Fellowships in Family Medicine: Who? What? Where? When? Why?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
COMLEX-USA for Residency Program Directors
COMLEX-USA FOR RESIDENCY PROGRAM DIRECTORS COMLEX-USA Evidence–based assessment designed specifically for osteopathic medical students and residents that measures competencies required for the provision of safe and effective osteopathic medical care to patients. It is recommended but not required that COMLEX-USA Level 3 be taken after a minimum of six months in residency. The attestation process for COMLEX-USA Level 3 helps to fulfill the NBOME mission to DO candidates are not required to pass the United States protect the public, and adds value and entrustability to state licensing Medical Licensing Examination (USMLE®) to be eligible to boards and patients. Additionally, attestation provides COMLEX-USA apply to ACGME-accredited residency programs. The score reports to residency program directors and faculty. ACGME does not specify which licensing board exam(s) (i.e., COMLEX-USA, USMLE) applicants must take to be eligible COMPETENCY AND EVIDENCE-BASED DESIGN for appointment in ACGME-accredited residency programs. In 2019, COMLEX-USA completed a transition to a contemporary, two Frequently Asked Questions: Single Accreditation System decision-point, competency-based exam blueprint and evidence- Accreditation Council for Graduate Medical Education, 20191 based design informed by extensive research on osteopathic physician practice, expert consensus and stakeholder surveys.3 The enhanced COMLEX-USA blueprint4 assesses measurable outcomes PATHWAY TO LICENSURE of seven Fundamental Osteopathic Medical Competency Domains5 COMLEX-USA, the Comprehensive Osteopathic Medical Licensing and focuses on high-frequency, high-impact health issues and clinical Examination of the United States, is the exam series used by all presentations that affect patients. medical licensing authorities to make licensing decisions for osteopathic physicians. -

Required Procedural Training in Family Medicine Residency: a Consensus Statement
248 April 2008 Family Medicine Residency Education Required Procedural Training in Family Medicine Residency: A Consensus Statement Melissa Nothnagle, MD; Julie M. Sicilia, MD; Stuart Forman, MD; Jeremy Fish, MD; William Ellert, MD; Roberta Gebhard, DO; Barbara F. Kelly, MD; John L. Pfenninger, MD; Michael Tuggy, MD; Wm. MacMillan Rodney, MD; STFM Group on Hospital Medicine and Procedural Training Background and Objectives: Specific procedural training standards for US family medicine residen- cies do not exist. As a result, family physicians graduate with highly variable procedural skills, and the scope of procedural practice for family physicians remains poorly defined. Our objective was to develop a standard list of required procedures for family medicine residencies. Methods: The Society of Teachers of Family Medicine Group on Hospital and Procedural Training convened a working group of 17 family physician educators. A multi-voting process was used to define categories and propose a list of required procedures for US family medicine residency programs. Results: The group defined five categories of procedures within the scope of family medicine. Consensus was reached for a core list of procedures that all family medicine residents should be able to perform by the time of graduation. Conclusions: Defining standards for procedural training in family medicine will help clarify family medicine’s scope of practice and should benefit both patients and family physicians. We propose that with input from national family medicine organizations, the procedure list presented in this report be used to develop a national standard for required procedural training. (Fam Med 2008;40(4):248-52.) Controversy exists over which procedures should be requirements for procedure skills to include “a list of taught in family medicine residency. -
AAFP Toolkit: Building and Growing a Sustainable Telehealth Program
