Analysis of Health Care Utilization in Côte D'ivoire
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DIAGNOSTIC REVIEW of PUBLIC EXPENDITURE in the AGRICULTURAL SECTOR in CÔTE D’IVOIRE Public Disclosure Authorized Period 1999–2012
104089 Public Disclosure Authorized MINISTRY OF AGRICULTURE MINISTRY OF WATER RESOURCES AND FORESTS MINISTRY OF LIVESTOCK AND FISHERY RESOURCES DIAGNOSTIC REVIEW OF PUBLIC EXPENDITURE IN THE AGRICULTURAL SECTOR IN CÔTE D’IVOIRE Public Disclosure Authorized Period 1999–2012 Ismaël Ouédraogo, International Consultant Kama Berté, National Consultant Public Disclosure Authorized FINAL November 2014 Public Disclosure Authorized Table of Contents LIST OF FIGURES iii LIST OF TABLES iv ACRONYMS AND ABBREVIATIONS v EXECUTIVE SUMMARY 1 I. INTRODUCTION 16 Objectives of the APE Diagnostic Review ........................................................................................ 17 Methodology ...................................................................................................................................... 17 II. STRATEGIC CONTEXT OF THE DIAGNOSTIC REVIEW 19 National Strategic Context ................................................................................................................. 19 Sectoral Strategies .............................................................................................................................. 20 Institutional Framework ..................................................................................................................... 23 III. COFOG CLASSIFICATION AND THE AGRICULTURAL PUBLIC EXPENDITURE DATABASE 25 COFOG Classification for the Agricultural Sector ............................................................................ 25 The APE Database ............................................................................................................................ -

Monthly Humanitarian Report November 2011
Côte d’Ivoire Rapport Humanitaire Mensuel Novembre 2011 Côte d’Ivoire Monthly Humanitarian Report November 2011 www.unocha.org The mission of the United Nations Office for the Coordination of Humanitarian Affairs (OCHA) is to mobilize and coordinate effective and principled humanitarian action in partnership with national and international actors. Coordination Saves Lives • Celebrating 20 years of coordinated humanitarian action November 2011 Côte d’Ivoire Monthly Bulletin | 2 Côte d’Ivoire Monthly Humanitarian Report Coordination Saves Lives Coordination Saves Lives No. 2 | November 2011 HIGHLIGHTS Voluntary and spontaneous repatriation of Ivorian refugees from Liberia continues in Western Cote d’Ivoire. African Union (AU) delegation visited Duékoué, West of Côte d'Ivoire. Tripartite agreement signed in Lomé between Ivorian and Togolese Governments and the United Nations High Commission for Refugees (UNHCR). Voluntary return of internally displaced people from the Duekoue Catholic Church to their areas of origin. World Food Program (WFP) published the findings of the post-distribution survey carried out from 14 to 21 October among 240 beneficiaries in 20 villages along the Liberian border (Toulépleu, Zouan- Hounien and Bin-Houyé). Child Protection Cluster in collaboration with Save the Children and UNICEF published The Vulnerabilities, Violence and Serious violations of Child Rights report. The Special Representative of the UN Secretary General on Sexual Violence in Conflict, Mrs. Margot Wallström on a six day visit to Côte d'Ivoire. I. GENERAL CONTEXT No major incident has been reported in November except for the clashes that broke out on 1 November between ethnic Guéré people and a group of dozos (traditional hunters). -
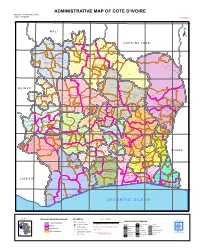
ADMINISTRATIVE MAP of COTE D'ivoire Map Nº: 01-000-June-2005 COTE D'ivoire 2Nd Edition
ADMINISTRATIVE MAP OF COTE D'IVOIRE Map Nº: 01-000-June-2005 COTE D'IVOIRE 2nd Edition 8°0'0"W 7°0'0"W 6°0'0"W 5°0'0"W 4°0'0"W 3°0'0"W 11°0'0"N 11°0'0"N M A L I Papara Débété ! !. Zanasso ! Diamankani ! TENGRELA [! ± San Koronani Kimbirila-Nord ! Toumoukoro Kanakono ! ! ! ! ! !. Ouelli Lomara Ouamélhoro Bolona ! ! Mahandiana-Sokourani Tienko ! ! B U R K I N A F A S O !. Kouban Bougou ! Blésségué ! Sokoro ! Niéllé Tahara Tiogo !. ! ! Katogo Mahalé ! ! ! Solognougo Ouara Diawala Tienny ! Tiorotiérié ! ! !. Kaouara Sananférédougou ! ! Sanhala Sandrégué Nambingué Goulia ! ! ! 10°0'0"N Tindara Minigan !. ! Kaloa !. ! M'Bengué N'dénou !. ! Ouangolodougou 10°0'0"N !. ! Tounvré Baya Fengolo ! ! Poungbé !. Kouto ! Samantiguila Kaniasso Monogo Nakélé ! ! Mamougoula ! !. !. ! Manadoun Kouroumba !.Gbon !.Kasséré Katiali ! ! ! !. Banankoro ! Landiougou Pitiengomon Doropo Dabadougou-Mafélé !. Kolia ! Tougbo Gogo ! Kimbirila Sud Nambonkaha ! ! ! ! Dembasso ! Tiasso DENGUELE REGION ! Samango ! SAVANES REGION ! ! Danoa Ngoloblasso Fononvogo ! Siansoba Taoura ! SODEFEL Varalé ! Nganon ! ! ! Madiani Niofouin Niofouin Gbéléban !. !. Village A Nyamoin !. Dabadougou Sinémentiali ! FERKESSEDOUGOU Téhini ! ! Koni ! Lafokpokaha !. Angai Tiémé ! ! [! Ouango-Fitini ! Lataha !. Village B ! !. Bodonon ! ! Seydougou ODIENNE BOUNDIALI Ponondougou Nangakaha ! ! Sokoro 1 Kokoun [! ! ! M'bengué-Bougou !. ! Séguétiélé ! Nangoukaha Balékaha /" Siempurgo ! ! Village C !. ! ! Koumbala Lingoho ! Bouko Koumbolokoro Nazinékaha Kounzié ! ! KORHOGO Nongotiénékaha Togoniéré ! Sirana -

