Novel Addition for Iop Reduction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Two Phase 3 Clinical Trials Comparing the Safety and Efficacy of Netarsudil to Timolol in Patients with Elevated Intraocular
Two Phase 3 Clinical Trials Comparing the Safety and Efficacy of Netarsudil to Timolol in Patients With Elevated Intraocular Pressure: Rho Kinase Elevated IOP Treatment Trial 1 and 2 (ROCKET-1 and ROCKET-2) JANET B. SERLE, L. JAY KATZ, EUGENE MCLAURIN, THERESA HEAH, NANCY RAMIREZ-DAVIS, DALE W. USNER, GARY D. NOVACK, AND CASEY C. KOPCZYNSKI, FOR THE ROCKET-1 AND ROCKET-2 STUDY GROUPS PURPOSE: To evaluate the efficacy and ocular and sys- ROCKET-2) for timolol (P < .0001 for netarsudil vs temic safety of netarsudil 0.02% ophthalmic solution, a timolol). rho-kinase inhibitor and norepinephrine transporter in- CONCLUSIONS: In 2 large, randomized, double-masked hibitor, in patients with open-angle glaucoma and ocular trials reported here, once-daily dosing of netarsudil hypertension. 0.02% was found to be effective and well tolerated for DESIGN: Double-masked, randomized noninferiority the treatment of patients with ocular hypertension and clinical trials: Rho Kinase Elevated IOP Treatment Trial open-angle glaucoma. The novel pharmacology and 1 and 2 (ROCKET-1 and ROCKET-2). aqueous humor dynamic effects of this molecule suggest METHODS: After a washout of all pre-study ocular hy- it may be a useful addition to the armamentarium of potensive medications, eligible patients were randomized ocular hypotensive medications. (Am J Ophthalmol to receive netarsudil 0.02% once daily (q.d.), timolol 2018;186:116–127. Ó 2017 The Authors. Published 0.5% twice a day (b.i.d.), and (ROCKET-2 only) netar- by Elsevier Inc. This is an open access article under the sudil 0.02% b.i.d. -
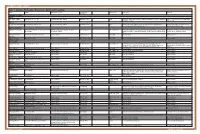
Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg
OPTOMETRIC STUDY CENTER Table 1. Glaucoma Medications: Mechanisms, Dosing and Precautions Brand Generic Mechanism of Action Dosage/Avg. % Product Sizes Side Effects Warnings Reduction CHOLINERGIC AGENTS Direct Pilocarpine (generic) Pilocarpine 1%, 2%, 4% Increases trabecular outflow BID-QID/15-25% 15ml Headache, blurred vision, myopia, retinal detachment, bronchiole constriction, Angle closure, shortness of breath, retinal narrowing of angle detachment Indirect Phospholine Iodide (Pfizer) Echothiophate iodide 0.125% Increases trabecular outflow QD-BID/15-25% 5ml Same as above plus cataractogenic iris cysts in children, pupillary block, Same as above, plus avoid prior to any increased paralysis with succinylcholine general anesthetic procedure ALPHA-2 AGONISTS Alphagan P (Allergan) Brimonidine tartrate 0.1%, 0.15% with Purite Decreases aqueous production, increases BID-TID/up to 26% 5ml, 10ml, 15ml Dry mouth, hypotension, bradycardia, follicular conjunctivitis, ocular irritation, Monitor for shortness of breath, dizziness, preservative uveoscleral outflow pruritus, dermatitis, conjunctival blanching, eyelid retraction, mydriasis, drug ocular redness and itching, fatigue allergy Brimonidine tartrate Brimonidine tartrate 0.15%, 0.2% Same as above Same as above 5ml, 10ml Same as above Same as above (generic) Iopidine (Novartis) Apraclonidine 0.5% Decreases aqueous production BID-TID/up to 25% 5ml, 10ml Same as above but higher drug allergy (40%) Same as above BETA-BLOCKERS Non-selective Betagan (Allergan) Levobunolol 0.25%, 0.5% Decreases -
Rhopressa™ Netarsudil Ophthalmic Solution 0.02%
Rhopressa™ Netarsudil ophthalmic solution 0.02% CDER Dermatologic and Ophthalmic Drugs Advisory Committee October 13, 2017 Aerie Pharmaceuticals, Inc. 1 Introduction Marvin Garrett Vice President, Regulatory Affairs and Quality Assurance Aerie Pharmaceuticals, Inc. 2 Aerie Pharmaceuticals • 2005: Aerie founded as a spin-out from Duke University: – Dr. Eric Toone – Dr. Casey Kopczynski – Dr. David Epstein – Dr. Epstein’s goal from the beginning: Develop a therapy that targeted the diseased tissue in glaucoma, the trabecular outflow pathway • 2006: Aerie discovered its first Rho kinase inhibitor • 2009: Aerie invented netarsudil • 2012: Netarsudil 1st clinical study • 2017: NDA filed 3 Netarsudil: A New Drug Class for Lowering IOP We are requesting a recommendation for approval of netarsudil ophthalmic solution 0.02% for reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension given one drop QD 4 Agenda Unmet Medical Needs Richard A. Lewis, MD Chief Medical Officer Aerie Pharmaceuticals, Inc. Past President, American Glaucoma Society Program Design and Efficacy Casey Kopczynski, PhD Chief Scientific Officer Aerie Pharmaceuticals, Inc. Safety Theresa Heah, MD, MBA VP Clinical Research and Medical Affairs Aerie Pharmaceuticals, Inc. Benefits and Risks Janet Serle, MD Professor of Ophthalmology Glaucoma Fellowship Director Icahn School of Medicine at Mount Sinai 5 List of Expert Responders • Cynthia Mattox, MD – Associate Professor of Ophthalmology, Tufts University School of Medicine – Current President, American Glaucoma Society • Mark Reasor, PhD – Professor of Physiology & Pharmacology, Robert C. Byrd Health Sciences Center, West Virginia University • Bennie H. Jeng, MD – Professor and Chair, Department of Ophthalmology & Visual Sciences, University of Maryland School of Medicine • Dale Usner, PhD – Biostatistics Consultant to Aerie Pharmaceuticals, Inc. -

