The Incidence of Spontaneous Abortion in Mothers with Blood Group O Compared with Other Blood Types
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Study of Blood Group (ABO and RH) Association and Secretor Status of ABH Substances in Patients with Systemic Lupus Erythematosus
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 18, Issue 5 Ser. 12 (May. 2019), PP 31-35 www.iosrjournals.org Study of Blood Group (ABO and RH) Association and Secretor Status of ABH Substances in Patients with Systemic Lupus Erythematosus Dr. Tashi Paleng1, Dr. A. Barindra Sharma2, Dr.Santa Naorem3, Dr. Laikangbam Dayalaxmi4, Dr. Eric Hilton Wanniang5, Dr. Eswara Moorthy G6 1Postgraduate trainee, 2Professor & Head, 3Professor, 4Senoir Resident, 5Postgraduate trainee, 6Postgraduate trainee 1,2,4,5,6Department of Transfusion Medicine, 3Department of Medicine, Regional Institute of Medical Sciences, Imphal-795004, Manipur, India Corresponding Author: Dr. Tashi Paleng Abstract: Individuals who secrete their blood group antigens in the body fluids are called secretors and individuals who do not secrete are called non-secretors. Non-secretors of blood group antigens have been found to be associated with many infectious and autoimmune diseases by many previous studies. The aims of our study were to find out any association between ABO blood group, RhD blood group and secretor status of ABH substances with the patients of Systemic Lupus Erythematosus. This Case Control study was carried out in the Department of Transfusion Medicine in collaboration with the Department of Medicine, Regional Institute of Medical Sciences, Imphal Manipur from September 2016 to August 2018. 75 confirmed SLE patients attending Rheumatology OPD, Department of Medicine and 75 healthy sex matched voluntary blood donors attending blood bank, Department of Tranfusion Medicine have been enrolled in the study. Their blood were typed for ABO and RhD groups using conventional tube technique and saliva were tested for secretor and non-secretor status using heamagglutination inhibition test. -

Journal of Blood Group Serology and Molecular Genetics Volume 34, Number 1, 2018 CONTENTS
Journal of Blood Group Serology and Molecular Genetics VOLUME 34, N UMBER 1, 2018 This issue of Immunohematology is supported by a contribution from Grifols Diagnostics Solutions, Inc. Dedicated to advancement and education in molecular and serologic immunohematology Immunohematology Journal of Blood Group Serology and Molecular Genetics Volume 34, Number 1, 2018 CONTENTS S EROLOGIC M ETHOD R EVIEW 1 Warm autoadsorption using ZZAP F.M. Tsimba-Chitsva, A. Caballero, and B. Svatora R EVIEW 4 Proceedings from the International Society of Blood Transfusion Working Party on Immunohaematology Workshop on the Clinical Significance of Red Blood Cell Alloantibodies, Friday, September 2, 2016, Dubai A brief overview of clinical significance of blood group antibodies M.J. Gandhi, D.M. Strong, B.I. Whitaker, and E. Petrisli C A S E R EPORT 7 Management of pregnancy sensitized with anti-Inb with monocyte monolayer assay and maternal blood donation R. Shree, K.K. Ma, L.S. Er and M. Delaney R EVIEW 11 Proceedings from the International Society of Blood Transfusion Working Party on Immunohaematology Workshop on the Clinical Significance of Red Blood Cell Alloantibodies, Friday, September 2, 2016, Dubai A review of in vitro methods to predict the clinical significance of red blood cell alloantibodies S.J. Nance S EROLOGIC M ETHOD R EVIEW 16 Recovery of autologous sickle cells by hypotonic wash E. Wilson, K. Kezeor, and M. Crosby TO THE E DITOR 19 The devil is in the details: retention of recipient group A type 5 years after a successful allogeneic bone marrow transplant from a group O donor L.L.W. -

