Glucagon and Amino Acids Are Linked in a Mutual Feedback Cycle: the Liver–A-Cell Axis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Unrestricted Immigration and the Foreign Dominance Of
Unrestricted Immigration and the Foreign Dominance of United States Nobel Prize Winners in Science: Irrefutable Data and Exemplary Family Narratives—Backup Data and Information Andrew A. Beveridge, Queens and Graduate Center CUNY and Social Explorer, Inc. Lynn Caporale, Strategic Scientific Advisor and Author The following slides were presented at the recent meeting of the American Association for the Advancement of Science. This project and paper is an outgrowth of that session, and will combine qualitative data on Nobel Prize Winners family histories along with analyses of the pattern of Nobel Winners. The first set of slides show some of the patterns so far found, and will be augmented for the formal paper. The second set of slides shows some examples of the Nobel families. The authors a developing a systematic data base of Nobel Winners (mainly US), their careers and their family histories. This turned out to be much more challenging than expected, since many winners do not emphasize their family origins in their own biographies or autobiographies or other commentary. Dr. Caporale has reached out to some laureates or their families to elicit that information. We plan to systematically compare the laureates to the population in the US at large, including immigrants and non‐immigrants at various periods. Outline of Presentation • A preliminary examination of the 609 Nobel Prize Winners, 291 of whom were at an American Institution when they received the Nobel in physics, chemistry or physiology and medicine • Will look at patterns of -

Further Evidence That G Proteins Are Multimeric And
Proc. Natl. Acad. Sci. USA Vol. 90, pp. 8782-8786, October 1993 Biochemistry The disaggregation theory of signal transduction revisited: Further evidence that G proteins are multimeric and disaggregate to monomers when activated SALEEM JAHANGEER AND MARTIN RODBELL Signal Transduction Section, Laboratory of Ceilular and Molecular Pharmacology, National Institute of Environmental Health Sciences, Research Triangle Park, NC 27709 Contributed by Martin Rodbell, May 27, 1993 ABSTRACT We have compared the sin on rates and those found in detergent extracts. Based on target on sucrose gradients of the heterotrhimeric GTP-binding regu- analysis, G proteins in the native membrane environment are latory (G) proteins G., Go, G,, and Gq etracted from rat brain thought to be higher-ordered structures, termed multimers, synaptoneurosomes with Lubrol and digtin. The individual that are converted to monomers by the combined actions of a and 3 subunits were monitored with specifi antisera. In all hormones and guanine nucleotides (4). Further support for cases, both subunits cosedimete dicatg that the subunits this hypothesis stems from recent findings that the major are likely complexed as heterotrimers. When extracted with heterotrimeric G proteins in rat brain synaptoneurosomes are Lubrol al of the G proteins s ted with rates of about 4.5 cross-linked in their native membrane environment, yielding S (condstent with heterotrimers) whereas diitonin extae very large structures compatible with their being multimeric 60% ofthe G proteins with peaksat 11 S; 40% pefleted aslager proteins (5). Different structures of G proteins and their structure. Dgtonin-extae G, was cross-linked by p-phe- products ofhormone and guanine nucleotide activation have nyle imaide, yielding structures too large to enter poly- also been obtained, depending on the types of detergents acrlamide gels. -

