Selective Impairment of Gene Expression and Assembly of Nephrin in Human Diabetic Nephropathy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Investigation of the Underlying Hub Genes and Molexular Pathogensis in Gastric Cancer by Integrated Bioinformatic Analyses
bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Investigation of the underlying hub genes and molexular pathogensis in gastric cancer by integrated bioinformatic analyses Basavaraj Vastrad1, Chanabasayya Vastrad*2 1. Department of Biochemistry, Basaveshwar College of Pharmacy, Gadag, Karnataka 582103, India. 2. Biostatistics and Bioinformatics, Chanabasava Nilaya, Bharthinagar, Dharwad 580001, Karanataka, India. * Chanabasayya Vastrad [email protected] Ph: +919480073398 Chanabasava Nilaya, Bharthinagar, Dharwad 580001 , Karanataka, India bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract The high mortality rate of gastric cancer (GC) is in part due to the absence of initial disclosure of its biomarkers. The recognition of important genes associated in GC is therefore recommended to advance clinical prognosis, diagnosis and and treatment outcomes. The current investigation used the microarray dataset GSE113255 RNA seq data from the Gene Expression Omnibus database to diagnose differentially expressed genes (DEGs). Pathway and gene ontology enrichment analyses were performed, and a proteinprotein interaction network, modules, target genes - miRNA regulatory network and target genes - TF regulatory network were constructed and analyzed. Finally, validation of hub genes was performed. The 1008 DEGs identified consisted of 505 up regulated genes and 503 down regulated genes. -

Identification of Novel Kirrel3 Gene Splice Variants in Adult Human
Durcan et al. BMC Physiology 2014, 14:11 http://www.biomedcentral.com/1472-6793/14/11 RESEARCH ARTICLE Open Access Identification of novel Kirrel3 gene splice variants in adult human skeletal muscle Peter Joseph Durcan1, Johannes D Conradie1, Mari Van deVyver2 and Kathryn Helen Myburgh1* Abstract Background: Multiple cell types including trophoblasts, osteoclasts and myoblasts require somatic cell fusion events as part of their physiological functions. In Drosophila Melanogaster the paralogus type 1 transmembrane receptors and members of the immunoglobulin superfamily Kin of Irre (Kirre) and roughest (Rst) regulate myoblast fusion during embryonic development. Present within the human genome are three homologs to Kirre termed Kin of Irre like (Kirrel) 1, 2 and 3. Currently it is unknown if Kirrel3 is expressed in adult human skeletal muscle. Results: We investigated (using PCR and Western blot) Kirrel3 in adult human skeletal muscle samples taken at rest and after mild exercise induced muscle damage. Kirrel3 mRNA expression was verified by sequencing and protein presence via blotting with 2 different anti-Kirrel3 protein antibodies. Evidence for three alternatively spliced Kirrel3 mRNA transcripts in adult human skeletal muscle was obtained. Kirrel3 mRNA in adult human skeletal muscle was detected at low or moderate levels, or not at all. This sporadic expression suggests that Kirrel3 is expressed in a pulsatile manner. Several anti Kirrel3 immunoreactive proteins were detected in all adult human skeletal muscle samples analysed and results suggest the presence of different isoforms or posttranslational modification, or both. Conclusion: The results presented here demonstrate for the first time that there are at least 3 splice variants of Kirrel3 expressed in adult human skeletal muscle, two of which have never previously been identified in human muscle. -

Nephrin Mutations Can Cause Childhood-Onset Steroid-Resistant Nephrotic Syndrome