In Vitro Selection for Adhesion of Plasmodium Falciparum-Infected Erythrocytes to ABO Antigens Does Not Affect Pfemp1 and RIFIN
www.nature.com/scientificreports OPEN In vitro selection for adhesion of Plasmodium falciparum‑infected erythrocytes to ABO antigens does not afect PfEMP1 and RIFIN expression William van der Puije1,2, Christian W. Wang 4, Srinidhi Sudharson 2, Casper Hempel 2, Rebecca W. Olsen 4, Nanna Dalgaard 4, Michael F. Ofori 1, Lars Hviid 3,4, Jørgen A. L. Kurtzhals 2,4 & Trine Staalsoe 2,4* Plasmodium falciparum causes the most severe form of malaria in humans. The adhesion of the infected erythrocytes (IEs) to endothelial receptors (sequestration) and to uninfected erythrocytes (rosetting) are considered major elements in the pathogenesis of the disease. Both sequestration and rosetting appear to involve particular members of several IE variant surface antigens (VSAs) as ligands, interacting with multiple vascular host receptors, including the ABO blood group antigens. In this study, we subjected genetically distinct P. falciparum parasites to in vitro selection for increased IE adhesion to ABO antigens in the absence of potentially confounding receptors. The selection resulted in IEs that adhered stronger to pure ABO antigens, to erythrocytes, and to various human cell lines than their unselected counterparts. However, selection did not result in marked qualitative changes in transcript levels of the genes encoding the best-described VSA families, PfEMP1 and RIFIN. Rather, overall transcription of both gene families tended to decline following selection. Furthermore, selection-induced increases in the adhesion to ABO occurred in the absence of marked changes in immune IgG recognition of IE surface antigens, generally assumed to target mainly VSAs. Our study sheds new light on our understanding of the processes and molecules involved in IE sequestration and rosetting. -

Journal of Blood Group Serology and Molecular Genetics Volume 33, Number 3, 2017 CONTENTS
Journal of Blood Group Serology and Molecular Genetics VOLUME 33, N UMBER 3, 2017 This issue of Immunohematology is supported by a contribution from Grifols Diagnostics Solutions, Inc. Dedicated to advancement and education in molecular and serologic immunohematology Immunohematology Journal of Blood Group Serology and Molecular Genetics Volume 33, Number 3, 2017 CONTENTS C ASE R EPO R T 99 ABO serology in a case of persistent weak A in a recipient following a group O–matched unrelated bone marrow transplant D.E. Grey, E.A. Fong, C. Cole, J. Jensen, and J. Finlayson O R IGINAL R EPO R T 105 Stability guidelines for dithiothreitol-treated red blood cell reagents used for antibody detection methods in patients treated with daratumumab W.L. Disbro C ASE R EPO R T 110 A LU:−16 individual with antibodies C. Éthier, C. Parent, A.-S. Lemay, N. Baillargeon, G. Laflamme, J. Lavoie, J. Perreault, and M. St-Louis C ASE R EPO R T 114 Postpartum acute hemolytic transfusion reactions associated with anti-Lea in two pregnancies complicated by preeclampsia M. Marchese O R IGINAL R EPO R T 119 Red blood cell phenotype prevalence in blood donors who self- identify as Hispanic C.A. Sheppard, N.L. Bolen, B. Eades, G. Ochoa-Garay, and M.H. Yazer R EVIEW 125 DEL Phenotype D.H. Kwon, S.G. Sandler, and W.A. Flegel 133 138 142 144 A NNOUN C EMENTS A DVE R TISEMENTS I NST R U C TIONS S UBS cr IPTION FO R A UTHO R S I NFO R M AT I O N E DITO R - IN -C HIEF E DITO R IAL B OA R D Sandra Nance, MS, MT(ASCP)SBB Philadelphia, Pennsylvania Patricia Arndt, MT(ASCP)SBB Geralyn M. -

Transfusion Medicine
Transfusion Medicine Dr. Raymond SM Wong Department of Medicine & Therapeutics Prince of Wales Hospital The Chinese University of Hong Kong Content Blood groups Cross-matching and pre-transfusion tests Blood components and blood products Complications of blood transfusion Blood transfusion in specific situations Blood groups ( 血型) Determined by the red cell antigens ( 紅血球抗原) About 400 red blood cell group antigens have been described Individual who lack a particular blood group antigen may produce antibodies ( 抗體) reacting with that antigen and may lead to a transfusion reaction ( 輸血 反應) ABO and rhesus ( 獼因子) groups are the most clinically significant blood groups Blood group antibodies Naturally occurring antibodies occur in plasma of subjects who lack the corresponding antigen and who have not been transfused or been pregnant Most important are anti-A and anti-B Immune antibodies Develop in response to exposure to antigens by transfusion or by trans-placental passage during pregnancy Most important is the Rhesus (Rh) antibody, anti-D ABO blood group system Consists of 3 allelic genes: A, B and O A and B gene control the synthesis of specific enzymes which transform the H substance Ceramide glu gal gnac gal fuc H antigen galnac Ceramide glu gal gnac gal A antigen fuc gal Ceramide glu gal gnac gal B antigen fuc Cell membrane ABO blood group system Phenotype Genotype Naturally occurring (表型) (基因型) Antigens antibodies O OO O Anti-A, anti-B A AA or AO A Anti-B B BB or BO B Anti-A AB AB AB None The O gene is an amorph (無效基因) -

