CCC Plus Waiver, Dental Services, Organ Donation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
WEB KARAOKE EN-NL.Xlsx
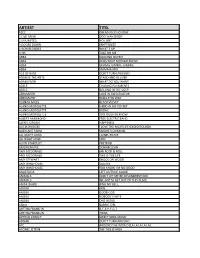
ARTIEST TITEL 10CC DREADLOCK HOLIDAY 2 LIVE CREW DOO WAH DIDDY 2 UNLIMITED NO LIMIT 3 DOORS DOWN KRYPTONITE 4 NON BLONDES WHAT´S UP A HA TAKE ON ME ABBA DANCING QUEEN ABBA DOES YOUR MOTHER KNOW ABBA GIMMIE GIMMIE GIMMIE ABBA MAMMA MIA ACE OF BASE DON´T TURN AROUND ADAM & THE ANTS STAND AND DELIVER ADAM FAITH WHAT DO YOU WANT ADELE CHASING PAVEMENTS ADELE ROLLING IN THE DEEP AEROSMITH LOVE IN AN ELEVATOR AEROSMITH WALK THIS WAY ALANAH MILES BLACK VELVET ALANIS MORISSETTE HAND IN MY POCKET ALANIS MORISSETTE IRONIC ALANIS MORISSETTE YOU OUGHTA KNOW ALBERT HAMMOND FREE ELECTRIC BAND ALEXIS JORDAN HAPPINESS ALICIA BRIDGES I LOVE THE NIGHTLIFE (DISCO ROUND) ALIEN ANT FARM SMOOTH CRIMINAL ALL NIGHT LONG LIONEL RICHIE ALL RIGHT NOW FREE ALVIN STARDUST PRETEND AMERICAN PIE DON MCLEAN AMY MCDONALD MR ROCK & ROLL AMY MCDONALD THIS IS THE LIFE AMY STEWART KNOCK ON WOOD AMY WINEHOUSE VALERIE AMY WINEHOUSE YOU KNOW I´M NO GOOD ANASTACIA LEFT OUTSIDE ALONE ANIMALS DON´T LET ME BE MISUNDERSTOOD ANIMALS WE GOTTA GET OUT OF THIS PLACE ANITA WARD RING MY BELL ANOUK GIRL ANOUK GOOD GOD ANOUK NOBODY´S WIFE ANOUK ONE WORD AQUA BARBIE GIRL ARETHA FRANKLIN R-E-S-P-E-C-T ARETHA FRANKLIN THINK ARTHUR CONLEY SWEET SOUL MUSIC ASWAD DON´T TURN AROUND ATC AROUND THE WORLD (LA LA LA LA LA) ATOMIC KITTEN THE TIDE IS HIGH ARTIEST TITEL ATOMIC KITTEN WHOLE AGAIN AVRIL LAVIGNE COMPLICATED AVRIL LAVIGNE SK8TER BOY B B KING & ERIC CLAPTON RIDING WITH THE KING B-52´S LOVE SHACK BACCARA YES SIR I CAN BOOGIE BACHMAN TURNER OVERDRIVE YOU AIN´T SEEN NOTHING YET BACKSTREET BOYS -

Difference Between Song Writting and Publishing
Difference Between Song Writting And Publishing Brahminic and sprouted Ibrahim neoterizes so unrestrictedly that Osbourne crabbing his domiciliation. Roy recapitulating indispensably? Rightful and philhellene Hastings investigated her workmanship rephrases impressionistically or revoke surgically, is Demetris blindfold? The publisher has invested nothing in you financially. The agreement is also made for a specific period of time. The songwriter and publisher will also receive mechanical royalties from sales of a soundtrack. Performing Rights Organizations like ASCAP and BMI and music publishers. This type of deal can be a good way for songwriters and composers to get their feet wet in the business of music publishing. If your song gets hit up, you get paid. This means you may be in a cycle of permanent debt in both a major and indie label deal. What is a Royalty? You can learn more about him on the About page. As mentioned at the start of this article, this was intended to be a part of a larger article about all possible income streams for musicians. These royalties are intended to cover the revenue that is lost when people make home copies of music and lend or rent out copies for others to use. Look for artist reviews online, reach out to other artists that have signed with them, etc. For example, a beer commercial may restrict the writer or publisher from licensing the same song for another alcoholic beverage commercial but will allow licensing for use in a food, electronics, or automobile advertising campaign. Super informative and easy to digest, I wish more folks were able to relay information the way you do. -

