Glycophorins and the MNS Blood Group System: a Narrative Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Duffy, and Mnss Group Systems
Blood Groups – Duffy, and MNSs Group Systems Qun Lu, MD Assistant Professor Division of Transfusion Medicine Department of Pathology and Laboratory Medicine UCLA, School of Medicine Los Angeles, California 2009-03-12 Duffy Blood Group System History . 1950: Mrs. Duffy, a multiply transfused hemophiliac woman, developed an antibody not reacting with the known RBC antigens. Corresponding antigen was named after Mrs. Duffy . 1951: Fyb antibody was described in a woman with 3 pregnancies. 1955: Majority of blacks tested Fy(a-b-) . 1975: Fy(a-b-) RBCs were shown to resist infection by malaria organism Plasmodium vivax. Later: more Duffy antigens (Fy3, Fy4, Fy5, Fy6) were discovered . ISBT: 008 for the Duffy Blood Group Duffy Antigens . Most common: Fya and Fyb. Present at 6 weeks of gestation, well developed at birth – anti- Fy can cause hemolytic disease of newborn . Duffy antigens can be destroyed by enzymes such as ficin, papain, bromelain, chymotrypsin, ZZAP . When compared to Rh or Kell antigens, Duffy antigens are not very immunogenic. So, anti-Fya or anti-Fyb is not common. Fy (a-b-) is not Fy null, but homozygous for Fyb gene, they express Fyb antigen in other tissues, but not on RBCs → only will produce anti-Fya, not anti-Fyb. Fy (a-b-) is negative for Fy6 antigen which is the receptor for P. vivax (Fy6 is + when Fya + or Fyb+) Duffy Antigens . Phenotype Frequencies Chinese Phenotype Whites % Blacks % % Fy (a+b-) 17 9 90.8 Fy (a+b+) 49 1 8.9 Fy (a-b+) 34 22 0.3 Fy (a-b-) rare 68 0 White donor population: Fya: 66% Caucasians, 10% Blacks, 99% Asians Fya – units: 35% Fyb: 83% Caucasians, 23% Blacks, 18.5% Asians Fyb – units: 15% Fy3: 100% Caucasians, 32% Blacks, 99.9% Asians Duffy Antigens . -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Journal of Blood Group Serology and Molecular Genetics Volume 34, Number 1, 2018 CONTENTS
Journal of Blood Group Serology and Molecular Genetics VOLUME 34, N UMBER 1, 2018 This issue of Immunohematology is supported by a contribution from Grifols Diagnostics Solutions, Inc. Dedicated to advancement and education in molecular and serologic immunohematology Immunohematology Journal of Blood Group Serology and Molecular Genetics Volume 34, Number 1, 2018 CONTENTS S EROLOGIC M ETHOD R EVIEW 1 Warm autoadsorption using ZZAP F.M. Tsimba-Chitsva, A. Caballero, and B. Svatora R EVIEW 4 Proceedings from the International Society of Blood Transfusion Working Party on Immunohaematology Workshop on the Clinical Significance of Red Blood Cell Alloantibodies, Friday, September 2, 2016, Dubai A brief overview of clinical significance of blood group antibodies M.J. Gandhi, D.M. Strong, B.I. Whitaker, and E. Petrisli C A S E R EPORT 7 Management of pregnancy sensitized with anti-Inb with monocyte monolayer assay and maternal blood donation R. Shree, K.K. Ma, L.S. Er and M. Delaney R EVIEW 11 Proceedings from the International Society of Blood Transfusion Working Party on Immunohaematology Workshop on the Clinical Significance of Red Blood Cell Alloantibodies, Friday, September 2, 2016, Dubai A review of in vitro methods to predict the clinical significance of red blood cell alloantibodies S.J. Nance S EROLOGIC M ETHOD R EVIEW 16 Recovery of autologous sickle cells by hypotonic wash E. Wilson, K. Kezeor, and M. Crosby TO THE E DITOR 19 The devil is in the details: retention of recipient group A type 5 years after a successful allogeneic bone marrow transplant from a group O donor L.L.W. -

Bioinformatics Analyses of Genomic Imprinting
Bioinformatics Analyses of Genomic Imprinting Dissertation zur Erlangung des Grades des Doktors der Naturwissenschaften der Naturwissenschaftlich-Technischen Fakultät III Chemie, Pharmazie, Bio- und Werkstoffwissenschaften der Universität des Saarlandes von Barbara Hutter Saarbrücken 2009 Tag des Kolloquiums: 08.12.2009 Dekan: Prof. Dr.-Ing. Stefan Diebels Berichterstatter: Prof. Dr. Volkhard Helms Priv.