“To Tell Or Not? the Omission of Truth Becomes a Lie!”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Updated Education Bulletin Volume 2 Issue 5.Pdf
May, 2014 - Volume: 2, Issue: 5 IN THIS BULLETIN HIGHLIGHTS: Higher Education Commission holds bilingual debates for 02 English News 2-8 university students Education Sector 9-12 KP Government announces education fund 03 Framework News Reforms in education only way to make Pakistan a developed 03 country: PM Nawaz Humanitarian Intervention's 13 Call for curricula reforms: IPC says education is a provincial 03 subject Education Profile - 14-16 President reiterates Government’s resolve to promote 04 Kurram Agency education $7 million from Malala Fund for education project in remote 06 Articles 18,20 areas Maps 17,19,21 Government doing all to promote technical 06 education: President Urdu News 22-25 Rs. 3.67b funds will offset impact of damages caused to 07 Fata education Education Directory 26-38 Army actively involved in education projects cleared in 07 Malakand, FATA KURRAM AGENCY EDUCATION FACILITIES KURRAM AGENCY PUBLIC EDUCATION STATS MAPS FATA - TEACHERS SATISTICS-2013 KURRAM AGENCY PUBLIC EDUCATION STATS Legend Enrolment ( % of total in Distict) 8.3 13.3 78.4 54.7% 42.0% Institutions (% of total in District) Teacher (% of total in District) National Boundary UPPER KURRAM District Boundary 78.4% K h y b e r A g e n c y Bajaur Agency Mohmand Agency Afghanistan Khyber Agency K u r r a m 36.0% Kurram Orakzai FR Peshawar Agency Agency FR Kohat A g e n c y 27.7% FR Bannu N. Wazirastan CENTRAL Institutions by Level O r a k z a ii FR Lakki KURRAM Primary Middle High H. -
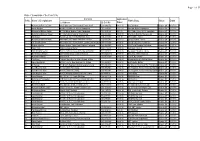
2016 Contacts Application Sr No
Page 1 of 29 Data of Complaints of the Year 2016 Contacts Application Sr No. Name of Complainant Public Body Status Dated (i) Address (II) Cell No Dated 1 Muhammad Faheem Zafar Adv. High Court, Tehsil Kachari Tonsa Sharif 0333-6466553 04-11-15 U C DG Khan Dispose Off 31-07-18 2 Arslan Muzamil H # NE-733, Moh Ch. Feroze Rawalpindi 0312-5641962 22-02-16 Principal GGHS, Rawalpindi Dispose Off 31-07-18 3 Muhammad Rizwan Safdar H # 7-Z-Block, Madina Town, Faisalabad 0333-8396122 19-4-16 Div. Public School & Col. Jaranwala Dispose Off 31-07-18 4 Muhammad Manzoor Anwar H # 292-A-Block Satellite Town Jhang 0333-6502442 15-09-15 Chairman, Board of Revenue Lhr Dispose Off 31-07-18 5 Rab Nawaz Karamt Cly. UC 117, Wahdat Rd. Lahore 0334-4125962 28-7-15 SP Dicipline, Lahore Dispose Off 31-07-18 6 Muhammad Waseem Elahi Adv. High Court - Baitul Raza Civil Line Guj 0333-8158180 23-01-17 CM Secretariat, Lahore Dispose Off 31-07-18 7 Ch. Shoaib Saleem Adv. High Court - Sunny Centre, Layers Lane Mozang 0345-4131863 13-06-16 Punjab Education Foundation Dispose Off 02-08-18 8 Ghulam Mustafa Nawan Shahar, Tehsil Pindi Bhattian, Hafizabad 0300-9564379 09-03-16 EDO Fin & Planning, Hafizabad Dispose Off 31-07-18 9 Aman Ullah Mahmoodaabad, Multan 0347-2220733 29-09-16 IG Punjab Lahored Dispose Off 24-07-18 10 Riaz Ahmad Cheema H # 1-3, F-Block, Navel Anchorage Islamabad 0332-5883822 28-03-16 Secretary Education, Lahore Dispose Off 31-07-18 11 Ms Rukhsana Begum GGPS Maila Bangi, Issakhail,Mianwali 0333-6656806 31-08-15 Distt. -

SHALAMAR INSTITUTE of HEALTH SCIENCES the Shalamar Times Vol: LVII-57 Pages: 24 Edition:Rajab 1439 April 2018