Looking for New Classes of Bronchodilators
REVIEW BRONCHODILATORS The future of bronchodilation: looking for new classes of bronchodilators Mario Cazzola1, Paola Rogliani 1 and Maria Gabriella Matera2 Affiliations: 1Dept of Experimental Medicine, University of Rome Tor Vergata, Rome, Italy. 2Dept of Experimental Medicine, University of Campania “Luigi Vanvitelli”, Naples, Italy. Correspondence: Mario Cazzola, Dept of Experimental Medicine, University of Rome Tor Vergata, Via Montpellier 1, Rome, 00133, Italy. E-mail: [email protected] @ERSpublications There is a real interest among researchers and the pharmaceutical industry in developing novel bronchodilators. There are several new opportunities; however, they are mostly in a preclinical phase. They could better optimise bronchodilation. http://bit.ly/2lW1q39 Cite this article as: Cazzola M, Rogliani P, Matera MG. The future of bronchodilation: looking for new classes of bronchodilators. Eur Respir Rev 2019; 28: 190095 [https://doi.org/10.1183/16000617.0095-2019]. ABSTRACT Available bronchodilators can satisfy many of the needs of patients suffering from airway disorders, but they often do not relieve symptoms and their long-term use raises safety concerns. Therefore, there is interest in developing new classes that could help to overcome the limits that characterise the existing classes. At least nine potential new classes of bronchodilators have been identified: 1) selective phosphodiesterase inhibitors; 2) bitter-taste receptor agonists; 3) E-prostanoid receptor 4 agonists; 4) Rho kinase inhibitors; 5) calcilytics; 6) agonists of peroxisome proliferator-activated receptor-γ; 7) agonists of relaxin receptor 1; 8) soluble guanylyl cyclase activators; and 9) pepducins. They are under consideration, but they are mostly in a preclinical phase and, consequently, we still do not know which classes will actually be developed for clinical use and whether it will be proven that a possible clinical benefit outweighs the impact of any adverse effect. -