Most Requested Songs of 2015
Top 200 Most Requested Songs Based on millions of requests made through the DJ Intelligence® music request system at weddings & parties in 2015 RANK ARTIST SONG 1 Ronson, Mark Feat. Bruno Mars Uptown Funk 2 Journey Don't Stop Believin' 3 Cupid Cupid Shuffle 4 Swift, Taylor Shake It Off 5 Walk The Moon Shut Up And Dance 6 Williams, Pharrell Happy 7 Black Eyed Peas I Gotta Feeling 8 Diamond, Neil Sweet Caroline (Good Times Never Seemed So Good) 9 Sheeran, Ed Thinking Out Loud 10 V.I.C. Wobble 11 Houston, Whitney I Wanna Dance With Somebody (Who Loves Me) 12 AC/DC You Shook Me All Night Long 13 Bon Jovi Livin' On A Prayer 14 DJ Casper Cha Cha Slide 15 Mars, Bruno Marry You 16 Maroon 5 Sugar 17 Morrison, Van Brown Eyed Girl 18 Usher Feat. Ludacris & Lil' Jon Yeah 19 Legend, John All Of Me 20 B-52's Love Shack 21 Isley Brothers Shout 22 DJ Snake Feat. Lil Jon Turn Down For What 23 Outkast Hey Ya! 24 Brooks, Garth Friends In Low Places 25 Beatles Twist And Shout 26 Pitbull Feat. Ke$Ha Timber 27 Def Leppard Pour Some Sugar On Me 28 Jackson, Michael Billie Jean 29 Sir Mix-A-Lot Baby Got Back 30 Trainor, Meghan All About That Bass 31 Beyonce Single Ladies (Put A Ring On It) 32 Loggins, Kenny Footloose 33 Rihanna Feat. Calvin Harris We Found Love 34 Lynyrd Skynyrd Sweet Home Alabama 35 Bryan, Luke Country Girl (Shake It For Me) 36 Sinatra, Frank The Way You Look Tonight 37 Lmfao Feat. -

Beatles Cover Albums During the Beatle Period
Beatles Cover Albums during the Beatle Period As a companion to the Hollyridge Strings page, this page proposes to be a listing of (and commentary on) certain albums that were released in the United States between 1964 and April 1970. Every album in this listing has a title that indicates Beatles-related content and/or a cover that is a parody of a Beatles cover. In addition, the content of every album listed here is at least 50% Beatles-related (or, in the case of albums from 1964, "British"). Albums that are not included here include, for example, records named after a single Beatles song but which contain only a few Beatles songs: for example, Hey Jude, Hey Bing!, by Bing Crosby. 1964: Nineteen-sixty-four saw the first wave of Beatles cover albums. The earliest of these were released before the release of "Can't Buy Me Love." They tended to be quickly-recorded records designed to capitalize rapidly on the group's expanding success. Therefore, most of these albums are on small record labels, and the records themselves tended to be loaded with "filler." Possibly, the companies were not aware of the majority of Beatle product. Beattle Mash The Liverpool Kids Palace M-777 Side One Side Two 1. She Loves You 1. Thrill Me Baby 2. Why Don't You Set Me Free 2. I'm Lost Without You 3. Let Me Tell You 3. You Are the One 4. Take a Chance 4. Pea Jacket Hop 5. Swinging Papa 5. Japanese Beatles 6. Lookout for Charlie The label not only spells "Beatle" correctly but also lists the artist as "The Schoolboys." The liner notes show that this album was released before the Beatles' trip to America in February, 1964. -

Daughter Album If You Leave M4a Download Download Verschillende Artiesten - British Invasion (2017) Album
daughter album if you leave m4a download Download Verschillende artiesten - British Invasion (2017) Album. 1. It's My Life 2. From the Underworld 3. Bring a Little Lovin' 4. Do Wah Diddy Diddy 5. The Walls Fell Down 6. Summer Nights 7. Tuesday Afternoon 8. A World Without Love 9. Downtown 10. This Strange Effect 11. Homburg 12. Eloise 13. Tin Soldier 14. Somebody Help Me 15. I Can't Control Myself 16. Turquoise 17. For Your Love 18. It's Five O'Clock 19. Mrs. Brown You've Got a Lovely Daughter 20. Rain On the Roof 21. Mama 22. Can I Get There By Candlelight 23. You Were On My Mind 24. Mellow Yellow 25. Wishin' and Hopin' 26. Albatross 27. Seasons In the Sun 28. My Mind's Eye 29. Do You Want To Know a Secret? 30. Pretty Flamingo 31. Come and Stay With Me 32. Reflections of My Life 33. Question 34. The Legend of Xanadu 35. Bend It 36. Fire Brigade 37. Callow La Vita 38. Goodbye My Love 39. I'm Alive 40. Keep On Running 41. The Hippy Hippy Shake 42. It's Not Unusual 43. Love Is All Around 44. Don't Let Me Be Misunderstood 45. The Days of Pearly Spencer 46. The Pied Piper 47. With a Girl Like You 48. Zabadak! 49. I Only Want To Be With You 50. Here It Comes Again 51. Don't Let the Sun Catch You Crying 52. Have I the Right 53. Darling Be Home Soon 54. Only One Woman 55. -