A Toolkit for Building and Growing a Sustainable Telehealth Program in Your Practice SEPTEMBER 2020 This toolkit was developed in partnership with Manatt Health. About AAFP The American Academy of Family Physicians (AAFP) is the national association of family physicians. It is one of the largest national medical organizations, with 136,700 members in 50 states, D.C., Puerto Rico, the Virgin Islands and Guam, as well as internationally. We are a membership organization in the purest sense: an association of family physicians led by family physicians. With our colleagues throughout the country, we work to solidify family medicine as the cornerstone of a functioning health care system. We lobby government, negotiate with payers, partner with employers, educate patients, and champion family medicine on the national stage. The AAFP exists to support family physicians so they can spend more time doing what they do best: providing quality, cost-effective patient care. About Manatt Health Manatt Health combines firsthand experience in shaping public policy, sophisticated strategy insight, deep analytic capabilities, and legal excellence to provide uniquely valuable professional services to the full range of health industry stakeholders. Manatt has deep expertise in advising providers, states, payers, and health tech companies on developing, providing, and paying for innovative virtual care solutions. Our diverse team of more than 160 attorneys and consultants from Manatt, Phelps & Phillips, LLP, and its consulting subsidiary, Manatt Health Strategies, LLC, is passionate about helping our clients advance their business interests, fulfill their missions, and lead health care into the future. For more information, visit https://www.manatt.com/Health. -

Curriculum of the Faculty of Family Medicine
CURRICULUM OF THE FACULTY OF FAMILY MEDICINE WEST AFRICAN COLLEGE OF PHYSICIANS TABLE OF CONTENTS Chapter One: Introduction 1.1 Introductory statement 1.2 Needs analysis 1.3 Mission of the Faculty 1.4 Aim and Goals of the Residency Training 1.5 The philosophy. Chapter Two: Pre-Entry (Primary) Syllabus 2.1 Aim of the primary exam 2.2 The Primary syllabus 2.3 The Primary revision course 2.4 The Primary examination Chapter Three: Membership Syllabus 3.1 Goal of the membership training 3.2 Introduction/General structure 3.3 Rotations with durations 3.4 Syllabus for core knowledge 3.5 Syllabus for skills acquisition Chapter Four: Fellowship Syllabus 4.1 Goal of the fellowship training 4.2 Introduction/General structure 4.3 Rotations with durations 4.4 Syllabus for core knowledge 4.5 Syllabus for skills acquisition 4.6 Proposal writing 4.7 Dissertation writing 4.8 Casebook writing Chapter Five: Training institutions and requirements for accreditation 5.1 Accreditation procedure 5.2 Accreditation requirements Chapter Six: Assessments 6.1 Introduction 6.2 Summative Assessments 6.3 Formative Assessments 6.4 Mentorship Appendices CHAPTER ONE – INTRODUCTION 1.1 Introductory statement Family medicine is the medical discipline also known as general practice, general medical practice, family practice, or primary care. It is a discipline which integrates several medical specialties into a new whole. It is concerned with the holistic approach to patient care in which the individual is seen in his totality and in the context of his family and community. The trainees in family medicine should be appropriately equipped to meet the contemporary and future health needs of individuals and families within their practice community. -
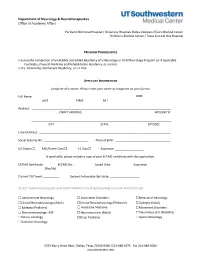
Neurology Fellowship Application
Department of Neurology & Neurotherapeutics Office of Academic Affairs Parkland Memorial Hospital / University Hospitals Dallas Veterans Affairs Medical Center Children's Medical Center / Texas Scottish Rite Hospital PROGRAM PREREQUISITES • Successful completion of an ACGME accredited Residency of a Neurology or Child Neurology Program (or if applicable Psychiatry, Physical Medicine and Rehabilitation Residency, or similar). • U.S. Citizenship, Permanent Residency, or J-1 Visa APPLICANT INFORMATION Complete all sections. Please enter your name as it appears on your license. Full Name: DOB: LAST FIRST M.I. Address: STREET ADDRESS APT/UNIT # ______________________________________________________________________________________ CITY STATE ZIP CODE Email Address: _________________________________________________________________________________ Social Security No.: ___________________________ Place of Birth: __________________________________ US Citizen ☐ EAD/Green Card ☐ J-1 Visa ☐ Expiration __________________ If applicable, please include a copy of your ECFMG certificate with this application. ECFMG Certificate: ________ ECFMG No.: ____________ Issued Date: _____________ Expiration ______________ (Yes/No) Current PGY level: __________ Desired Fellowship start date: __________________ SELECT WHICH NEUROLOGY & NEUROTHERAPEUTICS FELLOWSHIP(S) YOU ARE APPLYING FOR: ☐ Autoimmune Neurology ☐ Autonomic Disorders ☐Behavioral Neurology ☐Clinical Neurophysiology (Adult) ☐Clinical Neurophysiology (Pediatric) ☐ Epilepsy (Adult) ☐ Epilepsy (Pediatric) -

Boston Children's Hospital / Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health
Boston Children’s Hospital/Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health Speaker Alan Woolf, MD, MPH, FAACT, FAAP, FACMT Director, Pediatric Environmental Health Center, Boston Children’s Hospital Director, Region 1 New England PEHSU Director, Fellowship Training Program Professor, Harvard Medical School School Physician Acknowledgments & Disclosures This material was supported by the American Academy of Pediatrics (AAP) and funded (in part) by the cooperative agreement FAIN: 5 NU61TS000237-05 from the Agency for Toxic Substances and Disease Registry (ATSDR). Funding for this seminar was made possible (in part) by the cooperative agreement award number 1U61TS000237- 05 from the Agency for Toxic Substances and Disease Registry (ATSDR). The views expressed in written materials and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services. •The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government •Neither EPA nor ATSDR endorse the purchase of any commercial products or services mentioned in PEHSU publications. •In the past 12 months, we have had no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider(s) of commercial services discussed -
Medical Scientist Training Program
The University of Michigan MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines A Handbook for Fellows https://www.medicine.umich.edu/medschool/education/md-phd- program/current students/ August 2018 CONTENTS 1. MSTP Office 2. Communication 3. Academic Advising 4. I.D. and Computer Access 5. Course of Study 6. Biological Chemistry Requirement 7. Medical School Registration 8. Medical and Graduate School Grading Systems 9. Graduate School Registration 10. Research Rotations 11. Selecting a Doctoral Field and the Thesis Research Mentor 12. Graduate School Residency Requirements 13. Research Responsibility and Ethics Requirements 14. Research Phase: External Funding Sources 15. Advancement to Candidacy 16. Precandidate Year to Candidacy Transition: Funding and Insurance Issues 17. Research Phase to M3 Transition 18. M4 Year 19. Transition to Post Graduate Training, Residency 20. Dean’s Letters 21. Simultaneous Awarding of Dual Degrees 22. United States Medical Licensure Examination Step 1 and Step 2 (Clinical Knowledge and Clinical Skills) 23. Rackham Graduate School Policies 24. Medical School Policies and Procedures 25. The Fellowship Award and the Stipend Level 26. Monthly Stipend Check 27. Taxability of NRSA Stipends 28. NIH Funding Trainee Appointment Forms and Trainee Termination Notice Forms 29. Tuition Payment, Billing Procedures, and Registration 30. Travel Funds and Expense Forms 31. Health Care Insurance 32. Health Service 33. CV and Publication File 34. Individual Development Pan (IDP) 35. Vacations and Other Absences 36. MSTP Scientific Retreat 37. MSTP Seminars 38. Citizenship 39. MSTP Committees: Operating Committee (OC) and Program Activities Committee (PAC) A Handbook for MSTP Fellows MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines for Fellows 1. -

Primer for Applying to Internal Medicine Residency Programs A