Federation Member Society Nobel Laureates
FEDERATION MEMBER SOCIETY NOBEL LAUREATES For achievements in Chemistry, Physiology/Medicine, and PHysics. Award Winners announced annually in October. Awards presented on December 10th, the anniversary of Nobel’s death. (-H represents Honorary member, -R represents Retired member) # YEAR AWARD NAME AND SOCIETY DOB DECEASED 1 1904 PM Ivan Petrovich Pavlov (APS-H) 09/14/1849 02/27/1936 for work on the physiology of digestion, through which knowledge on vital aspects of the subject has been transformed and enlarged. 2 1912 PM Alexis Carrel (APS/ASIP) 06/28/1873 01/05/1944 for work on vascular suture and the transplantation of blood vessels and organs 3 1919 PM Jules Bordet (AAI-H) 06/13/1870 04/06/1961 for discoveries relating to immunity 4 1920 PM August Krogh (APS-H) 11/15/1874 09/13/1949 (Schack August Steenberger Krogh) for discovery of the capillary motor regulating mechanism 5 1922 PM A. V. Hill (APS-H) 09/26/1886 06/03/1977 Sir Archibald Vivial Hill for discovery relating to the production of heat in the muscle 6 1922 PM Otto Meyerhof (ASBMB) 04/12/1884 10/07/1951 (Otto Fritz Meyerhof) for discovery of the fixed relationship between the consumption of oxygen and the metabolism of lactic acid in the muscle 7 1923 PM Frederick Grant Banting (ASPET) 11/14/1891 02/21/1941 for the discovery of insulin 8 1923 PM John J.R. Macleod (APS) 09/08/1876 03/16/1935 (John James Richard Macleod) for the discovery of insulin 9 1926 C Theodor Svedberg (ASBMB-H) 08/30/1884 02/26/1971 for work on disperse systems 10 1930 PM Karl Landsteiner (ASIP/AAI) 06/14/1868 06/26/1943 for discovery of human blood groups 11 1931 PM Otto Heinrich Warburg (ASBMB-H) 10/08/1883 08/03/1970 for discovery of the nature and mode of action of the respiratory enzyme 12 1932 PM Lord Edgar D. -

Close to the Edge: Co-Authorship Proximity of Nobel Laureates in Physiology Or Medicine, 1991 - 2010, to Cross-Disciplinary Brokers
Close to the edge: Co-authorship proximity of Nobel laureates in Physiology or Medicine, 1991 - 2010, to cross-disciplinary brokers Chris Fields 528 Zinnia Court Sonoma, CA 95476 USA fi[email protected] January 2, 2015 Abstract Between 1991 and 2010, 45 scientists were honored with Nobel prizes in Physiology or Medicine. It is shown that these 45 Nobel laureates are separated, on average, by at most 2.8 co-authorship steps from at least one cross-disciplinary broker, defined as a researcher who has published co-authored papers both in some biomedical discipline and in some non-biomedical discipline. If Nobel laureates in Physiology or Medicine and their immediate collaborators can be regarded as forming the intuitive “center” of the biomedical sciences, then at least for this 20-year sample of Nobel laureates, the center of the biomedical sciences within the co-authorship graph of all of the sciences is closer to the edges of multiple non-biomedical disciplines than typical biomedical researchers are to each other. Keywords: Biomedicine; Co-authorship graphs; Cross-disciplinary brokerage; Graph cen- trality; Preferential attachment Running head: Proximity of Nobel laureates to cross-disciplinary brokers 1 1 Introduction It is intuitively tempting to visualize scientific disciplines as spheres, with highly produc- tive, well-funded intellectual and political leaders such as Nobel laureates occupying their centers and less productive, less well-funded researchers being increasingly peripheral. As preferential attachment mechanisms as well as the economics of employment tend to give the well-known and well-funded more collaborators than the less well-known and less well- funded (e.g. -
Nobel Laureates in Physiology Or Medicine
All Nobel Laureates in Physiology or Medicine 1901 Emil A. von Behring Germany ”for his work on serum therapy, especially its application against diphtheria, by which he has opened a new road in the domain of medical science and thereby placed in the hands of the physician a victorious weapon against illness and deaths” 1902 Sir Ronald Ross Great Britain ”for his work on malaria, by which he has shown how it enters the organism and thereby has laid the foundation for successful research on this disease and methods of combating it” 1903 Niels R. Finsen Denmark ”in recognition of his contribution to the treatment of diseases, especially lupus vulgaris, with concentrated light radiation, whereby he has opened a new avenue for medical science” 1904 Ivan P. Pavlov Russia ”in recognition of his work on the physiology of digestion, through which knowledge on vital aspects of the subject has been transformed and enlarged” 1905 Robert Koch Germany ”for his investigations and discoveries in relation to tuberculosis” 1906 Camillo Golgi Italy "in recognition of their work on the structure of the nervous system" Santiago Ramon y Cajal Spain 1907 Charles L. A. Laveran France "in recognition of his work on the role played by protozoa in causing diseases" 1908 Paul Ehrlich Germany "in recognition of their work on immunity" Elie Metchniko France 1909 Emil Theodor Kocher Switzerland "for his work on the physiology, pathology and surgery of the thyroid gland" 1910 Albrecht Kossel Germany "in recognition of the contributions to our knowledge of cell chemistry made through his work on proteins, including the nucleic substances" 1911 Allvar Gullstrand Sweden "for his work on the dioptrics of the eye" 1912 Alexis Carrel France "in recognition of his work on vascular suture and the transplantation of blood vessels and organs" 1913 Charles R. -
Nobel Laureates Published In
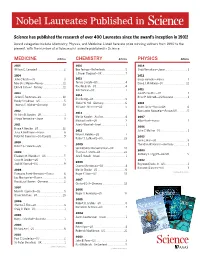
Nobel Laureates Published in Science has published the research of over 400 Laureates since the award’s inception in 1901! Award categories include Chemistry, Physics, and Medicine. Listed here are prize-winning authors from 1990 to the present, with the number of articles each Laureate published in Science. MEDICINE Articles CHEMISTRY Articles PHYSICS Articles 2015 2016 2014 William C. Campbell . 2 Ben Feringa —Netherlands........................5 Shuji Namakura—Japan .......................... 1 J. Fraser Stoddart—UK . 7 2014 2012 John O’Keefe—US...................................3 2015 Serge Haroche—France . 1 May-Britt Moser—Norway .......................11 Tomas Lindahl—US .................................4 David J. Wineland—US ............................12 Edvard I. Moser—Norway ........................11 Paul Modrich—US...................................4 Aziz Sancar—US.....................................7 2011 2013 Saul Perlmutter—US ............................... 1 2014 James E. Rothman—US ......................... 10 Brian P. Schmidt—US/Australia ................. 1 Eric Betzig—US ......................................9 Randy Schekman—US.............................5 Stefan W. Hell—Germany..........................6 2010 Thomas C. Südhof—Germany ..................13 William E. Moerner—US ...........................5 Andre Geim—Russia/UK..........................6 2012 Konstantin Novoselov—Russia/UK ............5 2013 Sir John B. Gurdon—UK . 1 Martin Karplas—Austria...........................4 2007 Shinya Yamanaka—Japan.........................3 -