-Doz. Dr. Martina Paulsen Vorsitz: Prof. Dr. Jörn Walter Akad. Mitarbeiter: Dr. Tihamér Geyer Table of contents Summary________________________________________________________________ I Zusammenfassung ________________________________________________________ I Acknowledgements _______________________________________________________II Abbreviations ___________________________________________________________ III Chapter 1 – Introduction __________________________________________________ 1 1.1 Important terms and concepts related to genomic imprinting __________________________ 2 1.2 CpG islands as regulatory elements ______________________________________________ 3 1.3 Differentially methylated regions and imprinting clusters_____________________________ 6 1.4 Reading the imprint __________________________________________________________ 8 1.5 Chromatin marks at imprinted regions___________________________________________ 10 1.6 Roles of repetitive elements ___________________________________________________ 12 1.7 Functional implications of imprinted genes _______________________________________ 14 1.8 Evolution and parental conflict ________________________________________________ -

Cellular and Molecular Signatures in the Disease Tissue of Early
Cellular and Molecular Signatures in the Disease Tissue of Early Rheumatoid Arthritis Stratify Clinical Response to csDMARD-Therapy and Predict Radiographic Progression Frances Humby1,* Myles Lewis1,* Nandhini Ramamoorthi2, Jason Hackney3, Michael Barnes1, Michele Bombardieri1, Francesca Setiadi2, Stephen Kelly1, Fabiola Bene1, Maria di Cicco1, Sudeh Riahi1, Vidalba Rocher-Ros1, Nora Ng1, Ilias Lazorou1, Rebecca E. Hands1, Desiree van der Heijde4, Robert Landewé5, Annette van der Helm-van Mil4, Alberto Cauli6, Iain B. McInnes7, Christopher D. Buckley8, Ernest Choy9, Peter Taylor10, Michael J. Townsend2 & Costantino Pitzalis1 1Centre for Experimental Medicine and Rheumatology, William Harvey Research Institute, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, Charterhouse Square, London EC1M 6BQ, UK. Departments of 2Biomarker Discovery OMNI, 3Bioinformatics and Computational Biology, Genentech Research and Early Development, South San Francisco, California 94080 USA 4Department of Rheumatology, Leiden University Medical Center, The Netherlands 5Department of Clinical Immunology & Rheumatology, Amsterdam Rheumatology & Immunology Center, Amsterdam, The Netherlands 6Rheumatology Unit, Department of Medical Sciences, Policlinico of the University of Cagliari, Cagliari, Italy 7Institute of Infection, Immunity and Inflammation, University of Glasgow, Glasgow G12 8TA, UK 8Rheumatology Research Group, Institute of Inflammation and Ageing (IIA), University of Birmingham, Birmingham B15 2WB, UK 9Institute of -
Flow Reagents Single Color Antibodies CD Chart
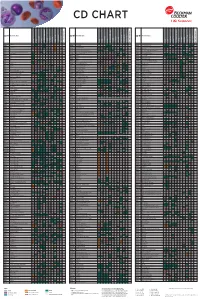
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Analysis of RNA Expression Profiles Identifies Dysregulated Vesicle Trafficking Pathways in Creutzfeldt-Jakob Disease
Molecular Neurobiology (2019) 56:5009–5024 https://doi.org/10.1007/s12035-018-1421-1 Analysis of RNA Expression Profiles Identifies Dysregulated Vesicle Trafficking Pathways in Creutzfeldt-Jakob Disease Anna Bartoletti-Stella1 & Patrizia Corrado2 & Nicola Mometto2 & Simone Baiardi2 & Pascal F. Durrenberger3 & Thomas Arzberger4,5 & Richard Reynolds6 & Hans Kretzschmar5 & Sabina Capellari1,2 & Piero Parchi1,7 Received: 18 July 2018 /Accepted: 1 November 2018 /Published online: 16 November 2018 # Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Functional genomics applied to the study of RNA expression profiles identified several abnormal molecular processes in experimental prion disease. However, only a few similar studies have been carried out to date in a naturally occurring human prion disease. To better characterize the transcriptional cascades associated with sporadic Creutzfeldt-Jakob disease (sCJD), the most common human prion disease, we investigated the global gene expression profile in samples from the frontal cortex of 10 patients with sCJD and 10 non-neurological controls by microarray analysis. The comparison identified 333 highly differentially expressed genes (hDEGs) in sCJD. Functional enrichment Gene Ontology analysis revealed that hDEGs were mainly associated with synaptic transmission, including GABA (q value = 0.049) and glutamate (q value = 0.005) signaling, and the immune/ inflammatory response. Furthermore, the analysis of cellular components performed on hDEGs showed a compromised regu- lation of vesicle-mediated transport with mainly up-regulated genes related to the endosome (q value = 0.01), lysosome (q value = 0.04), and extracellular exosome (q value < 0.01). A targeted analysis of the retromer core component VPS35 (vacuolar protein sorting-associated protein 35) showed a down-regulation of gene expression (p value= 0.006) and reduced brain protein levels (p value= 0.002). -
