Newsletter May 2016
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparison of ABTS, DPPH, and FRAP Assays for Estimating Antioxidant Potential of Selected Sri Lankan Traditional Sweetmeats
Comparison of ABTS, DPPH, and FRAP Assays for Estimating Antioxidant Potential of Selected Sri Lankan Traditional Sweetmeats M.K.S. Mihiranie1, J.M.J.K. Jayasinghe1, J.P.D. Wanasundara3 and C.V.L. Jayasinghe2 1Department of Food Science and Technology, University of Sri Jayewardenepura, Nugegoda, Sri Lanka 2Department of Food Science and Technology, Wayamba University of Sri Lanka, Gonawila, Sri Lanka 3College of Graduate Studies and Research, University of Saskatchewan, Saskatchewan, Canada Fifteen Sri Lankan traditional sweetmeats (Hendi kewum, Beraliya kewum, Naran kewum, Athirasa, Mung kewum, Aasmi, Kokis, Undu walalu, Welithalapa, Bedihaalpiti aggala, Dodol, Aluwa, Thala guli, Kurahan helapa and Pusnambu) were investigated for antioxidant potential (AP) by 2,2-diphenyl-1- picrylhydrazyl assay (DPPH), 2,2-azino- bis-3-ethylbenzothiazoline-6-sulphonic acid (ABTS) assay and Ferrous reducing antioxidant power assay (FRAP). Total phenolic content (TPC) and total flavonoid content (TFC) of sweetmeats were determined by using colorimetric assays. Lyophilized sweetmeats (1:10) were used to prepare 80% methanolic extractions at room temperature for 24 hours for all the assays. Helapa was further investigated for the changes in AP with the changes of ingredients utilized in different regions of Sri Lanka. Accordingly, Helapa prepared with 100% finger millet flour, finger millet+rice flour, Shorea megistophylla (sin. Beraliya) flour+rice flour, Vateria copallifera (sin. Hal) flour+rice flour, Madhuca longifolia (sin. Mee) flour+rice flour was studied. Results revealed that, among sweetmeats examined for AP, Naran Kewum showed the significantly highest AP (1595.7±0.03 µg/mL TE) by FRAP assay and Helapa showed the highest radical scavenging activity for DPPH (564.8± 0.02 µg/mL TE) and ABTS (553.2±0.01 µg/mL TE) assays (p<0.05). -

Features White Flour and Are at High Risk for Dia- Betes
10 Wednesday 27th October, 2010 The Island Features white flour and are at high risk for dia- betes. If you can't handle the taste of natural garlic, you can take it in widely available supplements. Aloe vera [Komarika] is also a traditional diabetic remedy in the Unani system of Arabian medicine, and its thera- peutic characteristics are now gaining worldwide acceptance in the treatment of diabetes. According to both human and animal research studies, aloe vera lowers blood glucose levels by a mechanism that’s still unclear to researchers. According to the Clinicians Handbook of Natural Healing, this natural hypoglycemic effect extends to over a period of 24 hours. Adding onions to your diet (along with gar- lic and cinnamon) can also significantly reduce your blood sugar level. Additionally, according to the book: The Healing Power of Herbs, studies have demonstrated that ginseng controls blood glucose in both dia- betic humans and diabetic laboratory ani- mals. It all comes down to asking if putting yourself at risk for diabetic coma, blind- ness, limb amputation and death is it worth eating white bread. If you're willing to risk your quality-of-life and your life itself, then go ahead and eat all the foods made with refined white flour you want. However, if you want to stop poisoning yourself with alloxan, a known toxic chem- ical, then make a few simple dietary changes. Eat groceries made with whole- grain wheat flour and other acceptable and more nutritious substitutes, not processed wheat (white) flour. What you have read so far are the unvar- nished facts about the effects of eating refined wheat (white) flour products, the most common and widespread of which is bread. -