Advances in the Field of Endocrinology: a Demographic Analysis
Advances in the Field of Endocrinology: A Demographic Analysis A Research Thesis Presented to The Faculty of the Biology Department Adelphi University By Pari Waghela In Partial Fulfillment of the Requirements for the M.S. Degree in Biology Date: 1/14/2021 Advisor: Dr. Tandra Chakraborty Thesis Committee: Dr. Andrea Ward Dr. Deborah Cooperstein Acknowledgement I want to express my gratitude to my thesis advisor, Dr. Tandra Chakraborty, Chair and Professor of the Biology Department of Adelphi University. The doors of her office were always open whenever I had doubts and queries regarding the thesis and the courses that I found extremely difficult to understand. Her vision, motivation, and faith in my work deeply inspired me. She has always guided me to the right path of my career, and this would not be possible without her guidance and support. I am extremely grateful for the opportunity offered to me. I would also like to thank my committee members, Dr. Andrea Ward, Associate Dean for Student Success Strategic Initiatives, Adelphi University and Dr. Deborah Cooperstein, Professor at Biology, College of Arts and Sciences and Vice President for Collective Bargaining American Association of University Professors, Adelphi Chapter, Adelphi University. I have gratefully indebted them to her for their precious comments on this thesis. I am extremely grateful to my parents, Rakesh Waghela (Father) and Mittal Waghela (Mother), for their love, prayers, and sacrifices to educate and prepare me for my future. I am very much thankful to Pratham Waghela (brother), for understanding and support me throughout my education. This accomplishment would not have been possible without them. -