Quantitation of the Number of Molecules of Glycophorins C and D on Normal Red Blood Cells Using Radioiodinatedfab Fragments of Monoclonal Antibodies
Quantitation of the Number of Molecules of Glycophorins C and D on Normal Red Blood Cells Using RadioiodinatedFab Fragments of Monoclonal Antibodies By Jon Smythe, Brigitte Gardner, andDavid J. Anstee Two rat monoclonal antibodies (BRAC 1 and BRAC 1 1 ) cytes. Fabfragments of BRAC 1 1 and ERIC 10 gave values have been produced. BRAC 1 recognizes an epitope com- of 143,000 molecules GPC per red blood cell (RBC). Fab mon to the human erythrocyte membrane glycoproteins fragments of BRAC1 gave 225,000 molecules of GPC and glycophorin C (GPC) and glycophorin D (GPD). BRAC 11 GPD per RBC. These results indicate that GPC and GPD is specific for GPC. Fabfragments of these antibodies and together are sufficiently abundantto provide membrane at- BRlC 10, a murine monoclonal anti-GPC,were radioiodin- tachment sites for all ofthe protein 4.1 in normal RBCs. ated and used in quantitative binding assays to measure 0 1994 by The American Societyof Hematology. the number of GPC and GPD molecules on normal erythro- HE SHAPE AND deformability of the mature human (200,000)" and those reported for GPC (50,000).7 This nu- Downloaded from http://ashpublications.org/blood/article-pdf/83/6/1668/612763/1668.pdf by guest on 24 September 2021 T erythrocyte is controlled by a flexible two-dimensional merical differencehas led to the suggestion that a significant lattice of proteins, which together comprise the membrane proportion of protein 4.1 in normal erythrocyte membranes skeleton.' The major components of the skeleton are spec- must be bound to sites other than GPC and GPD.3 The trin, actin, ankyrin, and protein 4.1. -
In Vitro Selection for Adhesion of Plasmodium Falciparum-Infected Erythrocytes to ABO Antigens Does Not Affect Pfemp1 and RIFIN
www.nature.com/scientificreports OPEN In vitro selection for adhesion of Plasmodium falciparum‑infected erythrocytes to ABO antigens does not afect PfEMP1 and RIFIN expression William van der Puije1,2, Christian W. Wang 4, Srinidhi Sudharson 2, Casper Hempel 2, Rebecca W. Olsen 4, Nanna Dalgaard 4, Michael F. Ofori 1, Lars Hviid 3,4, Jørgen A. L. Kurtzhals 2,4 & Trine Staalsoe 2,4* Plasmodium falciparum causes the most severe form of malaria in humans. The adhesion of the infected erythrocytes (IEs) to endothelial receptors (sequestration) and to uninfected erythrocytes (rosetting) are considered major elements in the pathogenesis of the disease. Both sequestration and rosetting appear to involve particular members of several IE variant surface antigens (VSAs) as ligands, interacting with multiple vascular host receptors, including the ABO blood group antigens. In this study, we subjected genetically distinct P. falciparum parasites to in vitro selection for increased IE adhesion to ABO antigens in the absence of potentially confounding receptors. The selection resulted in IEs that adhered stronger to pure ABO antigens, to erythrocytes, and to various human cell lines than their unselected counterparts. However, selection did not result in marked qualitative changes in transcript levels of the genes encoding the best-described VSA families, PfEMP1 and RIFIN. Rather, overall transcription of both gene families tended to decline following selection. Furthermore, selection-induced increases in the adhesion to ABO occurred in the absence of marked changes in immune IgG recognition of IE surface antigens, generally assumed to target mainly VSAs. Our study sheds new light on our understanding of the processes and molecules involved in IE sequestration and rosetting. -

Journal of Blood Group Serology and Molecular Genetics Volume 33, Number 3, 2017 CONTENTS
Journal of Blood Group Serology and Molecular Genetics VOLUME 33, N UMBER 3, 2017 This issue of Immunohematology is supported by a contribution from Grifols Diagnostics Solutions, Inc. Dedicated to advancement and education in molecular and serologic immunohematology Immunohematology Journal of Blood Group Serology and Molecular Genetics Volume 33, Number 3, 2017 CONTENTS C ASE R EPO R T 99 ABO serology in a case of persistent weak A in a recipient following a group O–matched unrelated bone marrow transplant D.E. Grey, E.A. Fong, C. Cole, J. Jensen, and J. Finlayson O R IGINAL R EPO R T 105 Stability guidelines for dithiothreitol-treated red blood cell reagents used for antibody detection methods in patients treated with daratumumab W.L. Disbro C ASE R EPO R T 110 A LU:−16 individual with antibodies C. Éthier, C. Parent, A.