Cognitive-Behavioural Therapy of Obsessive- Compulsive Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inositol Safety: Clinical Evidences
European Review for Medical and Pharmacological Sciences 2011; 15: 931-936 Inositol safety: clinical evidences G. CARLOMAGNO, V. UNFER AGUNCO Obstetrics & Gynecology Center, Rome (Italy) Abstract. – Myo-inositol is a six carbon ent required by the human cells for the growth cyclitol that contains five equatorial and one axi- and survival in the culture. In humans and other al hydroxyl groups. Myo-inositol has been classi- species, Myo-inositol can be converted to either fied as an insulin sensitizing agent and it is L- or D-chiro-inositol by epimerases. Early stud- commonly used in the treatment of the Polycys- tic Ovary Syndrome (PCOS). However, despite ies showed that inositol urinary clearance was al- its wide clinical use, there is still scarce informa- tered in type 2 diabetes patients, the next step tion on the myo-inositol safety and/or side ef- was to link impaired inositol clearance with in- fects. The aim of the present review was to sum- sulin resistance (for a review see1). Because of marize and discuss available data on the myo-in- these properties, inositol have been classified as ositol safety both in non-clinical and clinical set- “insulin sensitizing agent”2. tings. The main outcome was that only the highest In the recent years, inositol has found more dose of myo-inositol (12 g/day) induced mild and more space in the reproductive clinical prac- gastrointestinal side effects such as nausea, fla- tice3-6. Indeed, since the main therapy for Poly- tus and diarrhea. The severity of side effects did cystic Ovary Syndrome (PCOS) is the use of in- not increase with the dosage. -
Tic Disorders
No. 35 May 2012 Tic Disorders A tic is a problem in which a part of the body moves repeatedly, quickly, suddenly and uncontrollably. Tics can occur in any body part, such as the face, shoulders, hands or legs. They can be stopped voluntarily for brief periods. Sounds that are made involuntarily (such as throat clearing, sniffing) are called vocal tics. Most tics are mild and hardly noticeable. However, in some cases they are frequent and severe, and can affect many areas of a child's life. The most common tic disorder is called "transient tic disorder" and may affect up to 10 percent of children during the early school years. Teachers or others may notice the tics and wonder if the child is under stress or "nervous." Transient tics go away by themselves. Some may get worse with anxiety, tiredness, and some medications. Some tics do not go away. Tics which last one year or more are called "chronic tics." Chronic tics affect less than one percent of children and may be related to a special, more unusual tic disorder called Tourette's Disorder. Children with Tourette's Disorder have both body and vocal tics (throat clearing). Some tics disappear by early adulthood, and some continue. Children with Tourette's Disorder may also have problems with attention, and learning disabilities. They may act impulsively, and/or develop obsessions and compulsions. Sometimes people with Tourette's Disorder may blurt out obscene words, insult others, or make obscene gestures or movements. They cannot control these sounds and movements and should not be blamed for them. -

Anxiety Disorders in Children Revised 2020
Information about: Anxiety Disorders in Children Revised 2020 Vermont Family Network 600 Blair Park Road, Ste 240 Williston, VT 05495 1-800-800-4005 www.VermontFamilyNetwork.org Introduction According to The Child Mind Institute, “Children with anxiety disorders are overwhelmed by feelings of intense fear or worry that they are out of proportion to the situation or thing that triggers them. These emotional fears can be focused on separating from parents, physical illness, performing poorly, or embarrassing themselves. Or they can be attached to specific things, like dogs or insects or bridges.” We hope that this will give you a greater understanding of anxiety disorders and the ways that parents and professionals can support children at home, in school, and in the community. We have selected information from various sources and provided internet links when possible. The information we have presented was used by permission from various sources. We have provided links for you to find more, in-depth information at their