Nobel Laureates Published In
Nobel Laureates Published in Science has published articles by Nobel Prize® Laureates since the award’s inception! Award categories include Chemistry, Physics, and Medicine. Listed here are prize winning authors from 1990 to the present, with the number of articles each laureate published in Science. Science is considered one of the world’s most prestigious scientific journals and is published by the American Association for the Advancement of Science (AAAS). CHEMISTRY MEDICINE Physics 2009 2009 2007 Venkatraman Ramakrishnan—UK ............10 Elizabeth H. Blackburn—US ................................6 Albert Fert—France ...............................................1 Thomas A. Steitz—US ............................................28 Carol W. Greider—US ..................................................1 Ada E. Yonath—Israel ..................................................1 Jack W. Szostak—US ...................................................9 2006 John C. Mather—US ............................................1 2008 2008 Osamu Shimomura—US ........................................7 Françoise Barré-Sinnoussi—Germany ........6 2005 Martin Chalfie—US .......................................................6 Luc Montagnier—France .....................................11 John L. Hall—US .....................................................3 Roger Y. Tsien—US ...................................................14 Harald zur Hausen—France ...................................2 Theodore W. Hänsch—Germany ................2 2007 2007 2004 Gerhard Ertl—Germany -

List of Nobel Laureates 1
List of Nobel laureates 1 List of Nobel laureates The Nobel Prizes (Swedish: Nobelpriset, Norwegian: Nobelprisen) are awarded annually by the Royal Swedish Academy of Sciences, the Swedish Academy, the Karolinska Institute, and the Norwegian Nobel Committee to individuals and organizations who make outstanding contributions in the fields of chemistry, physics, literature, peace, and physiology or medicine.[1] They were established by the 1895 will of Alfred Nobel, which dictates that the awards should be administered by the Nobel Foundation. Another prize, the Nobel Memorial Prize in Economic Sciences, was established in 1968 by the Sveriges Riksbank, the central bank of Sweden, for contributors to the field of economics.[2] Each prize is awarded by a separate committee; the Royal Swedish Academy of Sciences awards the Prizes in Physics, Chemistry, and Economics, the Karolinska Institute awards the Prize in Physiology or Medicine, and the Norwegian Nobel Committee awards the Prize in Peace.[3] Each recipient receives a medal, a diploma and a monetary award that has varied throughout the years.[2] In 1901, the recipients of the first Nobel Prizes were given 150,782 SEK, which is equal to 7,731,004 SEK in December 2007. In 2008, the winners were awarded a prize amount of 10,000,000 SEK.[4] The awards are presented in Stockholm in an annual ceremony on December 10, the anniversary of Nobel's death.[5] As of 2011, 826 individuals and 20 organizations have been awarded a Nobel Prize, including 69 winners of the Nobel Memorial Prize in Economic Sciences.[6] Four Nobel laureates were not permitted by their governments to accept the Nobel Prize. -

Conceptual Evolution of Cell Signaling
International Journal of Molecular Sciences Review Conceptual Evolution of Cell Signaling 1, 1, 1, 2, Arathi Nair y , Prashant Chauhan y , Bhaskar Saha * and Katharina F. Kubatzky * 1 National Center for Cell Science (NCCS), Ganeshkhind, Pune 411007, India 2 Zentrum für Infektiologie, Medizinische Mikrobiologie und Hygiene, Universitätsklinikum Heidelberg, Im Neuenheimer Feld 324, 69120 Heidelberg, Germany * Correspondence: [email protected] (B.S.); [email protected] (K.F.K.) Indicates Equal Contribution. y Received: 11 April 2019; Accepted: 28 June 2019; Published: 4 July 2019 Abstract: During the last 100 years, cell signaling has evolved into a common mechanism for most physiological processes across systems. Although the majority of cell signaling principles were initially derived from hormonal studies, its exponential growth has been supported by interdisciplinary inputs, e.g., from physics, chemistry, mathematics, statistics, and computational fields. As a result, cell signaling has grown out of scope for any general review. Here, we review how the messages are transferred from the first messenger (the ligand) to the receptor, and then decoded with the help of cascades of second messengers (kinases, phosphatases, GTPases, ions, and small molecules such as cAMP, cGMP, diacylglycerol, etc.). The message is thus relayed from the membrane to the nucleus where gene expression ns, subsequent translations, and protein targeting to the cell membrane and other organelles are triggered. Although there are limited numbers of intracellular messengers, the specificity of the response profiles to the ligands is generated by the involvement of a combination of selected intracellular signaling intermediates. Other crucial parameters in cell signaling are its directionality and distribution of signaling strengths in different pathways that may crosstalk to adjust the amplitude and quality of the final effector output. -