Food Consumption Patterns in Sri Lanka
Food Consumption Patterns in Sri Lanka R.L.N. Jayatissa W.D. Wickramasinghe Chandrani Piyasena Research Report No: 172 September 2014 Hector Kobbekaduwa Agrarian Research and Training Institute 114, Wijerama Mawatha Colombo 7 Sri Lanka I First Published: September 2014 © 2014, Hector Kobbekaduwa Agrarian Research and Training Institute Coverpage Designed by: Udeni Karunaratne Final typesetting and lay-out by: Dilanthi Hewavitharana ISBN: 978-955-612-172-8 II FOREWORD The patterns of food consumption vary from time to time, according to various ethnic groups living in the country. Their culture, job category, income and internal migration situation are other factors affecting food consumption. In the British era, cheap labour was brought for the plantation industry from South India. Initially the British introduced bread and wheat flour based foods as their main food. Gradually, the consumption of wheat and wheat based food became popular in the country. But during the era of our ancient kings, consumption of traditional food varieties was the norm. Due to high nutritious value of our local food items our ancestors were healthy. After gaining Independence, successive governments paid attention to infrastructure facilities to uplift local agriculture. Some of them were Mahaweli Development Programme, Ama Programme (1995-2000) and the Api wawamu - rata nagamu progrmme (2007-2010). It is highly important to conduct research into rural, urban and estate sectors’ dietary habits to ascertain whether they are taking a nutritious diet. Although Sri Lanka is rich in many healthy foods like jak, breadfruit, domestic tuber roots, pulses, legumes and fruits, people are not concerned about these food items thus, those foods are wasted considerably. -

Sri Lanka Journal of Food and Agriculture (SLJFA)
Sri Lanka Journal of Food and Agriculture 3(1): 1-8, 2017 DOI: http://doi.org/10.4038/sljfa.v3i1.37 Sri Lanka Journal of Food and Agriculture (SLJFA) ISSN: 2424-6913 Journal homepage: www.slcarp.lk Research Paper Development of a pre-cooked supplementary food using Palmyrah tuber S. Piratheepan1, S. Sangheetha2, S. Srivijeindran3, O.D.A.N. Perera1 and C.V.L. Jayasinghe1* 1Department of Food Science and Technology, Faculty of Livestock, Fisheries and Nutrition, Wayamba University of Sri Lanka, Makandura, Gonawila (NWP), Sri Lanka 2Department of Food Technology, University College of Jaffna, Kokkuvil, Jaffna, Sri Lanka 2Palmyrah Research Institute, Kaithady, Jaffna, Sri Lanka *Corresponding Author: [email protected] __________________________________________________________________________________________________________________________________________ Article History: Abstract: Incorporation of legumes and tuber flours could improve the Received: 26 January 2017 protein quality and energy content of traditional supplementary foods Revised form received: 28 March 2017 prepared mainly from cereals such as maize and sorghum in the Accepted: 25 April 2017 developing countries. This study focused on developing a nutritious supplementary food using staple cereals, legumes and palmyrah tuber. “PalmyrahNutrimix” was formulated from the flour of cowpea, chickpea, sesame, green gram, soya bean and palmyrah tuber. Palmyrah tuber flour was obtained through tuber boiling, sun drying and milling process. Sugar and palmyrah tuber flour were optimized via 25 treatments. Sensory evaluation results revealed that three formulae consisting of sugar (19.4%) with different ratio of boiled and dried palmyrah tuber flour (15.9%, 18.2% and 20.3%) scored the highest mean rank sum (71.6), which complies with the Sri Lankan standards for energy (468.37 kcal/100g), protein (15.66%), fat (10.08%), fiber (4.75%) and carbohydrate (61.15%). -