sites. Contents Title Page Anxiety Disorders in Children and Adolescents 2 Additional Treatments and Guidance 2 The Anxious Child 3 Anxiety Quick Fact Sheet for School Personnel & 4 Parents/Guardians Children Who Won’t Go to School (Separation Anxiety) 6 Managing Anxiety with Siblings 6 Panic Disorder in Children and Adolescents 7 Parenting Tips for Anxious Kids 8 Getting Linked (local resources) 9 Advocating for Your Child: 25 Tips for Parents 10-12 Resources 13 Anxiety Disorders in Children and Adolescents What Are Anxiety Disorders? According to The National Alliance on Mental Illness (NAMI)*, “Anxiety disorders are the most common mental health concern in the United States. -

OCD Bingo Instructions
OCD Bingo Instructions Host Instructions: · Decide when to start and select your goal(s) · Designate a judge to announce events · Cross off events from the list below when announced Goals: · First to get any line (up, down, left, right, diagonally) · First to get any 2 lines · First to get the four corners · First to get two diagonal lines through the middle (an "X") · First to get all squares (a "coverall") Guest Instructions: · Check off events on your card as the judge announces them · If you satisfy a goal, announce "BINGO!". You've won! · The judge decides in the case of disputes This is an alphabetical list of all 29 events: Anxiety, Aviator, Brain, C.B.T., Clomipramine, Comorbidity, Compulsions, Counting, Cyclical, Hand-washing, Hepburn, History, Hughes, Indirect pathway, O.C.D., O.C.P.D., Obsessions, Persistent, Plane crash, Psychology, Recurrent, Screen Room, Scrupulosity, Stress, Tic Disorder, Washing, Y-BOCS, Zwangsneurose, phlebotomy. BuzzBuzzBingo.com · Create, Download, Print, Play, BINGO! · Copyright © 2003-2021 · All rights reserved OCD Bingo Call Sheet This is a randomized list of all 29 bingo events in square format that you can mark off in order, choose from randomly, or cut up to pull from a hat: Stress C.B.T. Hughes Hand-washing Aviator Tic Washing Obsessions O.C.D. Persistent Disorder Screen Psychology phlebotomy O.C.P.D. Scrupulosity Room Plane Compulsions Counting Zwangsneurose Comorbidity crash Clomipramine Y-BOCS Anxiety History Hepburn Indirect Cyclical Brain Recurrent pathway BuzzBuzzBingo.com · Create, Download, Print, Play, BINGO! · Copyright © 2003-2021 · All rights reserved B I N G O Screen Brain History Y-BOCS Aviator Room Zwangsneurose Hughes phlebotomy Persistent Anxiety Plane C.B.T. -

2 Türk Psikiyatri Dergisi 2 Turkish Journal of Psychiatry
2 Türk Psikiyatri Dergisi 2 Turkish Journal of Psychiatry CİLT | Volume 27 GÜZ | Autumn 2016 EK | Supplement 2: 52. ULUSAL PSİKİYATRİ KONGRESİ TÜRKİYE SİNİR VE ABSTRACTS RUH SAĞLIĞI ISSN 1300 – 2163 DERNEĞİ 2 Türk Psikiyatri Dergisi 2 Mart, Haziran, Eylül ve Aralık aylarında olmak üzere yılda 4 sayı çıkar Turkish Journal of Psychiatry Four issues annually: March, June, September, December CİLT | Volume 27 GÜZ | Autumn 2016 Türkiye Sinir ve Ruh Sağlığı Derneği EK | Supplement 2 tarafından yayınlanmaktadır. ISSN 1300 – 2163 www.turkpsikiyatri.com Türk Psikiyatri Dergisi Bu Sayının Yayın Yönetmeni /Editor in Chief of this Issue Doç. Dr. Semra Ulusoy Kaymak Türkiye Sinir ve Ruh Sağlığı Derneği adına Sahibi ve Sorumlu Müdürü Kongre Başkanları Published by Turkish Association of Nervous and Mental Health Prof. Dr. M. Orhan Öztürk E. Timuçin Oral - Ekrem Cüneyt Evren Düzenleme Kurulu Yayın Yönetmeni/ Editor in Chief Ekrem Cüneyt Evren (Başkan) Prof. Dr. Aygün Ertuğrul Ercan Dalbudak Selim Tümkaya Yazışma Adresi / Corresponding Address Semra Ulusoy Kaymak PK 401, Yenişehir 06442 Ankara Sinan Aydın (Genç Üye) Yönetim Yeri / Editorial Office Bu Sayının Yayın Yönetmen Yardımcıları Kenedi Cad. 98/4, Kavaklıdere, Ankara / Assoc. Editors in Chief of this Issue Telefon: (0-312) 427 78 22 Faks: (0-312) 427 78 02 Sinan Aydın Esra Kabadayı Yayın Türü / Publication Category Selim Tümkaya Yaygın, Süreli, Bilimsel Yayın Yayın Hizmetleri / Publishing Services BAYT Bilimsel Araştırmalar Reklam / Advertisements Basın Yayın ve Tanıtım Ltd. Şti. Reklam koşulları ve diğer ayrıntılar için yayın yönetmeniyle Tel (0-312) 431 30 62, Faks: (0-312) 431 36 02 ilişkiye geçilmesi gerekmektedir. E-posta: [email protected] (Dergide yer alan yazılarda belirtilen görüşlerden yazarlar sorumludur. -
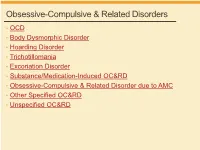
Obsessive-Compulsive & Related Disorders
