Epidermoid Cyst
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

Oral Diagnosis: the Clinician's Guide
Wright An imprint of Elsevier Science Limited Robert Stevenson House, 1-3 Baxter's Place, Leith Walk, Edinburgh EH I 3AF First published :WOO Reprinted 2002. 238 7X69. fax: (+ 1) 215 238 2239, e-mail: [email protected]. You may also complete your request on-line via the Elsevier Science homepage (http://www.elsevier.com). by selecting'Customer Support' and then 'Obtaining Permissions·. British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Library of Congress Cataloging in Publication Data A catalog record for this book is available from the Library of Congress ISBN 0 7236 1040 I _ your source for books. journals and multimedia in the health sciences www.elsevierhealth.com Composition by Scribe Design, Gillingham, Kent Printed and bound in China Contents Preface vii Acknowledgements ix 1 The challenge of diagnosis 1 2 The history 4 3 Examination 11 4 Diagnostic tests 33 5 Pain of dental origin 71 6 Pain of non-dental origin 99 7 Trauma 124 8 Infection 140 9 Cysts 160 10 Ulcers 185 11 White patches 210 12 Bumps, lumps and swellings 226 13 Oral changes in systemic disease 263 14 Oral consequences of medication 290 Index 299 Preface The foundation of any form of successful treatment is accurate diagnosis. Though scientifically based, dentistry is also an art. This is evident in the provision of operative dental care and also in the diagnosis of oral and dental diseases. While diagnostic skills will be developed and enhanced by experience, it is essential that every prospective dentist is taught how to develop a structured and comprehensive approach to oral diagnosis. -

WHAT HAPPENED? CDR, a 24-Year-Old Chinese Male
CHILDHOOD DEVELOPMENTAL SCREENING 2020 https://doi.org/10.33591/sfp.46.5.up1 FINDING A MASS WITHIN THE ORAL CAVITY: WHAT ARE THE COMMON CAUSES AND 4-7 GAINING INSIGHT: WHAT ARE THE ISSUES? In Figure 2 below, a list of masses that could arise from each site Figure 3. Most common oral masses What are the common salivary gland pathologies Salivary gland tumours (Figure 7) commonly present as channel referrals to appropriate specialists who are better HOW SHOULD A GP MANAGE THEM? of the oral cavity is given and elaborated briey. Among the that a GP should be aware of? painless growing masses which are usually benign. ey can equipped in centres to accurately diagnose and treat these Mr Tan Tai Joum, Dr Marie Stella P Cruz CDR had a slow-growing mass in the oral cavity over one year more common oral masses are: torus palatinus, torus occur in both major and minor salivary glands but are most patients, which usually involves surgical excision. but sought treatment only when he experienced a sudden acute mandibularis, pyogenic granuloma, mucocele, broma, ere are three pairs of major salivary glands (parotid, commonly found occurring in the parotid glands. e most 3) Salivary gland pathology may be primary or secondary to submandibular and sublingual) as well as hundreds of minor ABSTRACT onset of severe pain and numbness. He was fortunate to have leukoplakia and squamous cell carcinoma – photographs of common type of salivary gland tumour is the pleomorphic systemic causes. ese dierent diseases may present with not sought treatment as it had not caused any pain. -
Mandibular Tori
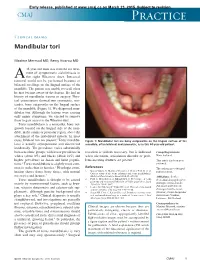
Early release, published at www.cmaj.ca on March 23, 2015. Subject to revision. CMAJ Practice Clinical images Mandibular tori Maxime Mermod MD, Remy Hoarau MD 44-year-old man was referred for treat- ment of symptomatic sialolithiasis in A the right Wharton duct. Intraoral removal could not be performed because of bilateral swellings on the lingual surface of the mandible. The patient was unable to recall when he first became aware of the lesions. He had no history of mandibular trauma or surgery. Phys- ical examination showed two symmetric, non- tender, bony outgrowths on the lingual surface of the mandible (Figure 1). We diagnosed man- dibular tori. Although the lesions were causing only minor symptoms, we elected to remove them to gain access to the Wharton duct. Torus mandibularis is a nontender, bony out- growth located on the lingual side of the man- dible, in the canine or premolar region, above the attachment of the mylohyoid muscle. In most 1 cases, bilateral tori are present. Torus mandibu- Figure 1: Mandibular tori are bony outgrowths on the lingual surface of the laris is usually asymptomatic and discovered mandible, often bilateral and symmetric, as in this 44-year-old patient. incidentally. The prevalence varies substantially between ethnic groups, with lower prevalence in resection is seldom necessary, but is indicated Competing interests: whites (about 8%) and blacks (about 16%) and when ulceration, articulation disorder or prob- None declared. higher prevalence in Asian and Inuit popula- lems inserting dentures are present.3 This article has been peer tions.2 Torus mandibularis is slightly more com- reviewed. -