Transfusion in a Rare Case of Para-Bombay Phenotype
TRANSFUSION IN A RARE CASE OF PARA-BOMBAY PHENOTYPE Charlotte Engström1, Stefan Meyer2, Young-Lan Song1, Adriana Komarek1, Alix O’Meara3, Claudia Papet3, Kathrin Neuenschwander2, Christoph Gassner2, Beat M. Frey1 1 Immunohematology, Blood Transfusion Service Zurich, Swiss Red Cross, Switzerland. 2 Molecular Diagnostics & Research, Blood Transfusion Service Zurich, Swiss Red Cross , Switzerland. 3 Hematology/Oncology, Spital Limmattal, Schlieren, Switzerland. Background Results Individuals with Bombay phenotype are characterized by the The routine anti-A, -B and -A/B failed to detect the respective absence of ABH blood group antigens both on the surface of antigens and, most notably, no H-antigen was traceable. The red blood cells (RBCs) and in secretions resulting from RBCs showed only weak agglutination with the potent anti-A/B silenced mutations in FUT1 (h/h) and FUT2 (se/se) genes, serum (Grifols). Only anti-H, but no anti-A or anti-B, was respectively. In contrast, para-Bombay phenotype retains identified in the serum. Initial ABO genotyping by sequence- some H antigen on RBCs either induced from a weakly active specific priming (PCR-SSP) resulted in AB genotype. In order (H+weak/H+weak) or completely silenced FUT1 gene (h/h). to confirm serological H-deficient phenotype a more detailed The latter is mandatory linked with an active FUT2 gene analysis was performed including sequencing of FUT1 and (Se/Se or Se/se) enabling synthesis of ABH-antigens in FUT2 which revealed an active secretor status (Se/Se) but secretions which may be adsorbed from the plasma onto homozygosity for the FUT1*01W.09 allele (c.658C>T, RBCs surface (1, 2). -

Glycophorins and the MNS Blood Group System: a Narrative Review
16 Review Article Page 1 of 16 Glycophorins and the MNS blood group system: a narrative review Genghis H. Lopez1,2, Catherine A. Hyland1,3, Robert L. Flower1,3 1Clinical Services and Research Division, Australian Red Cross Lifeblood, Kelvin Grove, Queensland, Australia; 2School of Medical Science, Griffith Health, Griffith University, Gold Coast, Queensland, Australia; 3School of Biomedical Sciences, Faculty of Health, Queensland University of Technology, Brisbane, Queensland, Australia Contributions: (I) Conception and design: All authors; (II) Administrative support: None; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Genghis H. Lopez, PhD. Clinical Services and Research Division, Australian Red Cross Lifeblood, 44 Musk Avenue, Kelvin Grove, Queensland 4059, Australia. Email: [email protected]. Abstract: The MNS blood group system, International Society of Blood Transfusion (ISBT) 002, is second after the ABO system. GYPA and GYPB genes encode MNS blood group antigens carried on glycophorin A (GPA), glycophorin B (GPB), or on variant glycophorins. A third gene, GYPE, produce glycophorin E (GPE) but is not expressed. MNS antigens arise from several genetic mechanisms. Single nucleotide variants (SNVs) contribute to the diversity of the MNS system. A new antigen SUMI (MNS50), p.Thr31Pro on GPA has been described in the Japanese population. Unequal crossing-over and gene conversion are the mechanisms forming hybrid glycophorins, usually from parent genes GYPA and GYPB. GYPE also contributes to gene recombination previously only described with GYPA. Recently, however, GYPE was shown to recombine with GYPB to form a GYP(B-E-B) hybrid. -