SHALAMAR INSTITUTE OF HEALTH SCIENCES The Shalamar Times Vol: LVII-57 Pages: 24 Edition:Rajab 1439 April 2018 "O Allah, Lord of mankind!, remove our suffering. Heal us as you are the healer, and none can heal but You. I beg You to bring about healing that leaves behind no ailment." Source: (Saheeh Al-Bukhari Hadith No. 5675 ) CONTENTS Chairman’s Message 2 Chief Executive’s Message 3 SPECIAL FEATURE: Department of Anesthesia & ICU 4 Inaugural Ceremony of SHALAMAR LAB Shalamar Radiology Center 5 Lab Collection Centers at Naseer OUTREACH PROGRAMME Hospital & Ammar Medical Complex 5 Inauguration Ceremony of Pulmonology Clinic 6 Seminar on Shalamar Radiology Center 6 SMDC 3rd Convocation 7 2nd Infection Control Workshop 7 Friends of Shalamar-Annual Dinner 8-9 The First International Conference at SMDC 10 Mobile Healthcare Unit - SiDER 11 AO Trauma Workshop 11 Pinning and Candle Lighting Ceremony 12 Symposium on Spectrum of Endocrinology 12 Leadership in Healthcare Management 13 Independence Day Celebrations 13 Rescue 1122 Training Workshop 14 Shalamar Nursing Symposium 14 The International Nursing Day 15 SSAHS Orientation of Students (First Year) 16 Medical Camps 17-19 Financial Highlights 19 New Clinics 20 Visits : Friends of Shalamar 21-22 Awareness Walk & General Public Seminar on Diabetes 23 Naming Ceremony of Hashmat Effendi Burn & Plastic Surgery Department 23 For less than Rs. 100 a day you can change a child's life. SIHS.ShalamarHospital shalamar.institute sihs.org.pk 111-205-205 Ext: 433, 443 SHALAMAR INSTITUTE OF HEALTH SCIENCES CHAIRMAN'S MESSAGE Our journey forward accelerated in 2017 Dental College, equipped with as we continued to improve our quality state-of-the-art laboratories, training of healthcare through innovation, aids, an outstanding faculty and superior high-impact research and dedicated teaching programmes, is well on its way efforts. -

Socio-Economic Inequalities and Their Impact on Health in Pakistan
International Journal of Research in Nursing Literature Reviews Socio-Economic Inequalities and their Impact on Health in Pakistan Sana Sehar Vincent Nursing College, Shalamar Nursing College, Pakistan Article history Abstract: This article critically reviews published literature on the Received: 08-02-2016 relationship between socioeconomic inequalities and health outcomes in Revised: 05-07-2016 Pakistan. Studies are systematically assessed in terms to find the Accepted: 13-07-2016 relationship between the social, economic, political and biological determinants to health. The studies shown that the genetical Email: [email protected] abnormalities, malnutrition and terrorism have significantly affected the quality of life. Moreover, international relations and the national policies have adversely affected the health outcome in the masses of population. Among the socio-economic determinants social exclusion and discrimination, being woman, health compliance, economic polarization in the society, education level, unemployment and work jeopardizes derives the inequality in health of the population which eventually has the implications on the poor economy of the country. Keywords: Socio-Economic Determinants, Health Inequalities, Pakistan Introduction Socioeconomic Inequalities (SEIs) and their impact on the economy is the most advantageous action for the Health is an important ‘consumption good’ that population. SEIs in health have a direct impact on the directly contributes to an individual’s ‘happiness’ or economy of the country. The larger the SEI, the greater ‘satisfaction’ with no other substitute. It is also a ‘capital are the magnitude of the burden of ill health and good’ in terms of assets to the nation too as well as an premature mortality associated with inequalities in important component which human beings value. -
News Letter2021