Abscesses Apicectomy
BChD, Dip Odont. (Mondchir.) MBChB, MChD (Chir. Max.-Fac.-Med.) Univ. of Pretoria Co Reg: 2012/043819/21 Practice.no: 062 000 012 3323 ABSCESSES WHAT IS A TOOTH ABSCESS? A dental/tooth abscess is a localised acute infection at the base of a tooth, which requires immediate attention from your dentist. They are usually associated with acute pain, swelling and sometimes an unpleasant smell or taste in the mouth. More severe infections cause facial swelling as the bacteria spread to the nearby tissues of the face. This is a very serious condition. Once the swelling begins, it can spread rapidly. The pain is often made worse by drinking hot or cold fluids or biting on hard foods and may spread from the tooth to the ear or jaw on the same side. WHAT CAUSES AN ABSCESS? Damage to the tooth, an untreated cavity, or a gum disease can cause an abscessed tooth. If the cavity isn’t treated, the inside of the tooth can become infected. The bacteria can spread from the tooth to the tissue around and beneath it, creating an abscess. Gum disease causes the gums to pull away from the teeth, leaving pockets. If food builds up in one of these pockets, bacteria can grow, and an abscess may form. An abscess can cause the bone around the tooth to dissolve. WHY CAN'T ANTIBIOTIC TREATMENT ALONE BE USED? Antibiotics will usually help the pain and swelling associated with acute dental infections. However, they are not very good at reaching into abscesses and killing all the bacteria that are present. -

Eagle's Syndrome, Elongated Styloid Process and New
Musculoskeletal Science and Practice 50 (2020) 102219 Contents lists available at ScienceDirect Musculoskeletal Science and Practice journal homepage: www.elsevier.com/locate/msksp Masterclass Eagle’s syndrome, elongated styloid process and new evidence for pre-manipulative precautions for potential cervical arterial dysfunction Andrea M. Westbrook a,*, Vincent J. Kabbaz b, Christopher R. Showalter c a Method Manual Physical Therapy & Wellness, Raleigh, NC, 27617, USA b HEAL Physical Therapy, Monona, WI, USA c Program Director, MAPS Accredited Fellowship in Orthopedic Manual Therapy, Cutchogue, NY, 11935, USA ARTICLE INFO ABSTRACT Keywords: Introduction: Safety with upper cervical interventions is a frequently discussed and updated concern for physical Eagle’s syndrome therapists, chiropractors and osteopaths. IFOMPT developed the framework for safety assessment of the cervical Styloid spine, and this topic has been discussed in-depth with past masterclasses characterizing carotid artery dissection CAD and cervical arterial dysfunction. Our masterclass will expand on this information with knowledge of specific Carotid anatomical anomalies found to produce Eagle’s syndrome, and cause carotid artery dissection, stroke and even Autonomic Manipulation death. Eagle’s syndrome is an underdiagnosed, multi-mechanism symptom assortment produced by provocation of the sensitive carotid space structures by styloid process anomalies. As the styloid traverses between the internal and external carotid arteries, provocation of the vessels and periarterial sympathetic nerve fiberscan lead to various neural, vascular and autonomic symptoms. Eagle’s syndrome commonly presents as neck, facial and jaw pain, headache and arm paresthesias; problems physical therapists frequently evaluate and treat. Purpose: This masterclass aims to outline the safety concerns, assessment and management of patients with Eagle’s syndrome and styloid anomalies. -

Chronic Orofacial Pain: Burning Mouth Syndrome and Other Neuropathic
anagem n M e ai n t P & f o M l e Journal of a d n i c r i u n o e J Pain Management & Medicine Tait et al., J Pain Manage Med 2017, 3:1 Review Article Open Access Chronic Orofacial Pain: Burning Mouth Syndrome and Other Neuropathic Disorders Raymond C Tait1, McKenzie Ferguson2 and Christopher M Herndon2 1Saint Louis University School of Medicine, St. Louis, USA 2Southern Illinois University Edwardsville School of Pharmacy, Edwardsville, USA *Corresponding author: RC Tait, Department of Psychiatry, Saint Louis University School of Medicine,1438 SouthGrand, Boulevard, St Louis, MO-63104, USA, Tel: 3149774817; Fax: 3149774879; E-mail: [email protected] Recevied date: October 4, 2016; Accepted date: January 17, 2017, Published date: January 30, 2017 Copyright: © 2017 Raymond C Tait, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Chronic orofacial pain is a symptom associated with a wide range of neuropathic, neurovascular, idiopathic, and myofascial conditions that affect a significant proportion of the population. While the collective impact of the subset of the orofacial pain disorders involving neurogenic and idiopathic mechanisms is substantial, some of these are relatively uncommon. Hence, patients with these disorders can be vulnerable to misdiagnosis, sometimes for years, increasing the symptom burden and delaying effective treatment. This manuscript first reviews the decision tree to be followed in diagnosing any neuropathic pain condition, as well as the levels of evidence needed to make a diagnosis with each of several levels of confidence: definite, probable, or possible. -