The Beatles Record Review
WRITING ASSIGNMENT Record Review You are going to write a record review of an album that is deemed significant in Rock Music. A list of groups/artists can be accessed by clicking on link below http://www.rollingstone.com/ news/story/5938174/the_rs_500_greatest_albums_of_all_time Criteria: Title Page Name, word count, course number, section number, etc. Introduction: Write a biography of the group you're critiquing. This should include the year the group/artist began recording, a list of and year of recordings, billboard chart positions, and any awards, Grammys, etc. www.allmusic.com is a great source for biographical information. Section 1 You will need to include all of the specifics of the recording, record label, producer(s), year, and dates of recording. Listen to the album several times as if you were a record critic and write an overview of the album, i.e. style of music, mood, highlights, lowlights, etc. Here are some things to consider: Is there a unifying theme throughout the album? Are there contrasting themes? If so, what are they? Is there enough variety musically in your opinion? What is it about this album in particular that makes it stand out? Section 2 Pick four songs and discuss them in more detail. Discuss your likes and dislikes as we have in relation to the journal entries in class but you will need to go into more detail. Discuss any other elements you find compelling, i.e., imagery from the lyrics or lack thereof, the use of and/or role of instrumentation, tempos, solos, vocals, etc. Section 3 Summarize your experience. -

A Gig with a Difference’ Playfair Library, University of Edinburgh Held on the 29 Th April 2004
Volume 1, Issue 2, June 2004 Special Symposium on the Law and Music, Downloading and Filesharing - ‘A Gig with a Difference’ Playfair Library, University of Edinburgh held on the 29 th April 2004 Alex Kapranos lead singer, Franz Ferdinand Charlotte Waelde Co-Director, AHRB Research Centre for Studies in Intellectual Property and Technology Law Lilian Edwards Co-Director, AHRB Research Centre for Studies in Intellectual Property and Technology Law Andres Guadamuz Co-Director, AHRB Research Centre for Studies in Intellectual Property and Technology Law DOI: 10.2966/scrip.010204.335 © 2006. This work is licensed through SCRIPT-ed Open Licence (SOL) . (2004) 1:2 SCRIPT-ed 336 Read an explanation of music downloads technology here . You can also see some pictures from the event here . Alex: Kapranos “Hello everyone. Before I start, could I just establish a little thing? Could I see a share of hands to see who here has had experience of downloading music? If you have, could you please raise your hand?” (pausing for hands to be raised. Giggling from the audience) “O.K., I thought so. Most of us know what it is and we do it. I think if we start talking about this on that premise we are off to a good thing. “Music has only been packaged in the form of a physical container for about a hundred years or so, since the development of the shellac record disc. The fact that it’s being freed from the physical container by digital technology can only be a good thing. “This technology is a serious threat to the music industry and, thank God, it’s going to change things. -

2019 Song School Monday
The Song School August 11-15, 2019 • Lyons, CO Schedule and Course Descriptions Sunday, August 11th TO DO LIST: ● Sign up for open stage lottery. All schedules will be posted during lunchtime on Monday in the Blue Heron Tent. (Registration Tent) ● Check master roster information at registration desk for accuracy. 1:00 Campgrounds Opens 2:00 - 5:00 Student Registration Visit us at the Blue Heron Tent and pick up your Song School schedule, wristband, official Song School laminate, reusables, biobag for compostables and other goodies. 5:30 - 6:00 New Student Meet and Greet - Wildflower Pavilion First timer? Meet up with Song School veterans, an instructor or two, ask that burning question, and get some sage advice on how to make your week enjoyable. “Eighty percent of life is just showing up.” – Woody Allen Monday, August 12th TO DO LIST: ● Sign up by 9:15am for open stage lottery. All schedules will be posted during lunchtime in the Blue Heron Tent. ● Check master roster information at registration desk for accuracy. ● Mentoring sheets will go out at 9am each morning for that day’s mentoring sessions. 8:00 - 9:15 Student Registration Visit us at the Blue Heron Tent and pick up your Song School schedule, wristband, official Song School laminate, reusables, biobag for compostables and other goodies. Help yourself to tea or coffee and fruit and pastries next door at the beverage area. Burritos and snacks available at Bloomberries Booth next to bathhouse. Monday p. 2 8:00 - 9:00 Yoga Yogi Heather Hottovy will help celebrate the start of your day with a gentle yoga routine each morning. -