SHALAMAR INSTITUTE OF HEALTH SCIENCES Shalamar Timeswww.sihs.org.pk Vol: LVIl-61 Pages:08 Edition: Shaban/Ramzan -1442 April 2021 ALWAYS BY YOURSIDE A Not-for-Profit Tertiary Care Hospital Providing Diagnostic and Treatment Facilities Since 1982 21+Clinical Departments and Specialties 500+Beds 11Operation Theaters 467,518 Patients Provided Subsidized Treatment Worth Rs. 234 Million During 2019-20 Shalimar Link Road, Lahore. facebook.com/SIHS.ShalamarHospital sihs.org.pk 042-111-205-205 Ext: 433, 443 SHALAMAR INSTITUTE OF HEALTH SCIENCES 5th International Conference February 04-06: The 5th International The opening ceremony of the • 3rd Prize ( Rs. 10,000/-) (Virtual) Conference titled “Together conference was chaired by Dr. Attiya Omer Nisar Towards Tomorrow” organized by Mubarik, the Chairman Punjab For the post-graduate ceremony, the Shalamar Medical and Dental College Healthcare Commission. following were the prize winners: kept its tradition alive in taking an The success of any academic activity • 1st Prize ( Rs. 100,000/-) initiative in the field of medical lies in the encouragement of the Dr. Muneeb Ather sciences and proudly hosting five young minds to participate. This year • 2nd Prize ( Rs. 75,000/-) successful International Conferences. the students of different medical Dr. Maryam Ashfaq The journey began with “Innovations colleges participated in the • 3rd Prize ( Rs. 50,000/-) in Healthcare” in 2017 with 1138 conference as young researchers for Ms. Zarrin Atif registered participants and 17 online presentations. These pre-conference workshops. In 2018, the 2nd International Conference “Beyond Horizons” was attended by 2167 participants and had 42 pre-conference workshops. The 3rd conference “Navigating the Future” in 2019 had 3000 registered participants and the number of pre-conference workshops escalated to 49. -

Knowledge and Attitude of Nurses Regarding Healthcare Waste Management Practices in a Tertiary Care Hospitalsoflahore
ORIGINAL ARTICLE Knowledge and Attitude of Nurses Regarding Healthcare Waste Management Practices in a Tertiary care HospitalsofLahore TANZEEL UL RAHMAN1, SAJID HAMEED2, SHAHJEHAN3, SADAF AYYAZ4, RANA M AKHTAR KHAN5 ABSTRACT Background: Healthcare waste is considered infectious and hazardous. It requires specific handling prior to its disposal and poses a stern dangers to ecological, occupational and public health if not managed with caution. Hazardous waste management is a concern for every health care organization and for every healthcare professional. As nurses are the primary members of healthcare team and during provision of care to the patients they are the primary people dealing with the healthcare waste. Aim: Toassess knowledge and attitude of nurses regarding healthcare waste management practices. Methodology:A quantitative descriptive cross-sectional Study design was used. Data was collected by a self-administered modified questionnaire, containing 20 questions, from 50 staff nurses of Shalamar Hospital Lahore, using a convenience sampling. The study was carried for the period of October 2011 to December 2011. The collected data was then analyzed and frequencies and percentages were calculated. Result and conclusion: Study revealed that that most of the nurses were not having satisfactory knowledge regarding healthcare waste management practices. Majority of staff nurses were conscious of the measures for safe collection and final disposal of health care and were having positive attitude toward healthcare waste management practices. Keywords: Attitude, knowledge, waste management practice INTRODUCTION Health care waste is produced by the health care infectious waste, pathological waste, sharps, establishments during their functioning(Ilyas, 2004). pharmaceutical waste, geotaxis waste, chemical ThemanagementofHealthcare w a s t e hasbecomea waste and radioactive waste. -