Côte D'ivoire
Côte d’Ivoire Monthly Humanitarian Report October 2011 www.unocha.org The mission of the United Nations Office for the Coordination of Humanitarian Affairs (OCHA) is to mobilize and coordinate effective and principled humanitarian action in partnership with national and international actors. Coordination Saves Lives • Celebrating 20 years of coordinated humanitarian action October 2011 Côte d’Ivoire Humanitarian Bulletin | 2 Côte d’Ivoire Monthly Humanitarian Report Coordination Saves Lives No.1 | October 2011 HIGHLIGHTS ■ The number of Internally Displaced People (IDPs) on 35 sites across the country is gradually decreasing. ■ A National Committee for Coordination of Humanitarian Action (CNCAH) was established by ministerial decree (Minister of State, Employment, Social Affairs and Solidarity) on 5 October 2011. ■ Ivorian refugees in Liberia are spontaneously and gradually returning to their villages of origin in the Moyen Cavally region. ■ The Humanitarian Coordinator and the Ivorian Minister for Employment, Solidarity and Social Affairs visited several European capitals to mobilize support for humanitarian action in Côte d'Ivoire. ■ The Special Representative of the UN Secretary General in Côte d'Ivoire took office on 24 October. I. GENERAL CONTEXT During October, violent incidents took place in the towns of Issia, Guiglo and Bangolo in the West of the country. These incidents resulted in the displacement of an estimated 450 people according to the Protection Cluster. In the Lagunes region, there has been an upsurge of security incidents: several cases of armed robbery, home intrusion and theft are reported to have been committed by armed men in the districts of Anyama, Abobo and Yopougon, in Abidjan. This situation is reportedly due to the free circulation of firearms and to escapee- prisoners since the post-electoral crisis. -