Influences of Estrogen and Progesterone on Periodontium 26 Deepa D
CODS Journal of Dentistry Ocial Publication of College of Dental Sciences Alumni Association, Davanagere Volume 6, Issue 1, 2014 CONTENTS Director’s Message 1 V.V. Subba Reddy President’s Message 2 Vasundhara Shivanna Secretary’s Message 3 Praveen S. Basandi Editorial 4 Nandini D.B Original Articles Effect of alcohol containing and alcohol free mouth rinses on microhardness of three 5 esthetic restorative materials Vasundhara Shivanna, Rucha Nilegaonkar Prevalence and distribution of dental anomalies and fluorosis in a small cohort of 9 Indian school children and teenagers Selvamani. M , Praveen S Basandi, Madhushankari G.S Review Articles Paperless dentistry - The future 13 Mala Ram Manohar, Gajendra Bhansali Photo activated disinfection in restorative dentistry - A technical review 16 Deepak B.S, Mallikarjun Goud K, Nishanth P An overview of occupational hazards in dental practice and preventive measures. 19 Poorya Naik .D.S, Chetan .S, Gopal Krishna.B.R, Naveen Shamnur An overview on influences of estrogen and progesterone on periodontium 26 Deepa D CODS Journal of Dentistry 2014, Volume 6, Issue 1 CODS Journal of Dentistry Ocial Publication of College of Dental Sciences Alumni Association, Davanagere Volume 6, Issue 1, 2014 CONTENTS Review Articles Dental home - A new approach for child oral health care 30 Poornima P, Meghna Bajaj, Nagaveni N.B, Roopa K.B, V.V. Subba Reddy Variants of inferior alveolar nerve block: A review 35 Anuradha M, Yashavanth Kumar D.S, Harsha .V. Babji, Rahul Seth Case Reports Ellis-van Creveld syndrome affecting siblings: A case report and review 40 Mamatha G.P, Manisha Jadhav , Rajeshwari G Annigeri, Poornima .P, V.V Subba Reddy Integrated approach of ceramic and composite veneers in tetracycline stained teeth: A case report. -

Pattern of Inflammatory Salivary Gland Diseases Among Sudanese Patients Dr
DOI: 10.21276/sjams Scholars Journal of Applied Medical Sciences (SJAMS) ISSN 2320-6691 (Online) Sch. J. App. Med. Sci., 2017; 5(4F):1668-1673 ISSN 2347-954X (Print) ©Scholars Academic and Scientific Publisher (An International Publisher for Academic and Scientific Resources) www.saspublisher.com Original Research Article Pattern of inflammatory salivary gland diseases among Sudanese patients Dr. Manahil Abuzeid1, Dr. Sharfi Ahmed2, Dr. Yousif O.Yousif3 1MBBS, faculty of Medicine, Bahr El Ghazal University 2Associated Professor, Faculty of Medicine, Omdurman Islamic University, Sudan, DOHNS London UK 3Assisstant Professor, faculty of Dentist, Khartoum University Consultant oral and Maxillofacial surgeon, Sudan *Corresponding author Dr. Sharfi Abdelgadir Omer Ahmed Email: [email protected] Abstract: Inflammatory conditions are the most common pathology to affect the salivary glands. Typical features of a comprehensive range of pathology including obstructive and sialadenitis, Sjogrens syndrome, sarcoidosis and HIV sialopathy. This study aims to know the pattern of inflammatory conditions of the salivary glands among 105 Sudanese patients in Khartoum state. This is a retrospective, cross- sectional, analytic and hospital based study from January 2014 to May 2016. Conducted in Otorhinolaryngological, Head and neck and Oromaxillofacial hospitals. The commonest inflammatory disease is ranula in sublingual glands. The most common site of stones in salivary gland was within glandular tissue. Inflammatory conditions were most common in salivary glands. Keywords: Salivary disease, inflammatory conditions INTRODUCTION within the ductal system of the gland, 80% percent of Inflammatory conditions are the most common all salivary calculi occur in the submandibular gland, pathology to affect the salivary glands [1]. Acute with approximately 70% of these demonstrable as sialadenitis is a bacterial inflammation of the salivary radio-opacities on routine plain radiography consisting gland. -