Knowledge, Attitude and Practice Toward Hand Washing Among
Saudi Journal of Nursing and Health Care Abbreviated Key Title: Saudi J Nurs Health Care ISSN 2616-7921 (Print) |ISSN 2616-6186 (Online) Scholars Middle East Publishers, Dubai, United Arab Emirates Journal homepage: https://saudijournals.com Original Research Article Knowledge, Attitude and Practice toward Hand Washing Among Undergraduate Nursing Students in Lahore Mehdi Hayat Khan1, Zubaida Akhtar2*, Jamila3, Nazma Bano4, Shamsa Rafique5 1Sr. Nursing Lecturer, College of Nursing, Shalamar Hospital, Lahore, PO Box 54500, Lahore, Pakistan 2Program Coordinator, College of Nursing, Shalamar Hospital, Lahore, PO Box 54500, Lahore, Pakistan 3Nursing Officer, The Children's Hospital & the Institute of Child Health, Lahore, Pakistan 4Nursing Officer, Kot Khawja Saeed Hospital, Lahore Pakistan 5Nursing Officer, The Children's Hospital & the Institute of Child Health, Lahore, Pakistan DOI: 10.36348/sjnhc.2021.v04i07.001 | Received: 03.05.2021 | Accepted: 08.06.2021 | Published: 06.07.2021 *Corresponding author: Mehdi Hayat Khan Abstract Background: Health care associated infections and emerging multi drug resistance in nosocomial pathogens is perceived as a serious public health threat with grievous concerns. Hand hygiene if practiced properly is cheapest, simplest and most effective tool in tackling this problem. The objective of this study was conducted to assess levels of knowledge, attitude and practice in various aspects of hand hygiene in undergraduate nursing students in the study area for identifying gaps for planning necessary corrective measures. Methods: A cross sectional study involving self- administered pre-structured anonymous questionnaires administered to all undergraduate nursing students (182) enrolled at Shalmar Nursing College Lahore, Pakistan. Results: Most of the study participants exhibited moderate levels of knowledge and practice with marginal difference while attitude were found to exhibit a remarkably higher, difference being statistically significant. -

PAKISTAN: TERTIRY EDUCATION SECTOR ASSESSMENT Consultant
PAKISTAN: TERTIRY EDUCATION SECTOR ASSESSMENT STUDY (6) PRIVATE HIGHER EDUCATION INSTITUTIONS REPORT Consultant Mubashar Ali 1 , TABLE OF CONTENTS Page Executive 4 Summary Abbreviations and 6 Acronyms 1 Introduction 7 2 Methodology 8 3 Findings 9 3.1 Overall picture of the private HEIs’ 9 3.1.1 Health 12 3.1.1 MBBS- BDS 12 3.1.1.2 Pharmacy 17 3.1.1.3 Homeopathy 19 3.1.1.4 TIBB 20 3.1.1.5 Nursing 21 3.1.1.6 Veterinary 23 3.1.1.7 DPT 24 3.1.2 Engineering Education 26 3.1.2.1 Engineering 26 3.1.2.2 Architecture and Town Planning 29 3.1.2.3 B. Tech. 30 3.1.3 Law 33 3.1.4 Deeni Madaris 36 3.1.5 Professional institutions 38 3.1.6 Role of Accreditation Councils for Private HEIs 41 3.1.6.1 NACTE 41 3.1.6.2 NAEAC 43 3.1.6.3 NCEAC 44 3.1.6.4 NBEAC 45 3.1.7 Recognized campuses of private universities 48 3.1.8 Unrecognized private HEIs 49 3.1.9 Private Affiliated colleges 50 3.1.10 Research situation 57 3.1.11 Levels of Degree offered, Disciplines offered 64 3.1.12 Location- urban rural 68 3.1.13 Public/private partnerships 70 3.1.14 Initiation of new programs 72 3.1.15 Distribution of enrollments 73 3.1.16 Contribution towards societal issues 81 3.2 Financial situation- Fees- Scholarship 82 2 , 3.3 Human resources -Faculty 83 3.4 Regulatory framework -Mode of Establishment 85 –Accreditation 3.5 TQM (curriculum, teaching methods, other 94 areas) 3.6.1 Financial benefits to Private HEIs 97 3.6.2 Professional Grooming of HEIs imparted by 98 HEC 3.6.3 Participation of HEC in statuary bodies 98 3.7 99 Caliber to address the issue of Internalization and Globalization 3.8 100 Foreign owned/ franchised private HEIs. -