-S. Lemay, N. Baillargeon, G. Laflamme, J. Lavoie, J. Perreault, and M. St-Louis C ASE R EPO R T 114 Postpartum acute hemolytic transfusion reactions associated with anti-Lea in two pregnancies complicated by preeclampsia M. Marchese O R IGINAL R EPO R T 119 Red blood cell phenotype prevalence in blood donors who self- identify as Hispanic C.A. Sheppard, N.L. Bolen, B. Eades, G. Ochoa-Garay, and M.H. Yazer R EVIEW 125 DEL Phenotype D.H. Kwon, S.G. Sandler, and W.A. Flegel 133 138 142 144 A NNOUN C EMENTS A DVE R TISEMENTS I NST R U C TIONS S UBS cr IPTION FO R A UTHO R S I NFO R M AT I O N E DITO R - IN -C HIEF E DITO R IAL B OA R D Sandra Nance, MS, MT(ASCP)SBB Philadelphia, Pennsylvania Patricia Arndt, MT(ASCP)SBB Geralyn M. -

2021 Code Changes Reference Guide
Boston University Medical Group 2021 CPT Code Changes Reference Guide Page 1 of 51 Background Current Procedural Terminology (CPT) was created by the American Medical Association (AMA) in 1966. It is designed to be a means of effective and dependable communication among physicians, patients, and third-party payers. CPT provides a uniform coding scheme that accurately describes medical, surgical, and diagnostic services. CPT is used for public and private reimbursement systems; development of guidelines for medical care review; as a basis for local, regional, and national utilization comparisons; and medical education and research. CPT Category I codes describe procedures and services that are consistent with contemporary medical practice. Category I codes are five-digit numeric codes. CPT Category II codes facilitate data collection for certain services and test results that contribute to positive health outcomes and quality patient care. These codes are optional and used for performance management. They are alphanumeric five-digit codes with the alpha character F in the last position. CPT Category III codes represent emerging technologies. They are alphanumeric five-digit codes with the alpha character T in the last position. The CPT Editorial Panel, appointed by the AMA Board of Trustees, is responsible for maintaining and updating the CPT code set. Purpose The AMA makes annual updates to the CPT code set, effective January 1. These updates include deleted codes, revised codes, and new codes. It’s important for providers to understand the code changes and the impact those changes will have to systems, workflow, reimbursement, and RVUs. This document is meant to assist you with this by providing a summary of the changes; a detailed breakdown of this year’s CPT changes by specialty, and HCPCS Updates for your reference. -

Whole Exome Sequencing in Families at High Risk for Hodgkin Lymphoma: Identification of a Predisposing Mutation in the KDR Gene
Hodgkin Lymphoma SUPPLEMENTARY APPENDIX Whole exome sequencing in families at high risk for Hodgkin lymphoma: identification of a predisposing mutation in the KDR gene Melissa Rotunno, 1 Mary L. McMaster, 1 Joseph Boland, 2 Sara Bass, 2 Xijun Zhang, 2 Laurie Burdett, 2 Belynda Hicks, 2 Sarangan Ravichandran, 3 Brian T. Luke, 3 Meredith Yeager, 2 Laura Fontaine, 4 Paula L. Hyland, 1 Alisa M. Goldstein, 1 NCI DCEG Cancer Sequencing Working Group, NCI DCEG Cancer Genomics Research Laboratory, Stephen J. Chanock, 5 Neil E. Caporaso, 1 Margaret A. Tucker, 6 and Lynn R. Goldin 1 1Genetic Epidemiology Branch, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; 2Cancer Genomics Research Laboratory, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; 3Ad - vanced Biomedical Computing Center, Leidos Biomedical Research Inc.; Frederick National Laboratory for Cancer Research, Frederick, MD; 4Westat, Inc., Rockville MD; 5Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; and 6Human Genetics Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD, USA ©2016 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol.2015.135475 Received: August 19, 2015. Accepted: January 7, 2016. Pre-published: June 13, 2016. Correspondence: [email protected] Supplemental Author Information: NCI DCEG Cancer Sequencing Working Group: Mark H. Greene, Allan Hildesheim, Nan Hu, Maria Theresa Landi, Jennifer Loud, Phuong Mai, Lisa Mirabello, Lindsay Morton, Dilys Parry, Anand Pathak, Douglas R. Stewart, Philip R. Taylor, Geoffrey S. Tobias, Xiaohong R. Yang, Guoqin Yu NCI DCEG Cancer Genomics Research Laboratory: Salma Chowdhury, Michael Cullen, Casey Dagnall, Herbert Higson, Amy A.