Cote D'ivoire Operational Plan Report FY 2013
Approved Cote d'Ivoire Operational Plan Report FY 2013 Note: Italicized sections of narrative text indicate that the content was not submitted in the Lite COP year, but was derived from the previous Full COP year. This includes data in Technical Area Narratives, and Mechanism Overview and Budget Code narratives from continued mechanisms. Custom Page 1 of 354 FACTS Info v3.8.12.2 2014-01-14 08:08 EST Approved Operating Unit Overview OU Executive Summary Country Context Almost two years after the Ouattara administration came into office, Côte d'Ivoire is moving toward stability and growth, putting behind it more than 10 years of civil unrest that divided the country, impoverished the population, decimated health and social services. President Alassane Ouattara’s administration achieved a number of early successes in organizing national legislative elections, originating a new national development strategy, and reinvigorating the investment climate. The government’s efforts to foster economic growth, increase foreign investment, and improve infrastructure are producing results. Following a contraction of 4.7% in 2011, GDP rebounded remarkably, with growth of 8.5% in 2012 and initial IMF forecasts anticipating 8% growth in 2013. Only limited progress, however, has been achieved on national reconciliation efforts, accountability for crimes committed during the crisis years, and security sector reform. About half the population of 22 million survives on less than $2 a day; a similar proportion lives in rural areas with high illiteracy rates and poor access to services. According to the National Poverty Reduction Strategy (2009), the poverty rate worsened from 10% in 1985 to 48.9% in 2008. -

Final Report: International Election Observation Mission to Côte D'ivoire, 2010 Presidential Elections and 2011 Legislative
International Election Observation Mission to Côte d’Ivoire Final Report 2010 Presidential Elections and 2011 Legislative Elections Waging Peace. Fighting Disease. Building Hope. The Carter Center strives to relieve suffering by advancing peace and health worldwide; it seeks to prevent and resolve conflicts, enhance freedom and democracy, and protect and promote human rights worldwide. International Election Observation Mission to Côte d’Ivoire Final Report 2010 Presidential Elections and 2011 Legislative Elections One Copenhill 453 Freedom Parkway Atlanta, GA 30307 (404) 420-5188 Fax (404) 420-5196 www.cartercenter.org The Carter Center Contents Foreword ..................................1 The Appeals Process ......................63 Executive Summary and Recommendations......3 Election-Related Violence ..................65 The Carter Center in Côte d’Ivoire ............3 Certification of Results . .66 Observation Methodology ....................4 Conclusions and Recommendations Conclusions of the Election Observation Mission ..6 Regarding the 2010 Presidential Election.......67 The Carter Center in Côte d’Ivoire — The Carter Center in Côte d’Ivoire — Presidential Election 2010 ..................16 Legislative Elections 2011 . .72 Political Context...........................18 Political Context...........................74 Framework of the Presidential Election ........21 Hijacking of the Election and the Political- Military Crisis ...........................74 Legal Framework ........................21 Boycott of the Front Populaire -
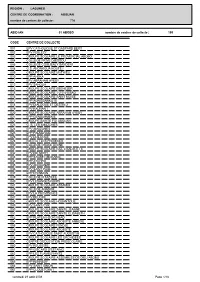
01 ABOBO CODE CENTRE DE COLLECTE ABIDJAN N
REGION : LAGUNES CENTRE DE COORDINATION : ABIDJAN nombre de centres de collecte : 774 ABIDJAN 01 ABOBO nombre de centres de collecte : 155 CODE CENTRE DE COLLECTE 001 EPV CATHOLIQUE ST GASPARD BERT 002 EPV FEBLEZY 003 GROUPE SCOLAIRE LE PROVENCIAL ABOBO 004 COLLEGE PRIVE DJESSOU 006 COLLEGE COULIBALY SANDENI 008 G.S. ANONKOUA KOUTE I 009 GROUPE SCOLAIRE MATHIEU 010 EPP AHEKA 011 EPV ABRAHAM AYEBY 012 EPV SAHOUA 013 GROUPE SCOLAIRE EBENEZER 015 GROUPE SCOLAIRE 1-2-3-4-5 BAD 016 GROUPE SCOLAIRE SAINT MOISE 017 EPP AGNISSANKO III 018 EPV DIALOGUE ET DESTIN 2 019 EPV KAUNAN I 020 GROUPE SCOLAIRE ABRAHAM AYEBY 021 EPP GENDARMERIE 022 GROUPE SAINTE FOI ABIDJAN 023 G. S. LES AMAZONES 024 EPV AMAZONES 025 EPP PALMERAIE 026 EPV DIALOGUE 028 INSTITUT LES PREMICES 030 COLLEGE GRACE DIVINE 031 GROUPE SCOLAIRE RAIL 4 BAD B ET C 032 EPV DIE MORY 033 EPP SAGBE I (BOKABO) 034 EPP ATCHRO 035 EPV ANOUANZE 036 EPV SAINT PAUL 037 EPP N'SINMON 039 COLLEGE H TAZIEFE 040 EPV LESANGES-NOIRS 041 GROUPE SCOLAIRE ASSAMOI 045 COLLEGE ANADOR 046 EPV LA PROVIDENCE 047 EPV BEUGRE 048 GROUPE SCOLAIRE HOUANTOUE 049 EPV SAINT-CYR 050 GROUPE SCOLAIRE SAINTE JEANNE 051 GROUPE SCOLAIRE SAINTE ELISABETH 052 EPP PLATEAU-DOKUI BAD 054 GROUPE SCOLAIRE ABOBOTE ANNEXE 055 GROUPE SCOLAIRE FENDJE 056 GROUPE SCOLAIRE ABOBOTE 057 EPV CATHOLIQUE SAINT AUGUSTIN 058 GROUPE SCOLAIRE LES ORCHIDEES 059 CENTRE D'EDUCATION PRESCOLAIRE 060 EPV REUSSITE 061 EPP GISCARD D'ESTAING 062 EPP LES FLAMBOYANTS 063 GROUPE SCOLAIRE ASSEMBLEE DE DIEU ABOBO 065 EPP KENNEDY 066 EPV SAINT SIMON 067 EPP CLOUETCHA -