Education Bulletin 1 Updated
June, 2014 - Volume: 2, Issue: 6 IN THIS BULLETIN HIGHLIGHTS: English News 2-7 Denmark to provide $11m to UNICEF for Pakistan programme 02 Shahbaz lauds British cooperation in education sectors 02 Education Sector 8-9 Prime Minister to disburse fee to 3,184 Sindh varsities 02 Framework News students Hiccups In Higher Education 03 Humanitarian Intervention's 10-11 Schools threatened over co-education in Pakistan’s 03 Balochistan Education Profile - 12-14 Punjab ahead of all provinces but education situation still 03 District Hyderabad bleak Allocation of additional funds for education in Sindh budget 04 Maps 15,17,19,21,23 Open up! Education is coming 04 Private schools in Panjgur closed after threats 05 Articles 16,18 Balochistan government restores 450 schools 05 Child marriages violate right to education: Sharmila 05 Urdu News 20,22,24 New primary schools in KP to have six rooms, six teachers 06 Education sector facing serious challenges, 06 26-38 Education Directory says Former Minister HYDERABAD EDUCATION FACILITIES HYDERABAD EDUCATION SUMMARY MAPS HYDERABAD PUBLIC EDUCATION STATS SINDH - PRIMARY EDUCATION STATS-2013 SINDH - TEACHERS SATISTICS-2013 HYDERABAD EDUCATION SUMMARY Universities Level wise Institutions 1- Liaquat University of Medical & Health Sciences Teachers by Level High High Sec 2- Isra University Middle 3- Mehran University of Engineering Primary and Technology 4- Sindh Agriculture University, Tandojam 5- University of Sindh Institutions 6- National University of Modern Languages having Electricity Hyderabad Campus 7- SZABIST Hyderabad Campus 935 86 86 14 Primary Education Statistics Institutions having 72.0% Boundarywall Number of male teachers 2962 Children (Age 6-16) Research Centres Institutions having Out-ofschool Number of female teachers 2375 Drinking Water (Girls) Institutions having 83.9% Toilets for Students SOLAR ENERGY RESEARCH Number of boys’ primary CENTRE SERC, PCSIR, HYDERABAD. -

Shalamar Institute of Health Sciences Past, Present and Future
Shalamar Institute of Health Sciences Past, Present and Future FINAL ABSTRACT This document presents a brief profile of Shalamar Institute of Health Sciences and its subsidiary organizations. The brief also includes some prospective areas for fund raising. SIHS – Past, Present and Future TABLE OF CONTENTS LIST OF FIGURES 3 LIST OF ABBREVIATIONS 4 EXECUTIVE SUMMARY 5 WHO WE ARE 6 OUR FOUNDERS 6 OUR GOVERNANCE STRUCTURE 7 OUR FUNDING 7 OUR FACILITIES 11 SHALAMAR HOSPITAL 11 SERVICES PROVIDED BY SHALAMAR HOSPITAL 13 SHALAMAR NURSING COLLEGE 15 SHALAMAR MEDICAL AND DENTAL COLLEGE 16 WHAT SETS US APART? 17 CAREFULLY SELECTED GEOGRAPHICAL FOCUS 17 HIGHLY QUALIFIED HUMAN RESOURCE 18 ENVIRONMENTAL RESPONSIVENESS 18 STRATEGIC PARTNERSHIPS 18 STATE-OF-THE-ART INFRASTRUCTURE 18 INTEGRATED APPROACH 19 OUR STRATEGY 21 KEY STRATEGY PILLARS 22 PATIENT-CENTRIC HEALTHCARE SERVICES 22 24-HOURS HIGHLY RESPONSIVE EMERGENCY AND TRAUMA CARE 22 COMMUNITY OUTREACH 22 POOL OF CAPABLE HUMAN RESOURCE 22 SOCIAL RESPONSIBILITY 22 OUR CORE VALUES 23 OUR STRATEGIC ACTION PLAN 2010-15 23 CONCLUSION 24 Page 2 | 29 SIHS – Past, Present and Future LIST OF FIGURES Figure 1: SH Yearly Financial Snapshot 1988-2010 ................................................................................... 8 Figure 2: SIHS Donations Over the Years .................................................................................................. 9 Figure 3: SIHS – Journey Through the Years ........................................................................................... 10 -