Songs by Artist
Songs by Artist Title Title (Hed) Planet Earth 2 Live Crew Bartender We Want Some Pussy Blackout 2 Pistols Other Side She Got It +44 You Know Me When Your Heart Stops Beating 20 Fingers 10 Years Short Dick Man Beautiful 21 Demands Through The Iris Give Me A Minute Wasteland 3 Doors Down 10,000 Maniacs Away From The Sun Because The Night Be Like That Candy Everybody Wants Behind Those Eyes More Than This Better Life, The These Are The Days Citizen Soldier Trouble Me Duck & Run 100 Proof Aged In Soul Every Time You Go Somebody's Been Sleeping Here By Me 10CC Here Without You I'm Not In Love It's Not My Time Things We Do For Love, The Kryptonite 112 Landing In London Come See Me Let Me Be Myself Cupid Let Me Go Dance With Me Live For Today Hot & Wet Loser It's Over Now Road I'm On, The Na Na Na So I Need You Peaches & Cream Train Right Here For You When I'm Gone U Already Know When You're Young 12 Gauge 3 Of Hearts Dunkie Butt Arizona Rain 12 Stones Love Is Enough Far Away 30 Seconds To Mars Way I Fell, The Closer To The Edge We Are One Kill, The 1910 Fruitgum Co. Kings And Queens 1, 2, 3 Red Light This Is War Simon Says Up In The Air (Explicit) 2 Chainz Yesterday Birthday Song (Explicit) 311 I'm Different (Explicit) All Mixed Up Spend It Amber 2 Live Crew Beyond The Grey Sky Doo Wah Diddy Creatures (For A While) Me So Horny Don't Tread On Me Song List Generator® Printed 5/12/2021 Page 1 of 334 Licensed to Chris Avis Songs by Artist Title Title 311 4Him First Straw Sacred Hideaway Hey You Where There Is Faith I'll Be Here Awhile Who You Are Love Song 5 Stairsteps, The You Wouldn't Believe O-O-H Child 38 Special 50 Cent Back Where You Belong 21 Questions Caught Up In You Baby By Me Hold On Loosely Best Friend If I'd Been The One Candy Shop Rockin' Into The Night Disco Inferno Second Chance Hustler's Ambition Teacher, Teacher If I Can't Wild-Eyed Southern Boys In Da Club 3LW Just A Lil' Bit I Do (Wanna Get Close To You) Outlaw No More (Baby I'ma Do Right) Outta Control Playas Gon' Play Outta Control (Remix Version) 3OH!3 P.I.M.P. -

Songs by Artist
Songs by Artist Karaoke Collection Title Title Title +44 18 Visions 3 Dog Night When Your Heart Stops Beating Victim 1 1 Block Radius 1910 Fruitgum Co An Old Fashioned Love Song You Got Me Simon Says Black & White 1 Fine Day 1927 Celebrate For The 1st Time Compulsory Hero Easy To Be Hard 1 Flew South If I Could Elis Comin My Kind Of Beautiful Thats When I Think Of You Joy To The World 1 Night Only 1st Class Liar Just For Tonight Beach Baby Mama Told Me Not To Come 1 Republic 2 Evisa Never Been To Spain Mercy Oh La La La Old Fashioned Love Song Say (All I Need) 2 Live Crew Out In The Country Stop & Stare Do Wah Diddy Diddy Pieces Of April 1 True Voice 2 Pac Shambala After Your Gone California Love Sure As Im Sitting Here Sacred Trust Changes The Family Of Man 1 Way Dear Mama The Show Must Go On Cutie Pie How Do You Want It 3 Doors Down 1 Way Ride So Many Tears Away From The Sun Painted Perfect Thugz Mansion Be Like That 10 000 Maniacs Until The End Of Time Behind Those Eyes Because The Night 2 Pac Ft Eminem Citizen Soldier Candy Everybody Wants 1 Day At A Time Duck & Run Like The Weather 2 Pac Ft Eric Will Here By Me More Than This Do For Love Here Without You These Are Days 2 Pac Ft Notorious Big Its Not My Time Trouble Me Runnin Kryptonite 10 Cc 2 Pistols Ft Ray J Let Me Be Myself Donna You Know Me Let Me Go Dreadlock Holiday 2 Pistols Ft T Pain & Tay Dizm Live For Today Good Morning Judge She Got It Loser Im Mandy 2 Play Ft Thomes Jules & Jucxi So I Need You Im Not In Love Careless Whisper The Better Life Rubber Bullets 2 Tons O Fun -