Image-Brochure-LNLM-2020-LQ.Pdf
NOBEL LAUREATES PARTICIPATING IN LINDAU EVENTS SINCE 1951 Peter Agre | George A. Akerlof | Kurt Alder | Zhores I. Alferov | Hannes Alfvén | Sidney Altman | Hiroshi Amano | Philip W. Anderson | Christian B. Anfinsen | Edward V. Appleton | Werner Arber | Frances H. Arnold | Robert J. Aumann | Julius Axelrod | Abhijit Banerjee | John Bardeen | Barry C. Barish | Françoise Barré-Sinoussi | Derek H. R. Barton | Nicolay G. Basov | George W. Beadle | J. Georg Bednorz | Georg von Békésy |Eric Betzig | Bruce A. Beutler | Gerd Binnig | J. Michael Bishop | James W. Black | Elizabeth H. Blackburn | Patrick M. S. Blackett | Günter Blobel | Konrad Bloch | Felix Bloch | Nicolaas Bloembergen | Baruch S. Blumberg | Niels Bohr | Max Born | Paul Boyer | William Lawrence Bragg | Willy Brandt | Walter H. Brattain | Bertram N. Brockhouse | Herbert C. Brown | James M. Buchanan Jr. | Frank Burnet | Adolf F. Butenandt | Melvin Calvin Thomas R. Cech | Martin Chalfie | Subrahmanyan Chandrasekhar | Pavel A. Cherenkov | Steven Chu | Aaron Ciechanover | Albert Claude | John Cockcroft | Claude Cohen- Tannoudji | Leon N. Cooper | Carl Cori | Allan M. Cormack | John Cornforth André F. Cournand | Francis Crick | James Cronin | Paul J. Crutzen | Robert F. Curl Jr. | Henrik Dam | Jean Dausset | Angus S. Deaton | Gérard Debreu | Petrus Debye | Hans G. Dehmelt | Johann Deisenhofer Peter A. Diamond | Paul A. M. Dirac | Peter C. Doherty | Gerhard Domagk | Esther Duflo | Renato Dulbecco | Christian de Duve John Eccles | Gerald M. Edelman | Manfred Eigen | Gertrude B. Elion | Robert F. Engle III | François Englert | Richard R. Ernst Gerhard Ertl | Leo Esaki | Ulf von Euler | Hans von Euler- Chelpin | Martin J. Evans | John B. Fenn | Bernard L. Feringa Albert Fert | Ernst O. Fischer | Edmond H. Fischer | Val Fitch | Paul J. -

24 August 2013 Seminar Held
PROCEEDINGS OF THE NOBEL PRIZE SEMINAR 2012 (NPS 2012) 0 Organized by School of Chemistry Editor: Dr. Nabakrushna Behera Lecturer, School of Chemistry, S.U. (E-mail: [email protected]) 24 August 2013 Seminar Held Sambalpur University Jyoti Vihar-768 019 Odisha Organizing Secretary: Dr. N. K. Behera, School of Chemistry, S.U., Jyoti Vihar, 768 019, Odisha. Dr. S. C. Jamir Governor, Odisha Raj Bhawan Bhubaneswar-751 008 August 13, 2013 EMSSSEM I am glad to know that the School of Chemistry, Sambalpur University, like previous years is organizing a Seminar on "Nobel Prize" on August 24, 2013. The Nobel Prize instituted on the lines of its mentor and founder Alfred Nobel's last will to establish a series of prizes for those who confer the “greatest benefit on mankind’ is widely regarded as the most coveted international award given in recognition to excellent work done in the fields of Physics, Chemistry, Physiology or Medicine, Literature, and Peace. The Prize since its introduction in 1901 has a very impressive list of winners and each of them has their own story of success. It is heartening that a seminar is being organized annually focusing on the Nobel Prize winning work of the Nobel laureates of that particular year. The initiative is indeed laudable as it will help teachers as well as students a lot in knowing more about the works of illustrious recipients and drawing inspiration to excel and work for the betterment of mankind. I am sure the proceeding to be brought out on the occasion will be highly enlightening.