Durysta™ (Bimatoprost Implant, for Intracameral Administration)
Durysta™ (bimatoprost implant, for intracameral administration) When requesting Durysta™ (bimatoprost implant), the individual requiring treatment must be diagnosed with an FDA-approved indication and meet the specific coverage guidelines and applicable safety criteria for the covered indication. FDA-approved Indication Durysta (bimatoprost implant) is indicated for the reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. Coverage Guidelines Reduction of intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension An individual must meet all of the following criteria for authorization: • Is 18 years of age or older; • Is not receiving re-treatment of eye(s) previously treated with Durysta; • Meets the following criteria: o Has experienced inadequate efficacy or severe adverse events to at least two ophthalmic prostaglandins (as monotherapy or concomitant therapy) for the treatment of open-angle glaucoma or ocular hypertension (e.g., bimatoprost ophthalmic solution, latanoprost ophthalmic solution, travoprost ophthalmic solution; latanoprostene bunod ophthalmic solution, and tafluprost ophthalmic solution); AND o Has experienced inadequate efficacy or severe adverse events to at least two ophthalmic products (as monotherapy or concomitant therapy) from two different pharmacologic classes for the treatment of open-angle glaucoma or ocular hypertension (e.g., beta-blockers, alpha-agonist (brimonidine), carbonic anhydrase inhibitors, and rho kinase inhibitor (netarsudil); AND • Durysta is prescribed by or in consultation with an ophthalmologist. Approval duration: 1 dose (one implant per treated eye; a total of two implants per patient) Dosing Recommendation Approve up to one Durysta implant per treated eye(s) [two implants per patient]. References 1. Durysta™ [prescribing information]. Madison, NJ: Allergan USA, Inc; March 2020. -

Commercial/Healthcare Exchange PA Criteria Effective: July 25, 2018
Commercial/Healthcare Exchange PA Criteria Effective: July 25, 2018 Prior Authorization: Rhopressa - Rocklatan Products Affected: Rhopressa (netarsudil) ophthalmic solution, Rocklatan (netarsudil and latanoprost) ophthalmic solution Medication Description: Rhopressa (netarsudil) a Rho kinase (ROCK) inhibitor has been approved by the U.S. Food and Drug Administration in Dcecember 18, 2017 to reduce intraocular pressure (IOP) in patients who have ocular hypertension (OHT) or open-angle glaucoma (OAG). Glaucoma affects approximately 2.3 million people in the United States (US). It is the second most common cause of permanent blindness in the US and the most common cause of blindness among African Americans and Hispanics. Two major types of glaucoma have been identified: open-angle and closed-angle. In OAG, there is reduced flow through the trabecular meshwork. OAG accounts for the majority of cases. OHT can be used as a generic term referring to any situation in which IOP is >21 mmHg, the widely accepted upper limit of normal IOP in the general population. OHT has a 10 to 15 times greater prevalence than primary OAG. A 20% reduction in IOP target in people with OHT has been shown to delay or prevent the onset of glaucoma, but treatment goals should be individualized. Rocklatan (netarsudil/latanoprost) is indicated for the reduction of elevated intraocular pressure (IOP) in patients with open-angle glaucoma or ocular hypertension. In 2 randomized trials, the average intraocular pressure (IOP) lowering effect of netarsudil 0.02%/latanoprost 0.005% was 1 to 3 mmHg greater than monotherapy with either netarsudil 0.02% or latanoprost 0.005%. The American Academy of Ophthalmology (AAO) preferred practice guidelines (2015) for the treatment of glaucoma note that the initial therapy choice, prostaglandin analogues are the most frequently used initial eye drops for lowering IOP in patients with glaucoma. -

Active Moiety Name FDA Established Pharmacologic Class (EPC) Text
FDA Established Pharmacologic Class (EPC) Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: Active Moiety Name “(Drug) is a (FDA EPC Text Phrase) indicated for [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13. -