ABO, Rh and Kell) and Ncovid-19 Susceptibility – a Retrospective Observational Study
Relationship between blood group phenotypes (ABO, Rh and Kell) and nCOVID-19 susceptibility – A retrospective observational study. Sudhir Bhandari SMS Medical College and Hospitals, Jaipur, Rajasthan, India Ajeet Singh Shaktawat SMS Medical College and Hospitals, Jaipur, Rajasthan, India Amit Tak ( [email protected] ) SMS Medical College and Hospitals, Jaipur, Rajasthan, India https://orcid.org/0000-0003-2509-2311 Bhoopendra Patel Government Medical College, Barmer, Rajasthan, India Jyotsna Shukla SMS Medical College and Hospitals, Jaipur, Rajasthan, India Sanjay Singhal SMS Medical College and Hospitals, Jaipur, Rajasthan, India Kapil Gupta SMS Medical College and Hospitals, Jaipur, Rajasthan, India Jitendra Gupta SMS Medical College and Hospitals, Jaipur, Rajasthan, India Shivankan Kakkar SMS Medical College and Hospitals, Jaipur, Rajasthan, India Amitabh Dube SMS Medical College and Hospitals, Jaipur, Rajasthan, India Sunita Dia Medstar Washington Hospital Center, Washington DC 20010, USA. Mahendra Dia North Carolina State University, Raleigh, NC 27695-7609, USA. Todd C Wehner North Carolina State University, Raleigh, NC 27695-7609, USA. Research Article Keywords: ABO blood grouping, coronavirus disease, COVID-19, multinomial test Page 1/13 Posted Date: July 10th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-39611/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 2/13 Abstract Since the outbreak of coronavirus disease-19 research has been continued to explore multiple facets of the disease. The objective of the present study is to evaluate the relationship between blood group phenotypes and COVID-19 susceptibility. In this hospital based, retrospective observational study 132 COVID-19 patients were enrolled from SMS Medical College and attached Hospitals, Jaipur, India after the proper approval from the institutional ethics committee. -

An Update on the Lewis Blood Group System
B LOOD G ROUP R EVIEW An update on the Lewis blood group system M.R. Combs This update of the Lewis blood group system (Combs MR. Lewis chills, severe back pain, hemoglobinuria, and increased levels blood group system review. Immunohematology 2009;25:112–8) of bilirubin, alanine transaminase, and serum creatinine. A describes new information on the clinical significance of Lewis monocyte monolayer assay, testing the patient’s serum with antigens regarding susceptibility of individuals to certain diseases and the possible role of bacteria in Lewis expression. This update the Le(a+) RBCs causing the reaction, was positive also describes recently reported examples of Lewis antibodies A case report in 2015 of a possible HTR due to anti-Lea causing hemolytic transfusion reactions. No new antigens have was reported in a pregnant patient with sickle cell disease with been identified in the International Society of Blood Transfusion a 10 system 7, leaving the antigen count to stand at six: Lea, Leb, LebH, a 37°C gel-reactive anti-Le . The crossmatch was compatible ALeb, BLeb, and Leab. Immunohematology 2019;35:65–66. using prewarmed plasma neutralized with Lewis substance. During transfusion, the patient experienced significant Key Words: Lewis, fucosyltransferases, antigen, antibody dyspnea, hypotension, and hemoglobinuria. Indirect bilirubin and lactate dehydrogenase tests were elevated. The direct Lewis Antigens antiglobulin test on the post-transfusion sample was negative, indicating the possibility that all incompatible RBCs were Lewis antigen fucosyltransferases are encoded by the cleared. FUT3 gene located on chromosome 19p13.3.1 The presence or A case of an HTR due to anti-Leb, also in 2015, was absence of Lewis antigens in an individual can be associated reported.11 A pretransfusion sample from a 30-year-old with the individual’s susceptibility to certain diseases and African-American woman showed a negative antibody infections. -
Jo Shorthouse
Jo Shorthouse Scientific Training Co-ordinator NHSBT Sheffield Scientific and Clinical Development To provide an overview of the following: Antigens and antibodies ABO blood group system Rh blood group system Other clinically significant blood group systems Scientific and Clinical Development Antigens are part of the surface of cells Red blood cells, white blood cells and platelets all have antigens Antibodies are protein molecules - called immunoglobulins (Ig) Usually of the immunoglobulin classes: IgG and IgM Found in the plasma Produced by the immune system following exposure to a foreign antigen Reactions to blood usually occurs when the antigen on the cells reacts with an antibody in the plasma Scientific and Clinical Development There are 30 known blood group systems Most clinically important are the ABO and Rh antigens Antigens in transfused blood can stimulate a patient to produce an antibody but only if the patient lacks the antigen themselves. The frequency of antibody production is very low but increases the more transfusions that are given Scientific and Clinical Development Blood transfusion i.e. blood carrying antigens foreign to the patient Pregnancy Foetal antigen entering maternal circulation during pregnancy or at birth stimulating antibody in mother Environmental factors (ie naturally acquired as with anti-A and anti-B) Scientific and Clinical Development IN VIVO (in the body) leads to the destruction of the cell either: directly when the cell breaks up in the blood stream (intravascular) indirectly where liver and -