Young Professional Students Organization ) YPSO ( Career Guide 2015
Young Professional Students Organization (YPSO ) Career Guide Fee Merits Structure 2015 Tests Scholarships Work for humanity, Serve to humanity Page 1 of 99 Prepared By: M.Zareef Sajid Muhammad Ali Muhammad Imran Bhutta Naimat Ullah Javid Iqbal Work for humanity, Serve to Humanity Contact us: E-mail: [email protected] Twitter: Type FOLLOW YPSO_Taunsa and send to 40404 from your Cell Phone. Phone: Mohsin Rasheed(Gomal DI Khan) 03328883949 Page 2 of 99 Contents Founder’s message………………………………………………………………………………….…………07 Chairman and Vice chairman’s message………………………………………………….…………..08 Vice president’s message……………………………………………………………………………………08 Why should you join a student organization……………………………………………...………..09 Cabinet 2015……………………………………………………………………………………………………..10 Contacts of students ………………………………………………………………………………………….11 Imagine what can you do? …………………………………………………………...…………………….16 Introduction to some important tests…………………………………………..……………………. 20 Engineering universities of Pakistan………………………………………………………..…..21 Merit lists…………………………………………………………………………………………… ……… 23 UET Lahore ……………………………………………………………………………………………...……….23 University College of Engineering & technology Punjab, Lahore…………………………..26 COMSATS institute of information technology…………………………………………………….27 Sharif College of engineering and technology……………………………………………………... 27 University of Lahore……………………………………………………………………………………….. ...27 Islamabad Region ……………………………………………………………………………................28 UET Taxila ………………………………………………………………………...…………………………… ..28 NUST -

HRH Profile for Punjab 2012.Pdf
2012 Human Resources for Health Profile Punjab, Pakistan World Health Organization Human Resource for Health Profile – Punjab, Pakistan i ACKNOWLEDGEMENT The Human Resource for Health Profile for Punjab was undertaken after due approval of the Department of Health, Punjab. PHSRP, on behalf of the Department of Health, Government of Punjab provided full facilitation towards the HRH data collection. Their support was very valuable in accessing the Human Resource for Health Data that existed at varied sources in Punjab. The cooperation of all the focal persons nominated by the Punjab Health Sector Reform Programme (PHSRP) in facilitating the data collection was immense and needs a special acknowledgement. We greatly appreciate their valuable inputs, thoughts and the time and energy they devoted towards this assignment. We are particularly thankful to the Global Health Workforce Alliance (GHWA) for providing catalytic funding support and valuable inputs by sharing of resource materials that provided excellent guidance to the team working on the project. The devoted technical support to the study provided by Dr Muhammad Mahmood Afzal, Head of Country Coordination & Facilitation Team, GHWA is specially acknowledged. We would also like to take the opportunity to acknowledge with thanks the following partners of the Alliance, whose funding contribution to the Alliance has made this piece of work possible: . Bill and Melinda Gates Foundation . Canadian International Development Agency (CIDA) . French Development Agency/Agence Francaise de developpemenet (AFD) . Deutsche Gesellschaft fur International Zusammenarbeit (GIZ) Gmbh . Irish aid, department of Foreign Affairs . Norwegian Agency for Development Cooperation (NORAD) . UK Development for International Development (DFID) . United States Agency for International Development (USAID) The technical support, facilitation and guidance provided by the World Health Organization Country Office in Islamabad and the WHO office in Lahore remained extremely useful and valuable.