Therapeutic Class Overview Ophthalmic Agents, Intraocular Pressure (IOP)-Modifying
Therapeutic Class Overview Ophthalmic Agents, Intraocular Pressure (IOP)-Modifying INTRODUCTION Glaucoma is an optic neuropathy that causes gradual degeneration of the cells making up the optic nerve. Glaucoma is among the leading causes of blindness worldwide, and in 2020, an estimated 3.2 million people worldwide are anticipated to be blind due to glaucoma (Flaxman et al 2017). Open-angle glaucoma is the most common form; other forms include angle-closure, congenital, and secondary glaucoma (Jacobs 2018[a]). Patients with open-angle glaucoma initially experience peripheral visual field loss, followed by central field loss, which may progress to irreversible blindness if untreated (Jacobs 2018[a]). The exact etiology of open-angle glaucoma is unknown (Jacobs 2018[a]). Major risk factors for developing open-angle glaucoma include advanced age, African or Hispanic/Latino descent, elevated intraocular pressure (IOP), family history of glaucoma, low ocular perfusion pressure, type 2 diabetes mellitus, and myopia (Ellis et al 2000, Girkin et al 2004, Lesk et al 2007, Prum et al 2016). Elevated IOP is the only major risk factor for glaucoma that is treatable. Available evidence suggests that lowering IOP inhibits or reduces the progression of optic nerve damage (Jacobs 2018[a]). Treatment may be initiated in patients with a raised IOP despite having no visual field loss or optic nerve damage (Jacobs 2018[a]). An IOP > 22 mmHg is generally considered to be elevated and would be treated by most clinicians; however, this number varies according to screening methods, risk factors, and disease progression (Jacobs 2018[a]). The target IOP should be individualized based on response to therapy and disease progression in order to maintain IOP within a range that is unlikely to adversely affect patients’ health-related quality of life (Jacobs 2018[b]). -

Drugs That May Be Used Based on Licensure Designation Page 1 of 7 Updated February 2021 by the Pennsylvania State Board of Optometry
Drugs Which May Be Used Based on Licensure Designation Approved Drugs a.) Administration and prescription of pharmaceutical agents for therapeutic purposes. Optometrists who are certified to prescribe and administer pharmaceutical agents for therapeutic purposes under section 4.1 of the Optometric Practice and Licensure Act (63 P. S. § 244.4a), may prescribe and administer the drugs listed in subsections (c)(1) – (11) below in their practice of optometry. See also 49 Pa. Code § 23.202 for the application procedure for optometrists to administer and prescribe pharmaceutical agents for therapeutic purposes. b.) Administration and prescription of pharmaceutical agents to treat glaucoma. Optometrists who are certified to prescribe and administer pharmaceutical agents to treat glaucoma under section 4.2 of the Optometric Practice and Licensure Act (63 P.S. § 244.4b), may prescribe and administer the drugs listed in subsection (c)(12) below in their practice of optometry. See also 49 Pa. Code § 23.205 for the application procedure for optometrists to administer and prescribe pharmaceutical agents to treat glaucoma. c.) DEA registration reminder. Licensees who hold, or plan to obtain, a DEA registration are reminded to review and comply with PDMP standards. d.) Allowable pharmaceutical products. Optometrists may prescribe and administer the following pharmaceutical products or the A-rated generic therapeutically equivalent drug: (1) Topical Anesthetics (i) benoxinate (ii) lidocaine (iii) proparacaine (iv) tetracaine (2) Topical Ocular Lubricants -

Glaucoma Medications
2/1/2020 Glaucoma Pharmacology: Old, New and What to Do? Joseph Sowka, OD Greg Caldwell, OD Rho-Kinase White 1 2 GLAUCOMA EPIDEMIOLOGY AND AQUEOUS HUMOR DYNAMICS TREATMENT IOP – A Complex Homeostasis Current Medical Treatments for OAG Aqueous formation in ciliary body – passive diffusion, ultrafiltration and active secretion Cornea Aqueous Production Aqueous Outflow Conventional Outflow – Trabecular Meshwork → Schlemm’s Canal → Conventional Unconventional Episcleral Venous System Trabecular Meshwork Prostaglandin Non-Conventional Outflow – Schlemm’s -blocker Cholinergic agonist analog Canal Uveoscleral Episcleral CAI NO-donating PGA NO-donating Veins 2-agonist RhoKinase inhibitor PGA 2-agonist Uveoscleral Outflow Updated 1/7/18 Ciliary Processes 3 4 PROSTAGLANDINS: PROSTAGLANDINS OCULAR ADVERSE EFFECTS ▪ Prostaglandins are not indicated ideal in secondary inflammatory glaucoma or any ▪ Hyperemia clinical entity that has anterior segment ▪ Increased iris coloration inflammation as a component ▪ Periorbitopathy: skin darkening, Sulcus ▪ Prostaglandins are important in that they deepening flatten the diurnal IOP curve as well as giving - Hyperemia is reversible with medication cessation. Iris color lingering IOP reduction even as much as 60 changes appear to be irreversible. Periorbitopathy may be reversible if the medication is stopped soon enough, but may hours after dosing. Thus, they are more indeed be permanent. forgiving of patients that miss dosages. ▪ Hypertrichosis ▪ Punctate keratopathy, dry eye ▪ Uveitis, CME, and dendritic -