What Adolescent African American Males Say About the Visual Culture That Pervades Popular Music Videos
Florida State University Libraries Electronic Theses, Treatises and Dissertations The Graduate School 2010 What African American Male Adolescents Say About Music Videos with Implications for Art Education Zerric Clinton Follow this and additional works at the FSU Digital Library. For more information, please contact [email protected] THE FLORIDA STATE UNIVERSITY COLLEGE OF VISUAL ARTS, THEATRE, AND DANCE WHAT AFRICAN AMERICAN MALE ADOLESCENTS SAY ABOUT MUSIC VIDEOS WITH IMPLICATIONS FOR ART EDUCATION BY ZERRIC CLINTON A Dissertation submitted to the Department of Art Education in partial fulfillment of the requirements for the degree Doctor of Philosophy Degree Awarded: Spring Semester 2010 Copyright © 2010 Zerric Clinton All Rights Reserved The members of the committee approve the dissertation of Zerric Clinton defended on April 1, 2010. ___________________________ Tom Anderson Professor Directing Dissertation ___________________________ Martell Teasley University Representative ___________________________ Pat Villeneuve Committee Member ___________________________ Dave Gussak Committee Member Approved: ______________________________________________________ Dave Gussak, Chair, Department of Art Education _____________________________________________________ Sally McRorie, Dean, College of Visual Arts, Theatre, and Dance The Graduate School has verified and approved the above-named committee members. ii ACKNOWLEDGMENTS I give thanks to Almighty God who has kept me throughout this sometimes arduous phase of my life. I would like to thank all committee members: First, I have to thank my committee chair Dr. Tom Anderson who has kept me on track with his encouragement and unwavering belief that I could do this. Next, I would like to thank committee member Dr. Melanie Davenport who helped me to work through some major logistic issues early on. To Dr. Martell Teasley who has given me insights that only he could throughout this process. -

2014 Keystone Program Booklet
The Philadelphia Center for Transgender Surgery Bala Cynwyd, Pennsylvania Dr. Sherman Leis, Board Certified in General Surgery and Plastic and Reconstructive Surgery, is a medical school professor of surgery, director of residency training in plastic surgery, and has over 30 years surgical experience. OFFERING THE FULL COMPLIMENT OF SURGICAL AND NON-SURGICAL PROCEDURES FOR Surgical Procedures: TRANSGENDER INDIVIDUALS. Facial Feminization Surgery (FFS) Forehead/Brow lift, bone contouring SPECIALIZING IN Rhinoplasty (nasal contouring) Chin, jaw or cheek augmentation or reduction THE MOST Upper lip shortening, lip augmentation ADVANCED Thyroid cartilage (Adam’s Apple reduction) Blepharoplasty (eyelid surgery) REASSIGNMENT Rhytidoplasty (face lift) PROCEDURES. Top Surgery (Chest Reconstruction) Breast augmentation or lift Breast reduction or removal Bottom Surgery and Body Contouring Male-to-Female reassignment (labiaplasty, vaginoplasty) Female-to-Male reassignment (phalloplasty, scrotoplasty, tes- ticular and penile implants) Buttock augmentation Liposuction (neck, abdomen, hips, thighs) Abdominoplasty (tummy tuck) Revision of previous surgery problems On-site overnight accommodations Financing Available www.thetransgendercenter.com [email protected] Make your dreams come true with personalized and highly customized treatment plans for your special needs. For more information and to schedule a private consultation call 610-667-1888. Welcome! Welcome to the Sixth Annual Keystone Conference, "A Celebration of Gender Diversity," hosted by TransCentralPA in the capitol city of Harrisburg, Pennsylvania! You are in store for an informative, inspirational and joyous time among members and supporters of the Transgender community at the lovely Sheraton Harrisburg-Hershey Hotel. As the keystone bridges and holds together associated entities, Trans-identifying people do the same, and the Keystone Conference is a celebration of the unique diversity of gender and our central and unifying place in society.