Secretor Status, Fucosyltransferase 2 (Fut2) Gene Polymorphisms and Susceptibility to Hiv Infections Among Female Sex Workers in Nairobi, Kenya
SECRETOR STATUS, FUCOSYLTRANSFERASE 2 (FUT2) GENE POLYMORPHISMS AND SUSCEPTIBILITY TO HIV INFECTIONS AMONG FEMALE SEX WORKERS IN NAIROBI, KENYA Nadia Musimbi Chanzu W80/83581/2012 A Thesis Submitted in Fulfillment for the Degree of Doctor of Philosophy (Ph.D) in the University of Nairobi Institute of Tropical and Infectious Diseases University of Nairobi 2014 DECLARATION This Thesis is my original work and has not been presented for a degree in any other University. Nadia Musimbi Chanzu Signed: ………………………………………………… This Thesis has been presented with our approval as University Supervisors: Prof. Walter Mwanda, MBChB., MD. Signed: …………………………………………… Date: ……………………………………………… Prof. Omu Anzala, MBChB, PhD. Signed: …………………………………………… Date: ……………………………………………… Dr. Julius Oyugi, MSc. Ph.D Signed: …………………………………………… Date: ……………………………………………… ii DEDICATION This Thesis is dedicated to my parents, Yusuf Chanzu and Jamila Chanzu, my siblings, Abdalla, Issa, and Zahra. Thank you for the confidence you have always had in me. Thank you for your tremendous encouragement, support and prayers. I also dedicate this book to my late grandfather Abdalla Baraka Chanzu and my late great grandfather Baraka Lwoya Chanzu for their foresightedness which encouraged our family acquire high level quality education. iii ACKNOWLEDGEMENTS This work has had the support and goodwill of so many people that it is difficult to acknowledge each one of them individually, I would like to thank my entire family for their continued support. A special mention to my mother Jamila Chanzu, for always encouraging me to pursue my dreams, and teaching me that education was truly the key to success, her patience and kind heart. My father, Yusuf Chanzu for his continued support, mentorship and for teaching me that there is nothing impossible. -
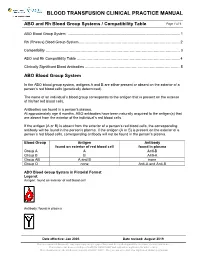
ABO and Rh Blood Group Systems / Compatibility Table Page 1 of 6
BLOOD TRANSFUSION CLINICAL PRACTICE MANUAL ABO and Rh Blood Group Systems / Compatibility Table Page 1 of 6 ABO Blood Group System .............................................................................................................. 1 Rh (Rhesus) Blood Group System………….………………………………………….………………….. 2 Compatibility …………………………………………………………………………………………………. 3 ABO and Rh Compatibility Table ……………………………………………………………………….…. 4 Clinically Significant Blood Antibodies ………………………………………………………...………..… 5 ABO Blood Group System In the ABO blood group system, antigens A and B are either present or absent on the exterior of a person’s red blood cells (genetically determined). The name of an individual’s blood group corresponds to the antigen that is present on the exterior of his/her red blood cells. Antibodies are found in a person’s plasma. At approximately age 4 months, ABO antibodies have been naturally acquired to the antigen(s) that are absent from the exterior of the individual’s red blood cells. If the antigen (A or B) is absent from the exterior of a person’s red blood cells, the corresponding antibody will be found in the person’s plasma. If the antigen (A or B) is present on the exterior of a person’s red blood cells, corresponding antibody will not be found in the person’s plasma. Blood Group Antigen Antibody found on exterior of red blood cell found in plasma Group A A Anti-B Group B B Anti-A Group AB A and B none Group O none Anti-A and Anti-B ABO Blood Group System in Pictorial Format Legend: Antigen: found on exterior of red blood cell Antibody: found in plasma Date effective: Jan 2005 Date revised: August 2019 This is a controlled document.