Pdf | 348.12 Kb
Côte d’Ivoire Humanitarian Bulletin No. 6 | 2 December 2011 HIGHLIGHTS 16,276 internally displaced people (IDPs) continue to live in 33 sites in Côte d'Ivoire. Joint Assessment Mission conducted by the UN Operation in Côte d'Ivoire, the UN Country Team and the UN Mission in Liberia between 21 and 25 November in Liberia. Former president Laurent Gbagbo transferred to the International Criminal Court in The Hague, the Netherlands, on 29 November. I. General Context A joint technical evaluation mission of the UN Operation in Côte d'Ivoire, the UN Country Teams in Côte d'Ivoire and Liberia as well as the UN Mission in Liberia visited Liberia from 21 – 25 November. The purpose of the mission was to harmonize the joint assessment of the current situation along the border, including in Taï and Toulépleu, to develop strategic approaches in order to tackle the DDR/SSR components of the cross-border stabilization strategy and to encourage young Ivorian refugees to return home. The former Ivorian President, Laurent Gbagbo, has been indicted and under an arrest warrant issued by the International Criminal Court on 29 November. He was immediately transferred the same day and held in custody in the premises of the International Criminal Court (ICC) Hague in the Netherlands. Following the transfer, the party of the former President, Front Populaire Ivoirien (FPI) announced that it will be withdrawing from “any reconciliation process”. II. Humanitarian Situation Protection The seminar for building the capacities of the Republican Forces of Côte d'Ivoire (FRCI) held from 16 to 25 November was formally brought to an end in the presence of Mrs. -

Interim Eligibility Guidelines for Assessing the International Protection Needs of Asylum-Seekers from Cote D'ivoire
INTERIM ELIGIBILITY GUIDELINES FOR ASSESSING THE INTERNATIONAL PROTECTION NEEDS OF ASYLUM-SEEKERS FROM COTE D’IVOIRE United Nations High Commissioner for Refugees (UNHCR) 15 June 2012 HCR/EG/CIV/12/01 Table of Contents LIST OF ABBREVIATIONS .......................................................................................... 3 I. INTRODUCTION ......................................................................................................... 4 II. BACKGROUND INFORMATION ........................................................................... 5 III. ELIGIBILITY FOR INTERNATIONAL PROTECTION .................................. 15 A. POTENTIAL RISK PROFILES ................................................................................................... 16 1. Persons Belonging to Certain Ethnic Groups .................................................................. 16 a) Persons Belonging to Certain Ethnic Groups in the West of the Country ...................................18 b) Persons Belonging to Certain Ethnic Groups in Abidjan ............................................................22 2. Members and Supporters of Political Opposition Parties, and Individuals with Alleged Links to Former President Gbagbo’s Government ............................................................... 24 a) Members and Supporters of Political Opposition Parties ............................................................24 3. Journalists and Other Media Professionals Perceived to be Hostile to the Ouattara Government.......................................................................................................................... -