BRIEF COMMUNICATION www.jasn.org Nephrin Mutations Can Cause Childhood-Onset Steroid-Resistant Nephrotic Syndrome Aure´lie Philippe,*† Fabien Nevo,*† Ernie L. Esquivel,*† Dalia Reklaityte,*† ʈ Olivier Gribouval,*† Marie-Jose`phe Teˆte,*‡ Chantal Loirat,§ Jacques Dantal, Michel Fischbach,¶ Claire Pouteil-Noble,** Ste´phane Decramer,†† Martin Hoehne,‡‡ Thomas Benzing,‡‡ Marina Charbit,‡ Patrick Niaudet,*†‡ and Corinne Antignac*†§§ † *Inserm U574, Hoˆpital Necker-Enfants Malades, Universite´ Paris Descartes, Faculte´deMe´ decine Rene´ Descartes, BRIEF COMMUNICATION ‡Pediatric Nephrology and §§Department of Genetics, Hoˆpital Necker-Enfants Malades, Assistance Publique-Hoˆpitaux de Paris, and §Pediatric Nephrology Department, Universite´ Paris VII, Assistance Publique-Hoˆpitaux de Paris, Hoˆpital ʈ Robert Debre´, Paris, ITERT, Department of Nephrology and Clinical Immunology, CHU Nantes, Nantes, ¶Nephrology Dialysis Transplantation Children’s Unit, Hoˆpital de Hautepierre, Strasbourg, **Transplantation and Nephrology Unit, Centre Hospitalier Lyon-Sud, Pierre-Be´nite, and ††Department of Pediatric Nephrology, Hoˆpital des Enfants, and Inserm, U858/I2MR, Department of Renal and Cardiac Remodeling, Toulouse, France; and ‡‡Department of Medicine IV, University of Cologne, Cologne, Germany ABSTRACT Classically, infants with mutations in NPHS1, which encodes nephrin, present with but has since been described in other nephrotic syndrome within the first 3 mo of life (congenital nephrotic syndrome of populations.3–5 Nephrin is a single-pass the Finnish-type), and children with mutations in NPHS2, which encodes podocin, transmembrane protein consisting of present later with steroid-resistant nephrotic syndrome. Recently, however, eight extracellular Ig-like modules, a fi- NPHS2 mutations have been identified in children with congenital nephrotic syn- bronectin type III–like motif, and a cy- drome. Whether NPHS1 mutations similarly account for some cases of childhood tosolic C-terminal tail. -

Nephrin Is Specifically Located at the Slit Diaphragm of Glomerular Podocytes
Proc. Natl. Acad. Sci. USA Vol. 96, pp. 7962–7967, July 1999 Cell Biology Nephrin is specifically located at the slit diaphragm of glomerular podocytes VESA RUOTSALAINEN*†,PA¨IVI LJUNGBERG*‡§,JORMA WARTIOVAARA¶,ULLA LENKKERI†,MARJO KESTILA¨†, ʈ HANNU JALANKO‡,CHRISTER HOLMBERG‡, AND KARL TRYGGVASON† †Biocenter and Department of Biochemistry, University of Oulu, 90570 Oulu, Finland; ‡Hospital for Children and Adolescents, University Hospital of Helsinki, 00014 Helsinki, Finland; §Department of Bacteriology and Immunology, Haartman Institute and ¶Electron Microscopy Unit, Institute of Biotechnology, University of Helsinki, 00014 Helsinki, Finland; and ʈDivision of Matrix Biology, Department of Medical Biochemistry and Biophysics, Karolinska Institute, 171 77 Stockholm, Sweden Communicated by Peter A. Reichard, Karolinska Institute, Stockholm, Sweden, April 9, 1999 (Received for review February 12, 1999) ABSTRACT We describe here the size and location of tight junction protein ZO-1 (17) has been localized in the nephrin, the first protein to be identified at the glomerular glomerulus, predominantly to points where the slit diaphragm podocyte slit diaphragm. In Western blots, nephrin antibodies is inserted into the lateral cell membrane of the foot process generated against the two terminal extracellular Ig domains of (18). The ZO-1 protein possibly connects the slit diaphragm, recombinant human nephrin recognized a 180-kDa protein in directly or indirectly, to the cytoskeleton. lysates of human glomeruli and a 150-kDa protein in trans- In numerous primary and secondary diseases of the kidney, fected COS-7 cell lysates. In immunofluorescence, antibodies the filtration barrier is affected, resulting in proteinuria, i.e., to this transmembrane protein revealed reactivity in the leakage of albumin and larger plasma proteins into the urine, glomerular basement membrane region, whereas the podocyte with edema and nephrotic syndrome as a consequence. -