Primer for Applying to Internal Medicine Residency Programs A) Fourth-Year Schedule: • Ideally, schedule the internal medicine sub-internship during July or August in order to procure a letter of recommendation (if needed). • Alternative clinical experiences to consider in place of the sub-internship include: o Away rotations: ▪ Away rotations are NOT required for IM. The majority of students applying to IM across the country do not partake in visiting rotations. Visiting rotations are most helpful if students demonstrate a significant interest in a particular program or location. ▪ Away rotations may increase the chance of an invitation to interview at the hosting institution, but this is NOT guaranteed. ▪ Visiting subspecialty electives are preferred over visiting sub- internships, which require strong institutional systems knowledge to optimize clinical performance. o Critical Care Clerkship o Subspecialty Rotations at Cooper • IM residency interviews often start in mid-October and extend to the end of January with the majority of interviews occurring in November and December. Therefore, plan accordingly. • Schedule a more rigorous clinical experience in the spring to enhance clinical skills prior to graduation in preparation for residency. B) Timeline: C) Curriculum Vitae & ERAS Application: • Timeline: Should include all longitudinal, meaningful experiences from the first day of college until present day. • Experience Boxes: o Research Experience: ▪ Include all meaningful research at both the undergraduate and medical school level -
SAP Crystal Reports
Results of the 2016 NRMP Program Director Survey Specialties Matching Service October 2016 www.nrmp.org Requests for permission to use these data as well as questions about the content of this publication or the National Resident Matching Program data and reports may be directed to Mei Liang, Director of Research, NRMP, at [email protected]. Questions about the NRMP should be directed to Mona M. Signer, President and CEO, NRMP, at [email protected]. Suggested Citation National Resident Matching Program, Data Release and Research Committee: Results of the 2016 NRMP Program Director Survey, Specialties Matching Service. National Resident Matching Program, Washington, DC. 2016. Copyright © 2016 National Resident Matching Program. All rights reserved. Permission to use, copy and/or distribute any documentation and/or related images from this publication shall be expressly obtained from the NRMP. Table of Contents Introduction .................................................................................................................................................... 1 Response rates ................................................................................................................................................. 2 All Specialties................................................................................................................................................. 3 Charts for Individual Specialties Abdominal Transplant Surgery .................................................................................................................... -

Ophthalmology Lecture 2: Red Eye for the Family Physician
University of Massachusetts Medical School eScholarship@UMMS PEER Liberia Project UMass Medical School Collaborations in Liberia 2020-06-08 Ophthalmology Lecture 2: Red Eye for the Family Physician Louis Oteng-Gyimah Sunyani SDA Hospital Let us know how access to this document benefits ou.y Follow this and additional works at: https://escholarship.umassmed.edu/liberia_peer Part of the Eye Diseases Commons, Family Medicine Commons, Medical Education Commons, and the Ophthalmology Commons Repository Citation Oteng-Gyimah L. (2020). Ophthalmology Lecture 2: Red Eye for the Family Physician. PEER Liberia Project. https://doi.org/10.13028/z1ka-g173. Retrieved from https://escholarship.umassmed.edu/ liberia_peer/41 This material is brought to you by eScholarship@UMMS. It has been accepted for inclusion in PEER Liberia Project by an authorized administrator of eScholarship@UMMS. For more information, please contact [email protected]. RED EYE FOR THE FAMILY PHYSICIAN ELWA Family Medicine Residency Program LOUIS OTENG-GYIMAH, MBChB, MGCS OPHTHALMOLOGIST @ SUNYANI SDA HOSPITAL BONO REGION, GHANA INTRODUCTION For the primary care