Bali Rituals and Therapeutic Communication in the Traditional Rural Society in Sri Lanka*
Journalism and Mass Communication, November 2016, Vol. 6, No. 11, 679-699 doi: 10.17265/2160-6579/2016.11.003 D DAVID PUBLISHING Bali Rituals and Therapeutic Communication in the Traditional Rural Society in Sri Lanka* Manoj Jinadasa University of Kelaniya, Kelaniya, Sri Lanka Bali is a form of classical ritual that makes a sound performance of a variety of psychological and physical treatments for many psychiatric and cultural diseases. Bali is defined as a form of oblation for gods and deities. Bali is determined by the ephemeral cycle of one’s life, so that the procedures and practices of specific Bali performances are planned to communicate with the planetary system, which is based on his/her astrology. Hence, Bali is made to perform with the use of traditional dance, music and local cultural substances. There are nearly eighty four thousand forms of Bali performances derived out from the constellation. History of Bali goes back to the early kingdom of Kotte which started in early fifteen century. However, it is considered that the origin of Bali resembles with the Indian Hindu religious cults, so that the Sri Lankan Bali tradition has been transformed by the local cultural and Buddhist religious milieu. This study explores the content and effects of Bali ritual. As the qualitative research, it assumes that Bali constitutes a broad spectrum of human needs and wants despite its communication to the supernatural elements of planetary system. Sederaman (1965) has explored Bali to the extent of its entire performance with respective lyrics and dancing procedures, as the pioneering study. -
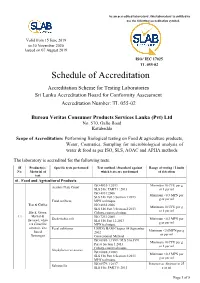
Schedule of Accreditation
As an accredited laboratory, this laboratory is entitled to use the following accreditation symbol. Valid from 15 June 2019 to 30 November 2020 Issued on 07 August 2019 ISO/ IEC 17025 TL 055-02 Schedule of Accreditation Accreditation Scheme for Testing Laboratories Sri Lanka Accreditation Board for Conformity Assessment Accreditation Number: TL 055-02 Bureau Veritas Consumer Products Services Lanka (Pvt) Ltd No. 570, Galle Road Katubedda Scope of Accreditation: Performing Biological testing on Food & agriculture products, Water, Cosmetics, Sampling for microbiological analysis of water & food as per ISO, SLS, AOAC and APHA methods The laboratory is accredited for the following tests. SI Product(s) / Specific tests performed Test method / Standard against Range of testing / Limits No. Material of which tests are performed of detection test 01. Food and Agricultural Products ISO 4833-1:2013 Minimum 10 CFU per g Aerobic Plate Count SLS 516: PART 1: 2013 or 1 per ml ISO 4831:2006 Minimum <0.3 MPN per SLS 516 Part 3 Section 1:2013 g or per ml Total coliform MPN technique Tea & Coffee ISO 4832:2006 Minimum 10 CFU per g SLS 516 Part 3 Section 2:2013 or 1 per ml Black, Green, Colony-count technique 1.1 Herbal & ISO 7251:2005 Escherichia coli Minimum <0.3 MPN per flavored, white SLS 516 Part 12:2013 g or per ml tea Camellia MPN technique sinensis, Tea Fecal coliforms USFDA BAM Chapter 04 September Minimum <3.0MPN per g based 2002 or per ml Beverages Conventional Method ISO 6888-1:1999 / SLS 516:1991 Minimum 10 CFU per g Part 6 Section 1:2013 or 1 per ml Colony-count technique Staphylococcus aureus ISO 6888-3:2003 Minimum <0.3 MPN per SLS 516 Part 6 Section 3:2013 g or per ml MPN technique ISO 6579-1:2017 Presence or Absence in 25 Salmonella SLS 516: PART 5: 2013 g or ml Page 1 of 8 SI Product(s) / Specific tests performed Test method / Standard against Range of testing / Limits No. -

In the Dry Zone of Sri Lanka
A PROPOSAL FOR DECLARATION AS A GIAHS THE CASCADED TANK-VILLAGE SYSTEM (CTVS) IN THE DRY ZONE OF SRI LANKA MINISTRY OF AGRICULTURE AND FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS, SRI LANKA MARCH 2017 TABLE OF CONTENTS ACRONYMS ............................................................................................................................. 5 SUMMARY INFORMATION .................................................................................................. 6 CHAPTER 1: INTRODUCTION TO THE PROPOSED GIAHS ............................................ 9 1.1 The Dry Zone ............................................................................................................ 10 1.2 Ancient Hydraulic Civilization of Sri Lanka ............................................................ 11 1.3 Traditional Agriculture in the Dry Zone ................................................................... 15 1.4 Irrigation Systems ..................................................................................................... 16 1.5 Traditional System of Water Management ............................................................... 18 1.6 Geographical Distribution of Village Tanks ............................................................. 20 1.7 The Cascaded Tank-Village System (CTVS) ........................................................... 22 1.8 Key Components of the System ................................................................................ 24 1.9 Production System.................................................................................................... -