NPHS2 (Podocin) Mutations in Nephrotic Syndrome
0031-3998/05/5705-0054R PEDIATRIC RESEARCH Vol. 57, No. 5, Pt 2, 2005 Copyright © 2005 International Pediatric Research Foundation, Inc. Printed in U.S.A. NPHS2 (Podocin) Mutations in Nephrotic Syndrome. Clinical Spectrum and Fine Mechanisms GIANLUCA CARIDI, FRANCESCO PERFUMO, AND GIAN MARCO GHIGGERI Laboratory on Pathophysiology of Uremia [G.C., G.M.C.], and Renal Unit [F.P., G.M.C.], Istituto Giannina Gaslini, 16148 Genova, Italy. ABSTRACT Nephrotic syndrome (NS) is the most frequent cause of iments with the common R229Q polymorphism demonstrated an proteinuria in children and is emerging as a leading cause of altered interaction with nephrin that affects the stability of the uremia. Molecular studies in families with recessive NS have led functional unit. Overall, data are here presented that underscore to the discovery of specialized molecules endowed in podocytes a major role of inherited defects of NPHS2 in NS in children that play a role in proteinuria. This review focalizes the key (including a relevant impact in sporadic cases) and give the position of podocin (NPHS2 gene) in this rapidly evolving field functional rationale for the association. A practical compendium and furnishes a compendium to those involved in clinics and is also given to clinicians involved in the management of NS that genetics of NS. Screening for NPHS2 mutations have been done should modify the classic therapeutic approach. (Pediatr Res 57: in sporadic NS and familial cases with recessive inheritance, 54R–61R, 2005) documenting a mutation detection rate of 45–55% in families and 8–20% in sporadic NS according to the different groups and considering all the clinical phenotypes. -
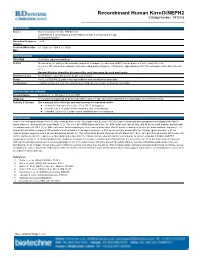
Recombinant Human Kirrel3/NEPH2 Catalog Number: 4910-K3
Recombinant Human Kirrel3/NEPH2 Catalog Number: 4910-K3 DESCRIPTION Source Mouse myeloma cell line, NS0derived Leu29Ala535 & Tyr33Ala535 & Arg41Ala535, all with a Cterminal 6His tag Accession # Q8IZU9 Nterminal Sequence Leu29 Analysis Predicted Molecular 56.1 kDa, 55.7 kDa & 54.7 kDa Mass SPECIFICATIONS SDSPAGE 6585 kDa, reducing conditions Activity Measured by the ability of the immobilized protein to support the adhesion of MS1 mouse pancreatic islet endothelial cells. When 5 x 104 cells/well are added to rhKirrel3 coated plates (30 µg/mL, 100 µL/well), approximately 40%70% will adhere after 90 minutes at 37° C. Optimal dilutions should be determined by each laboratory for each application. Endotoxin Level <0.10 EU per 1 μg of the protein by the LAL method. Purity >95%, by SDSPAGE under reducing conditions and visualized by silver stain. Formulation Lyophilized from a 0.2 μm filtered solution in PBS. See Certificate of Analysis for details. PREPARATION AND STORAGE Reconstitution Reconstitute at 100 μg/mL in sterile PBS. Shipping The product is shipped at ambient temperature. Upon receipt, store it immediately at the temperature recommended below. Stability & Storage Use a manual defrost freezer and avoid repeated freezethaw cycles. l 12 months from date of receipt, 20 to 70 °C as supplied. l 1 month, 2 to 8 °C under sterile conditions after reconstitution. l 3 months, 20 to 70 °C under sterile conditions after reconstitution. BACKGROUND Kirrel3 (kin of irregular chiasm1like 3), also known as Kirre or NEPH2 (nephrinlike 2), is an ~100 kDa type I transmembrane glycoprotein belonging to the NEPH family within the immunoglobulin superfamily (1, 2). -

Human KIRREL / NEPH1 / KIRREL1 Protein (Fc Tag)