176 a Critical Period for Ensuring Stability in Cote Divoire
A CRITICAL PERIOD FOR ENSURING STABILITY IN CÔTE D’IVOIRE Africa Report N°176 – 1 August 2011 TABLE OF CONTENTS EXECUTIVE SUMMARY AND RECOMMENDATIONS ................................................. i I. INTRODUCTION ............................................................................................................. 1 II. THE SECURITY CHALLENGE .................................................................................... 3 A. FRAGMENTED FORCES ................................................................................................................. 3 B. MULTIPLE THREATS .................................................................................................................... 5 C. FILL THE SECURITY VACUUM ...................................................................................................... 6 III. RECONCILIATION AND JUSTICE ............................................................................. 8 A. A BLOODY CONFLICT .................................................................................................................. 8 B. AN END TO IMPUNITY ................................................................................................................ 10 IV. CREATE THE CONDITIONS FOR POLITICAL NORMALISATION ................. 12 V. AN ECONOMIC EMERGENCY .................................................................................. 14 VI. CONCLUSION ................................................................................................................ 16 APPENDICES -

Pdf | 563.11 Kb
Côte d’Ivoire Humanitarian Bulletin No. 7 | 9 December 2011 HIGHLIGHTS Maiden repatriation convoy of 546 Ivorian refugees from Liberia facilitated by the UN High Commission for Refugees (UNHCR) on 8 December. Three people killed and three others wounded by an explosion during the electoral campaign meet of a Democratic Party of Cote D’Ivoire (PDCI) candidate in Grand Lahou, on 7 December. A 1st tripartite agreement on voluntary repatriation of Ivorian refugees in Guinea signed on 1 December in Conakry between the Governments of Guinea, Côte d'Ivoire and the UNHCR. I. General Context As the legislative elections of 11 December approaches, the security situation remains calm throughout the country, except for the recent incident in Grand Lahou, about a hundred kilometers west of Abidjan, where an explosion from a propelled rocket killed three people and wounded three others during a political campaign of a Democratic Party of Cote D’Ivoire (PDCI) candidate.. Investigations are reported to be on-going. However, as part of the legislative elections, important security measures have been taken by the authorities in Abidjan, particularly through the mobilization of several tens of thousands law enforcement agents, the gendarmerie, army and United Nations Operation in Côte d'Ivoire (UNOCI) Peacekeepers to guarantee security during the elections. As part of the tripartite agreement setting the conditions for the voluntary repatriation of Ivorian refugees from Liberia, signed on 11 August, a maiden convoy of 546 Ivorian refugees, i.e. 219 families from Nimba County and Grand Gedeh was facilitated by UNHCR on 8 December. Final destinations of the returnees include the Departments of Bloléquin, Danané, Guiglo and Toulépleu. -

UNICEF Côte D'ivoiresituation Report #21 10 June 2011
UNICEF Côte d’IvoireSituation Report #21 10 June 2011 Reporting Period: 3-10 June 2011 For External Use A displaced girl holds a plastic bottle as she waits to fill it with water from a pipe outside a navy training centre in Abidjan, Coted'Ivoire. © UNICEF Côte d’Ivoire/2011/Asselin Highlights • Although generally calm, incidents of abuses continued to be reported this week. There is a wide perception of insecurity by the displaced population , which is hampering the assistance provided to host families and IDPs and preventing returns. Many are seeking refuge in the forest far from the main roads without any adequate services. • UNICEF provided urgent medical supplies to treat up to 1,000 patients to health authorities in Abidjan, after at least 42 cases of cholera were confirmed in the Koumassi district since 16 May. Soap, chlorine, and water treatment kits were also provided for up to 400,000 people. • While 90 per cent of schools have reopened and 85 per cent of students have gone back to school, at least 350,000 students who were enrolled prior to the crisis are still out-of-school . The distribution of teaching and learning materials, provision of teacher training, and organisation of social mobilisation activities are essential for the coming weeks to minimise drop-out. SITUATION OVERVIEW Insecurity persists, as incidents of abuses continued to be reported this week despite the commitment of the new Government to restore order and security. Some IDPs from Danane and Zouan-Hounien sites returned to their villages, while some new displaced persons came to seek refuge in these sites.