Family Power in Governance of Family Businesses: Cases from Sri Lanka
ECOFORUM [Volume 7, Issue 1(14), 2018] FAMILY POWER IN GOVERNANCE OF FAMILY BUSINESSES: CASES FROM SRI LANKA Ravindra Hewa KURUPPUGE Tomas Bata University in Zlin, Czech Republic, [email protected] Athula EKANAYAKE University of Peradeniya, Sri Lanka Alexandru-Mircea NEDELEA Stefan cel Mare University of Suceava, Romania [email protected] Abstract Family businesses have been widely researched over the years. For instance, scholars attempted to distinguish family businesses over nonfamily businesses using many criteria. Although there is no commonly accepted such criteria to identify family businesses more specifically, family power has been identified as a key criterion to explain the governance of family businesses. Following qualitative research approach and undertaking four case studies this paper aims to explain the ways in which family power shapes the governance of family businesses. The existing literature suggests, among other things, that family ownership and their involvement in management contribute heavily on the governance of family businesses. The notions of agency and stewardship theories propose that family power could create positive outcomes such as minimizing agency costs between owners and managers. However, it can also form governance issues due to lack of professional management particularly when the organizations become larger. Data were gathered through interviews of directors, owner-managers, family-tied non-executive employees of the four family owned businesses, and analyzed in three interactive processes, namely data reduction, data display, and conclusion drawing and verification. The findings suggest that the ownership control influence differently on the governance of family owned businesses depending on whether the family business is single owned or multiple owned. -
Traditional Food & Beverages of Sri Lanka
Traditional Food & Beverages of Sri Lanka ll living beings live by food. The staple food of the Sri Lankan Prof. A. Nimal F. Perera ("Sabbesaththa aharatthika") is rice. Rice is obtained from the AIn. other words, food is paddy plant. Paddy was also known A. Nimhani K. Perera as "salee* in the past. Paddy essential for our existence. Wayamba University of included two broad categories; "Maa Moreover, the great sages of ancient Sri Lanka, Kutiyapitiya times [Hrishis) have declared that wee" and "EI wee". Various our disposition and qualities evidence points out that there had depend on the food that we take. been more than 1500 traditional Prof. E.R. Kalyani Perera Further, there are three categories paddy varieties. The rice prepared University of Peradeniya, of persons according to their food from these different paddy varieties Peradentya. preferences; the righteous and was diverse in taste, aroma and gentle " Sathvikas" prefer soft and their nutritional values. In addition delicious food, rough, nonchalant to rice, other grains containing sweetmeats, fish and meat. Curries and indulgent "Rajasikas" prefer carbohydrates, such as millet, ("maalu") were complementary for acidic, hot and spiced food, and the paspahun scrobicultatum ("amtf), com, lazy, less enthusiastic and less maize, barley, and eleusine coraoana the rice and hence it was known as intelligent "Thamasikas", savor ("kurakkan') were also used widely. "boJhmaaht (rice and curries). In the unclean and stale food. Green gram, cow pea, long beans, consumption of rice and curries, masurg, lentil, koJJu, and gingili were drinking of water ["bath pert) was Food and beverages and their essential capsular ["shimbf) grains also essential. -

FR Page 6.Qxd
Page 6 The Island Travel Wednesday 17th November, 2010 No show this week Friday’s show of Sri Thelme, Sabaragamuwa, and Lanka Tourism ‘ Feel Sri Salupaliya with one or two Lanka ’ will not be staged on creative dances 19 Friday November in view ‘Feel Sri Lanka ’ was of the celebrations. launched in Colombo by The next show will take tourism authorities every place following Friday 26 Friday which is a concert of November 2010 which please authentic traditional dances pass around. of Sri Lanka specially for The organisers are happy tourists, foreign delegates and to announce that the last expatriates. show had attracted over 70 ‘ For details and compli- Free Independent Travellers’ mentary tickets for special ( FITs) in addition to the guests , please contact Achini Diplomats, Expatriates and 0714880571, Kumudu Steak & Wine Buffet at Cinnamon Conference delegated. 0714880570, Hasanji 077 Lakeside The recital now consists 3627733, Nemanthi 071 9872028 Known for its star class cuisine, the next innovative food pro- with a superb recital of Wes, anf Gayan 077 2544 117 motion introduces a buffet of steaks and accompaniments from November 18th to 20th. Set upon the Terrace, an extension of Iconic traditions celebrated the hit restaurant 7 Degrees North that overlooks the pool, steaks will be grilled before guests by the hotel’s Chefs. You might wan- der “How can one enjoy a steak buffet? Isn’t that unheard of?” with a bang by MLH Well, Executive Chef Wasantha has made it possible so as to As Mount Lavinia Hotel’s theme for the tions of the hotel’s properties with the give you a taste of the many types of steaks you have been long- season is based on iconic traditions it is voices of Voice Print and Vocal Essence ing to try! A variety of tender steaks will be specially flown in from no wonder that the celebration of St. -