Human KIRREL / NEPH1 / KIRREL1 Protein (Fc Tag) Catalog Number: 15752-H02H General Information SDS-PAGE: Gene Name Synonym: NEPH1 Protein Construction: A DNA sequence encoding the human KIRREL (NP_060710.3) (Met1-Leu493) was expressed with the Fc region of human IgG1 at the C-terminus. Source: Human Expression Host: HEK293 Cells QC Testing Purity: > 95 % as determined by SDS-PAGE Endotoxin: Protein Description < 1.0 EU per μg of the protein as determined by the LAL method NEPH1 (KIRREL1) belongs to a family of three closely related Stability: transmembrane proteins of the Ig superfamily with a structure similar to that of nephrin. All three Neph proteins share a conserved podocin-binding ℃ Samples are stable for up to twelve months from date of receipt at -70 motif; mutation of a centrally located tyrosine residue dramatically lowers the affinity of Neph1 for podocin. Neph1 triggers AP-1 activation similarly to Gln 17 Predicted N terminal: nephrin but requires the presence of Tec family kinases for efficient Molecular Mass: transactivation. Neph1 consists of a signal peptide, five Ig-like C2-type domains with the middle domain overlapping with a PKD-like domain, an The recombinant human KIRREL/Fc comprises 715 amino acids and has a RGD sequence, a transmembrane domain and a cytoplasmic tail, which is predicted molecular mass of 78.8 kDa. The apparent molecular mass of the expressed in slit diaphragm domains of podocytes and in vertebrate and protein is approximately 96.1 kDa in SDS-PAGE under reducing conditions. invertebrate nervous systems. Neph1 is abundantly expressed in the kidney, specifically expressed in podocytes of kidney glomeruli, and plays a Formulation: significant role in the normal development and function of the glomerular permeability. -

The Intellectual Disability Gene Kirrel3 Regulates Target-Specific Mossy Fiber
SHORT REPORT The intellectual disability gene Kirrel3 regulates target-specific mossy fiber synapse development in the hippocampus E Anne Martin1†, Shruti Muralidhar1†, Zhirong Wang1, Die´ go Cordero Cervantes1, Raunak Basu1, Matthew R Taylor1, Jennifer Hunter1, Tyler Cutforth2, Scott A Wilke3, Anirvan Ghosh4, Megan E Williams1* 1Department of Neurobiology and Anatomy, University of Utah School of Medicine, Salt Lake City, United States; 2Department of Neurology, Columbia University, New York City, United States; 3Neurobiology Section, Division of Biological Sciences, University of California, San Diego, San Diego, United States; 4Neuroscience Discovery, Roche Innovation Center Basel, F. Hoffmann-La Roche, Basel, Switzerland Abstract Synaptic target specificity, whereby neurons make distinct types of synapses with different target cells, is critical for brain function, yet the mechanisms driving it are poorly understood. In this study, we demonstrate Kirrel3 regulates target-specific synapse formation at hippocampal mossy fiber (MF) synapses, which connect dentate granule (DG) neurons to both CA3 and GABAergic neurons. Here, we show Kirrel3 is required for formation of MF filopodia; the structures that give rise to DG-GABA synapses and that regulate feed-forward inhibition of CA3 neurons. Consequently, loss of Kirrel3 robustly increases CA3 neuron activity in developing mice. Alterations in the Kirrel3 gene are repeatedly associated with intellectual disabilities, but the role of *For correspondence: megan. Kirrel3 at synapses remained largely unknown. Our findings demonstrate that subtle synaptic [email protected] changes during development impact circuit function and provide the first insight toward understanding the cellular basis of Kirrel3-dependent neurodevelopmental disorders. † These authors contributed DOI: 10.7554/eLife.09395.001 equally to this work Competing interests: The authors declare that no competing interests exist. -

