcemia (hypoCa) follow- Te patient received treatment with intravenous ing administration, which can be difcult to con- (IV) fuids, calcitonin, and a single 3.3-mg dose of trol despite aggressive calcium replacement. We IV zoledronic acid. After 6 days of treatment, her report on a patient with metastatic breast cancer calcium levels decreased to 12.1 mg/dL, and she was who presented with severe symptomatic hypoCa discharged home. She received her frst session of after receiving zoledronic acid for hypercalcemia of palliative chemotherapy a week after her discharge. malignancy. Two weeks after the zoledronic acid treatment, the patient presented to the hospital with diarrhea as Case presentation and summary well as tingling and numbness all over the body. A A 51-year-old woman was diagnosed with right- physical examination of the patient was remarkable sided breast cancer in 2012 for which she under- for carpopedal spasm of her upper extremities. -

Efficacy of a Cathepsin K Inhibitor in a Preclinical Model for Prevention and Treatment of Breast Cancer Bone Metastasis
Author Manuscript Published OnlineFirst on September 23, 2014; DOI: 10.1158/1535-7163.MCT-14-0253 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Efficacy of a Cathepsin K Inhibitor in a Preclinical Model for Prevention and Treatment of Breast Cancer Bone Metastasis Le T. Duong1, Gregg A. Wesolowski, Patrick Leung, Renata Oballa*, Maureen Pickarski Merck & Co. Inc., Whitehouse Station, NJ, USA. Running Title: Cathepsin K inhibitor for metastatic bone disease Keywords: Cathepsin K inhibitor, osteoclast, metastatic bone disease, osteolysis, breast cancer. 1Author for correspondence: Le T. Duong, Ph.D. Bone Biology Merck & Co., Inc. 770 Sumneytown Pike West Point, PA 19486, USA Tel. 215-652-7574 Fax: 215-652-4328 E-mail: [email protected] Funding Statement - This study was funded by Merck & Co., Whitehouse Station, NJ, USA Downloaded from mct.aacrjournals.org on September 27, 2021. © 2014 American Association for Cancer Research. Author Manuscript Published OnlineFirst on September 23, 2014; DOI: 10.1158/1535-7163.MCT-14-0253 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Cathepsin K inhibitor for metastatic bone disease Le T. Duong Bone Biology Merck & Co., Inc. 770 Sumneytown Pike West Point, PA 19486, USA Tel. 215-652-7574 Fax: 215-652-4328 E-mail: [email protected] Gregg A. Wesolowski Bone Biology Merck & Co., Inc. 770 Sumneytown Pike West Point, PA 19486, USA E-mail: [email protected] Patrick Leung Bone Biology Merck & Co., Inc. 770 Sumneytown Pike West Point, PA 19486, USA E-mail: [email protected] *Renata Oballa Inception Sciences Canada Inc. -

Diagnosis and Treatment of Osteoporosis
Supporting Evidence: Diagnosis and Treatment of Osteoporosis The subdivisions of this section are: • References Copyright © 2017 by Institute for Clinical Systems Improvement 1 Diagnosis and Treatment of Osteoporosis Ninth Edition/July 2017 References Abrahamsen B, Eiken P, Eastell R. Cumulative alendronate dose and the long-term absolute risk of subtrochanteric and diaphyseal femur fractures: a register-based national cohort analysis. J Clin Endocrinol Metab 2010;95:5258-65. Adami S, Libanati C, Boonen S, et al. Denosumab treatment in postmenopausal women with osteo- porosis does not interfere with fracture-healing. J Bone Joint Surg Am 2012;94:2113-19. Adler RA, El-Hajj Fuleihan G, Bauer DC, et al. Managing osteoporosis in patients on long-term bisphos- phonate treatment: report of a task force of the American society for bone and mineral research. J Bone Miner Res 2016;31:16-35. Alekel DL, St Germain A, Peterson CT, et al. Isoflavone-rich soy protein isolate attenuates bone loss in the lumbar spine of perimenopausal women. Am J Clin Nutr 2000;72:844-52. Alexandersen P, Toussaint A, Christiansen, et al. for the Ipriflavone Multicenter European Fracture Study. Ipriflavone in the treatment of postmenopausal osteoporosis: a randomized controlled trial. JAMA 2001;285:1482-88. Anastasilakis AD, Polyzos SA, Makras P, et al. Clinical features of 24 patients with rebound-associated vertebral fractures after denosumab discontinuation: systematic review and additional cases. J Bone Miner Res 2017. Andrews EB, Gilsenan AW, Midkiff K, et al. The US postmarketing surveillance study of adult osteosarcoma and teriparatide: study design and findings from the first 7 years.