Final 40 Page Jan 2012.Qxd
VOL. 9 NO. 9 JULY 2012 www.civilsocietyonline.com `50 JJJaaaccckkkfffrrruuuiiittt bbbuuusssiiinnneeessssss HHHooowww sssrrriii LLLaaannnkkkaaa gggrrreeewww aaa ttthhhrrriiivvviiinnnggg aaagggrrrooo---iiinnnddduuussstttrrryyy ‘Shanghai canalS vs water tankS the buzz about buzzaria iS a foot Pages 8-9 Page 26 in the door’ vizag Steel waS warned great park, rare goat Pages 10-11 Pages 32-33 Dibakar Banerjee on his kind of cinema inSide a green office kiShwar on Surrogacy Pages 6-7 Pages 14-15 Pages 34-35 CoNTENTS READ U S. WE READ YO U. The jackfruit solution or inclusion to work there has to be prosperity. The Sri Lanka cover story this month shows how the simplest of initiatives can be driv - Fers of employment and put money in people’s pockets. Why can’t we cOVer stOrY look at Sri Lanka and Southeast Asian nations and do similar things for our farm sector? our cover is one of many stories we have done on the importance of jackFruit business fresh thinking in the search for economic growth. Big investments are Sri Lanka has raised a thriving agro-industry in jackfruit by needed, but can they ever be a substitute for enabling people to earn in training vendors, housewives and entrepreneurs in processing small robust ways with their immediate resources? The best growth we technologies. They now make a range of jackfruit products. 20 can hope for should be broadbased. It should involve letting small enter - prises come up by linking them to markets and helping them with Cover piCture By shree paDre finance and simple technologies. The humble and unglamorous jackfruit is a solution only to those who Jarawa buffer zone is in force . -

Consumer Awareness and Preference Towards Finger Millet in Sri Lanka
Asian Food Science Journal 18(3): 34-44, 2020; Article no.AFSJ.57104 ISSN: 2581-7752 Consumer Awareness and Preference towards Finger Millet in Sri Lanka Sooriya Arachchige Sachini Jayawardana1, Dineth Suharda Samarawickrama1, Jayanetti Koralalage Ramani Radhika Samarasekera1*, Gardhi Hettiarachchige Chamari Madhu Hettiarachchi2 and Mahavidanage Jaanaki Gooneratne1 1Industrial Technology Institute, No. 363, Bauddhaloka Mawatha, Colombo 07, Sri Lanka. 2Department of Chemistry, Faculty of Science, University of Colombo, Colombo 03, Sri Lanka. Authors’ contributions This work was carried out in collaboration among all authors. Authors SASJ and DSS designed the consumer survey and performed the statistical analysis. Author SASJ managed the literature searches and wrote the first draft of the manuscript. Author DSS revised the manuscript. Authors JKRRS, GHCMH and MJG supervised the research and revised the manuscript. All authors read and approved the final manuscript. Article Information DOI:10.9734/AFSJ/2020/v18i330220 Editor(s): (1) Dr. Uttara Singh, Panjab University, India. Reviewers: (1) Margarita Išoraitė, Vilniaus kolegija/University, Lithuania. (2) Adeyeye, Samuel Ayofemi Olalekan, Ton Duc Thang University, Vietnam. (3) Omar Mohammad Faleh Atrooz, Mutah University, Jordan. Complete Peer review History: http://www.sdiarticle4.com/review-history/57104 Received 10 March 2020 Accepted 16 May 2020 Original Research Article Published 14 October 2020 ABSTRACT Aim: This survey was conducted to evaluate Sri Lankans’ awareness and attitudes towards finger millet and preferences towards finger millet-based foods. Methodology: Pre-tested, self-administrated questionnaires were formulated in the three main languages used in Sri Lanka, namely Sinhala, English and Tamil. The questionnaires consisted of different sections to obtain data on respondents’ socio-demographic characteristics, health and food related lifestyles, attitudes towards finger millet and preferences towards finger millet-based food products.