Supplementary Figure 1. Western Blot Analysis of Total Nephrin Protein Levels in Glomeruli Isolated from Kidneys of Newborn
Supplementary Figure 1. Western Blot analysis of total Nephrin protein levels in glomeruli isolated from kidneys of newborn CRE[+];NOTCH-IC mice and control littermates. (A) Shown are Western Blot images for Nephrin (upper panel), WT1 (middle panel), and ACTIN (lower panel) in glomerular lysates from three CRE[-];NOTCH-IC (lanes 1-3) and four CRE[+];NOTCH-IC (lanes 4-8) newborn mice. Lysates were prepared from glomeruli isolated from newborn mouse kidneys by iron oxide perfusion followed by magnetic separation. Lysates were separated by SDS-PAGE, transferred onto PVDF membrane, and probed with anti-Nephrin to detect total Nephrin. Membranes were stripped and re-probed with anti-WT to detect WT1 protein, which was used as a surrogate measure of podocyte number to control for sample bias. Membranes were stripped a third time and re-probed with anti-Actin to detect Actin as a loading control. The leftmost lane depicts molecular weight standards. (B) Graphic representation of Nephrin (upper panel) and WT1 (lower panel) protein levels as determined semi-quantitatively by band densitometry. Band density was measured using image analysis software. Values for each lane were normalized to band density for corresponding actin loading control and expressed in arbitrary units (pixel number). White bars depict the mean value of measurements from three CRE[-];NOTCH-IC mice. Black bars show the mean measurement from four CRE[+];NOTCH- IC mice. Error bars denote S.E. (upper panel) No significant difference in total Nephrin protein levels was detected in glomerular lysates from CRE[+];NOTCH-IC mice compared to CRE[- ];NOTCH-IC controls. -

Nuclear Relocation of the Nephrin and CD2AP-Binding Protein Dendrin Promotes Apoptosis of Podocytes
Nuclear relocation of the nephrin and CD2AP-binding protein dendrin promotes apoptosis of podocytes Katsuhiko Asanuma*, Kirk Nicholas Campbell, Kwanghee Kim, Christian Faul, and Peter Mundel† Department of Medicine, Mount Sinai School of Medicine, New York, NY 10029 Edited by Marilyn Gist Farquhar, University of California at San Diego School of Medicine, La Jolla, CA, and approved April 28, 2007 (received for review February 1, 2007) Kidney podocytes and their slit diaphragms (SDs) form the final Results barrier to urinary protein loss. There is mounting evidence that SD Dendrin Is a Component of the SD Complex. Dendrin contains two proteins also participate in intracellular signaling pathways. The SD putative nuclear localization signals (NLSs) and three PPXY protein nephrin serves as a component of a signaling complex that motifs that are preserved among human, rat, and mouse (Fig. directly links podocyte junctional integrity to actin cytoskeletal 1a). To explore the renal expression of dendrin, we generated dynamics. Another SD protein, CD2-associated protein (CD2AP), is and affinity-purified a peptide antibody against the C terminus an adaptor molecule involved in podocyte homeostasis that can of mouse dendrin. This antibody detected the previously de- repress proapoptotic TGF- signaling in podocytes. Here we show scribed 89-kDa and 81-kDa isoforms of dendrin in the brain but that dendrin, a protein originally identified in telencephalic den- only the 81-kDa isoform in isolated glomeruli (Fig. 1b). By drites, is a constituent of the SD complex, where it directly binds immunofluorescence microscopy of adult mouse kidney, dendrin to nephrin and CD2AP. In experimental glomerulonephritis, den- was detected exclusively in glomeruli (Fig. -

Comparative Promoter Analysis Allows De Novo Identification of Specialized Cell Junction-Associated Proteins