Eagle's Syndrome
PRACTICE case report Eagle’s syndrome: an unusual cause of a clicking jaw D R P Godden,1 S Adam,2 and R T M Woodwards,3 her jaw, although it could not be palpated. Calcification of the stylohyoid ligament is a well recognised There was mild ill-defined tenderness in radiographic finding in dental practice. Fortunately, affected the right retromandibular region. Exami- individuals seldom develop symptoms. We report a case of a nation of the TMJ was normal, with full patient whose main complaint was a loud click following jaw range of jaw movement, no muscle ten- derness, and no palpable click from the movement. This unusual presentation has not been described joint. Deep palpation of the right tonsillar before and should be considered in the differential diagnosis of fossa elicited tenderness. Examination of ‘clicking jaw’. the pharynx was otherwise normal. The panoral radiograph showed a thickened articulated stylohyoid process. Eagle’s syndrome was diagnosed and the patient Mineralisation of the stylohyoid ligament radiated to the ear. Her medical practi- underwent excision through an extra-oral is a well recognised radiographic finding tioner suspected internal derangement of approach. Through a skin crease incision, and an incidence of 18.2% has been the temporomandibular joint (TMJ) and the carotid artery, internal jugular vein reported on panoramic radiographs.1 advised her to consult her dental practi- and IX, X, XI and XII cranial nerves were The majority of patients are asympto- tioner. A panoral radiograph was taken dissected out and the stylohyoid ligament matic. However, in 1937, Eagle was the (fig. -
Pdf 461.11 K
http:// ijp.mums.ac.ir Original Article (Pages: 381-39 0) Clinical and Histopathological Profiles of Pediatric and Adolescent Oral and Maxillofacial Biopsies in a Persian Population Shirin Saravani1, *Hamideh Kadeh1, Foroogh Amirabadi2, Narges Keramati3 1 Dental Research Center, Department of Oral & Maxillofacial Pathology, Faculty of Dentistry, Zahedan University of Medical Science, Zahedan, Iran. 2 Dental Research Center, Department of Pediatric dentistry, Faculty of Dentistry, Zahedan University of Medical Science, Zahedan, Iran. 3 Department of Oral & Maxillofacial Pathology, Faculty of Dentistry, Zahedan University of Medical Science, Zahedan, Iran. Abstract Introduction The frequency of pediatric and adolescent oral and maxillofacial lesions is various in different societies. The present study was aimed at investigating the frequency of oral and maxillofacial pediatric and adolescent biopsies in Zahedan, Southeastern Iran, and compare the results with other epidemiologic studies. Methods and Materials This retrospective study reviewed oral and maxillofacial lesions in patients aged 0-18 years old referring to the treatment centers of Zahedan University of Medical Sciences, during 12-years period. Patients’ demographic information including age, gender and location of the lesion were collected and statistically analyzed with SPSS software, version 19. Results In general, among 1112 oral and maxillofacial lesions, 154 (13.9%) cases were related to children and adolescents younger than 18 years old. The average age of patients was 11.4 ± 4.9, 53.2% and 46.8% of them were boys and girls, respectively. The most frequent sites of lesions were the gingiva and lip. The most prevalent lesions included inflammatory/reactive, cystic and neoplastic lesions, respectively. Benign and malignant tumors comprised 12.3% and 4.5% of cases. -

Oral Pathology Final Exam Review Table Tuanh Le & Enoch Ng, DDS
Oral Pathology Final Exam Review Table TuAnh Le & Enoch Ng, DDS 2014 Bump under tongue: cementoblastoma (50% 1st molar) Ranula (remove lesion and feeding gland) dermoid cyst (neoplasm from 3 germ layers) (surgical removal) cystic teratoma, cyst of blandin nuhn (surgical removal down to muscle, recurrence likely) Multilocular radiolucency: mucoepidermoid carcinoma cherubism ameloblastoma Bump anterior of palate: KOT minor salivary gland tumor odontogenic myxoma nasopalatine duct cyst (surgical removal, rare recurrence) torus palatinus Mixed radiolucencies: 4 P’s (excise for biopsy; curette vigorously!) calcifying odontogenic (Gorlin) cyst o Pyogenic granuloma (vascular; granulation tissue) periapical cemento-osseous dysplasia (nothing) o Peripheral giant cell granuloma (purple-blue lesions) florid cemento-osseous dysplasia (nothing) o Peripheral ossifying fibroma (bone, cartilage/ ossifying material) focal cemento-osseous dysplasia (biopsy then do nothing) o Peripheral fibroma (fibrous ct) Kertocystic Odontogenic Tumor (KOT): unique histology of cyst lining! (see histo notes below); 3 important things: (1) high Multiple bumps on skin: recurrence rate (2) highly aggressive (3) related to Gorlin syndrome Nevoid basal cell carcinoma (Gorlin syndrome) Hyperparathyroidism: excess PTH found via lab test Neurofibromatosis (see notes below) (refer to derm MD, tell family members) mucoepidermoid carcinoma (mixture of mucus-producing and squamous epidermoid cells; most common minor salivary Nevus gland tumor) (get it out!)