physician, the occurrence of a red eye is a frequent and prominent finding of a disease process in patients. A careful history and simple examination with the observation of typical clinical signs are important for the management of this common disorder. The causes can be classified as painful red eye, trauma, and other common conditions. The most frequent causes of a red eye, such as dry eye, conjunctivitis, keratitis, iritis, acute glaucoma, subconjunctival hematoma, foreign bodies, corneal abrasion, and blunt or penetrating trauma Often benign and self-limiting, some diseases associated with a red eye can nevertheless threaten eyesight or even life. -

Annex 1 ; 20 Definitions Analyzed in GP/FM and PHC
Annex 1 ; supplement to ; Marc Jamoulle, Melissa Resnick, Robert Vander Stichele, Ashwin Ittoo, Elena Cardillo, Marc Vanmeerbeek. Analysis of definitions of General Practice/Family Medicine and Primary Health Care (accepted for publication BJGP Open 2017) Annex 1 ; 20 Definitions analyzed in GP/FM and PHC Ten General Practice / Family Medicine Ten Primary Health Care (GP/FM) definitions (PHC) definitions • Leeuwenhorst definition (1974)(1) • Institute of Medicine (1996) (2) • American association of Family Physicians Primary • PAHO (4)Primary Health Care statement (2007) Care Physician definition( 1977)(3) (4) • American association of Family Physicians Family • EU Expert panel definition of primary care medicine definition (1984) (5) (2014) (6) • F. Olesen Proposal for a new definition of General • Brazil organization of Primary Health Care practice (2000) (7) (2013) (8) • WONCA dictionary ( 2003) (9) • World Health Organization Glossary (2016) (10) • WONCA Europe definition Euract (2011) (11) • PHC-RIS Australia (2015)(12) • The CIMF Carta de Quito definition (Latin América) • The Belgian Medical Home (FMMCSF) (2014) (13) (2016)(14) • The Role Definition Group definition (USA)(2014) (15) • The Primary care medical home (AHRQ)(2016)(16) • National Board of Examination India definition (NBE • The French Medical Home (FFMPS) (2016) (18) India) (2015) (17) • AAFP Primary Care Physician (2016)(3) • AAFP Primary Care (2016)(3) Table 1 Sources of the two set definitions of definitions for General Practice/Family Medicine and Primary HealthCare List of ten definitions about General Practice/ Family Medicine 1. Leeuwenhorst definition general practitioner 1974 (1) The general practitioner is a licensed medical graduate who gives personal, primary and continuing care to individuals, families and a practice population, irrespective of age, sex and illness. -
Introductory Ophthalmology for Internists
Common Eye Conditions Every Primary Care Clinician Should Know Cynthia S. Chiu, MD, FACS Associate Professor UCSF Department of Ophthalmology UCSF Family Medicine Board Review March 9, 2016 http://www.timandjeni.com/images/cookiemonster.jpg Disclosure I have no financial interest in any of the products mentioned in this presentation The Eye Exam Eye Vital Sign Near Vision Card Held at 14 inches Glasses as needed http://www.drbanker.com/images/Nearvision.gif Pupils Look for afferent pupillary defect Swinging flashlight test +APD indicates optic nerve or large retinal lesion http://img.tfd.com/ElMill/thumb/F0P-24-S2958.jpg Motility Six extraocular muscles Test cardinal fields of gaze http://www.opsweb.org/OpPhoto/Extern/Motility/muscle.jpg http://www.opsweb.org/OpPhoto/Extern/Motility/9gazedwg.jpg Confrontational Visual Fields Cover eyes on same side Hold fingers midway between Normal per eye: 60-60-60-90 http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=cm&part=A3460&rendertype=figure&id=A3464 Penlight Exam Lids Lashes Conjunctiva/Sclera Cornea Iris/Pupil Puncta Lens http://cache.heraldinteractive.com/blogs/sports/rap_sheet/wp-content/uploads/2009/11/bionic-eye.jpg Anterior Chamber Depth Deep chamber: illumination of nasal iris Shallow chamber: shadow on nasal iris Dilation: Phenylephrine 2.5%, Tropicamide 1% http://iei.ico.edu/images/anatomy.jpg http://www.ophthobook.com/wp-content/uploads/2007/12/video-glaucoma-shallowpenlight.jpg Fundoscopy PanOptic or Direct Ophthalmoscope Evaluate optic nerve, retinal vessels, macula