A Comprehensive Map of Disease Networks and Molecular Drug Discoveries for Glaucoma Haixin Wang1,2,3, Yanhui Deng1, Ling Wan4 & Lulin Huang1,2,3 ✉
www.nature.com/scientificreports OPEN A comprehensive map of disease networks and molecular drug discoveries for glaucoma Haixin Wang1,2,3, Yanhui Deng1, Ling Wan4 & Lulin Huang1,2,3 ✉ Glaucoma is the leading cause of irreversible blindness worldwide. The molecular etiology of glaucoma is complex and unclear. At present, there are few drugs available for glaucoma treatment. The aim of the present study was to perform a systematic analysis of glaucoma candidate drugs/chemicals based on glaucoma genes, including genetic factors and diferentially expressed (DE) genes. In total, 401 genes from the genetic databases and 1656 genes from the DE gene analysis were included in further analyses. In terms of glaucoma-related genetic factors, 54 pathways were signifcantly enriched (FDR < 0.05), and 96 pathways for DE genes were signifcantly enriched (FDR < 0.05). A search of the PheWAS database for diseases associated with glaucoma-related genes returned 1,289 diseases, and a search for diseases associated with DE glaucoma-related genes returned 1,356 diseases. Cardiovascular diseases, neurodegenerative diseases, cancer, and ophthalmic diseases were highly related to glaucoma genes. A search of the DGIdb, KEGG, and CLUE databases revealed a set of drugs/chemicals targeting glaucoma genes. A subsequent analysis of the electronic medical records (EMRs) of 136,128 patients treated in Sichuan Provincial People’s Hospital for candidate drug usage and the onset of glaucoma revealed nine candidate drugs. Among these drugs, individuals treated with nicardipine had the lowest incidence of glaucoma. Taken together with the information from the drug databases, the 40 most likely candidate drugs for glaucoma treatment were highlighted. -

Rhopressa™ (Netarsudil Ophthalmic Solution) 0.02% Aerie Pharmaceuticals, Inc
Rhopressa™ (netarsudil ophthalmic solution) 0.02% Aerie Pharmaceuticals, Inc. FDA Advisory Committee Briefing Document NDA 208254 Dermatologic and Ophthalmic Drugs Advisory Committee Meeting Briefing Document Product: Rhopressa™ (netarsudil ophthalmic solution) 0.02% NDA Number: 208254 Indication: Reduction of elevated intraocular pressure in patients with open-angle glaucoma or ocular hypertension Sponsor: Aerie Pharmaceuticals, Inc. 2030 Main Street, Suite 1500 Irvine, CA 92614 949-526-8700 Meeting Date: October 13, 2017 ADVISORY COMMITTEE BRIEFING MATERIALS: AVAILABLE FOR PUBLIC RELEASE Page 1 of 93 Rhopressa™ (netarsudil ophthalmic solution) 0.02% Aerie Pharmaceuticals, Inc. FDA Advisory Committee Briefing Document NDA 208254 EXECUTIVE SUMMARY The data presented in this briefing document demonstrate that Rhopressa™ (netarsudil ophthalmic solution) 0.02% is safe and effective for the reduction of elevated intraocular pressure (IOP) in patients with open-angle glaucoma (OAG) or ocular hypertension (OHT). The proposed dosage is 1 drop in the affected eye(s) once daily (QD) in the evening (PM). Background Glaucoma is a leading cause of irreversible blindness that affects more than 60 million people worldwide (Alward 1998, Casson 2012). Glaucoma can arise through various etiologies but vision loss is ultimately due to the progressive death of retinal ganglion cells and related damage to the optic nerve (Vrabec 2007). OAG is the most common form of glaucoma. OAG is defined as the ocular condition where the anterior chamber angle is open upon gonioscopic observation, there is some evidence of optic nerve damage or dysfunction (eg, visual field loss), and patients frequently exhibit elevated IOP. A second disease condition, OHT, has been identified as one for which patients have an elevated IOP compared to population-based cut-off values in the absence of apparent optic nerve damage (Kass 2002).