Comparative promoter analysis allows de novo identification of specialized cell junction-associated proteins Clemens D. Cohen*, Andreas Klingenhoff†, Anissa Boucherot*, Almut Nitsche‡, Anna Henger*§, Bodo Brunner‡, Holger Schmid*, Monika Merkle*, Moin A. Saleem¶, Klaus-Peter Koller‡, Thomas Werner†, Hermann-Josef Gro¨ neʈ, Peter J. Nelson*,**, and Matthias Kretzler*§ *Medizinische Poliklinik, University of Munich, 80336 Munich, Germany; †Genomatix GmbH, 80335 Munich, Germany; ‡Sanofi-Aventis, 65926 Frankfurt, Germany; ¶Children’s Renal Unit, University of Bristol, Bristol BS10 5NB, United Kingdom; and ʈCellular and Molecular Pathology, German Cancer Research Center, 69120 Heidelberg, Germany Edited by Mark T. Groudine, Fred Hutchinson Cancer Research Center, Seattle, WA, and approved February 8, 2006 (received for review December 28, 2005) Shared transcription factor binding sites that are conserved in could also be used in bioinformatic analyses to detect genes distance and orientation help control the expression of gene heretofore not associated with the specific biologic process (5). products that act together in the same biological context. New To test these hypotheses, a unique tissue environment linked to bioinformatics approaches allow the rapid characterization of a specific biologic function was selected for a bioinformatic-driven shared promoter structures and can be used to find novel inter- analysis of promoter coregulation as outlined in Fig. 1. Glomerular acting molecules. Here, these principles are demonstrated by using epithelial cells, also referred to as podocytes, cover the fenestrated molecules linked to the unique functional unit of the glomerular capillaries of renal glomeruli in vertebrates and contribute to the slit diaphragm. An evolutionarily conserved promoter model was kidney filtration barrier (8). Podocytes have a complex phenotype generated by comparative genomics in the proximal promoter with interdigitating foot processes that are bridged by the final regions of the slit diaphragm-associated molecule nephrin. -

Kirrel3-Mediated Synapse Formation Is Attenuated by Disease-Associated Missense Variants 3 Abbreviated Title: Kirrel3 Variants Impair Its Function 4 5 Matthew R
bioRxiv preprint doi: https://doi.org/10.1101/2019.12.30.891085; this version posted December 30, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. 1 2 Kirrel3-mediated synapse formation is attenuated by disease-associated missense variants 3 Abbreviated Title: Kirrel3 variants impair its function 4 5 Matthew R. Taylor1*, E. Anne Martin1*, Brooke Sinnen1, Rajdeep Trilokekar1, Emmanuelle Ranza2,3, 6 Stylianos E. Antonarakis2,4, Megan E. Williams1 7 8 1Department of Neurobiology and Anatomy, University of Utah School of Medicine, Salt Lake City, UT 9 84112, USA 10 2Service of Genetic Medicine, Geneva University Hospitals, Geneva, Switzerland 11 3Current address: Medigenome, Swiss Institute of Genomic Medicine, Geneva, Switzerland 12 4Department of Genetic Medicine and Development, University of Geneva Medical Faculty, Geneva, 13 Switzerland 14 * These authors contributed equally to this work 15 16 Correspondence should be addressed to Megan E. Williams at [email protected]. 17 18 Number of pages: 37 19 Number of figures: 6 20 Number of tables: 1 21 Abstract word count: 209 22 Introduction word count: 728 23 Discussion word count: 1562 24 25 Conflict of Interest Statement: The authors declare no competing financial interests. 26 27 Acknowledgements: This work was supported by grants from the National Institute of Mental Health 28 (R01 MH105426, M.E.W), Brain Research Foundation Fay/Frank Seed Grant (M.E.W), Childcare 29 Foundation (S.E.A), and an Autism Speaks Dennis Weatherstone Predoctoral Fellowship 10116 (E.A.M).