Obsessive-Compulsive & Related Disorders • OCD • Body Dysmorphic Disorder • Hoarding Disorder • Trichotillomania • Excoriation Disorder • Substance/Medication-Induced OC&RD • Obsessive-Compulsive & Related Disorder due to AMC • Other Specified OC&RD • Unspecified OC&RD B Chow 2019 OCD OCD – Diagnostic Criteria A. Obsessions, compulsions, or both: 1. Obsessions (2/2) • Recurrent thoughts/urges/images, intrusive + unwanted, distressing • Attempts to supress, ignore or neutralize 2. Compulsions (2/2) • Repetitive behaviors, feels driven to do, due to obsession or rules • Aimed to prevent anxiety/distress, but not connected or excessive B. Time-consuming, or sig distress/impairment C. Not due to substance or AMC D. Not better explained by AMD DSM5 OCD – Diagnostic Specifiers • Specify if: • With good or fair insight: recognizes definitely/probably not true • With poor insight: thinks probably true • With absent insight/delusional beliefs: convinced beliefs are true • Specify if: • Tic-related: current OR past hx of tic disorder DSM5 OCD – Diagnostic Specifiers • Dysfunctional beliefs • Inflated sense of responsibility, tendency to overestimate threat • Perfectionism, intolerance of uncertainty • Over-importance of thoughts, need to control thoughts • Degree of insight → accuracy of beliefs, can vary over course • Good/fair insight → many • Poor insight → some • Absent insight/delusional beliefs → 4% or less • Poorer insight → worse long-term outcome • Tic disorders → 30% of OCD have lifetime tic disorder • Most common in MALES with childhood-onset -
DSM-V Overview 1.2 Section II: Diagnostic Criteria and Codes
DSM-V Overview 1.2 Section II: diagnostic criteria and codes 1.2.1 Neurodevelopmental disorders "Mental retardation" has a new name: "intellectual disability (intellectual developmental disorder)."[4] Phonological disorder and stuttering are now called communication disorders—which include language disorder, speech sound disorder, childhood-onset fluency disorder, and a new condition characterized by impaired social verbal and nonverbal communication called social (pragmatic) communication disorder.[4] Autism spectrum disorder incorporates Asperger disorder, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (PDD-NOS) - see Diagnosis of Asperger syndrome#Proposed changes to DSM-5.[5] A new sub-category, motor disorders, encompasses developmental coordination disorder, stereotypic movement disorder, and the tic disorders including Tourette syndrome.[6] 1.2.2 Schizophrenia spectrum and other psychotic disorders All subtypes of schizophrenia were deleted (paranoid, disorganized, catatonic, undifferentiated, and residual).[2] A major mood episode is required for schizoaffective disorder (for a majority of the disorder's duration after criterion A [related to delusions, hallucinations, disorganized speech or behavior, and negative symptoms such as avolition] is met).[2] Criteria for delusional disorder changed, and it is no longer separate from shared delusional disorder.[2] Catatonia in all contexts requires 3 of a total of 12 symptoms. Catatonia may be a specifier for depressive, bipolar, -
Tourette Syndrome and Tic Disorders
Tourette Syndrome and Tic Disorders Presentation by Kiran Singh, PGY-3 UCI/CHOC Pediatrics Residency Program Case 1: Leslie ● 8 year old previously healthy female. At age 6, she started developing involuntary blinking and head jerking. These movements will sometimes recede for a couple of weeks but then reappear without any known triggers. She has a family history of generalized anxiety disorder in mom, OCD in dad. She is not on any medications currently. Otherwise, she is doing well in school, and has been told she has “above average intelligence. Mom does, however, report that she has “an anxious temperament.” What is her diagnosis? Case 2: Benjamin ● 11 year old with history of inattention and hyperactivity presenting with a history of throat clearing since age 10, with grimacing and shoulder shrugging. Mom is frustrated with his behavior, saying “first he wouldn’t stop disrupting class by clearing his throat loudly, which finally got better over the last few weeks, but now he’s starting to make grunting sounds!” Benjamin says he can’t control these actions, that he just has an urge to them and feels better after doing them. He otherwise is not on any medications. His brother has a history of ADHD. What is his diagnosis? Tic Disorders: DSM V diagnoses ● Tourette’s disorder: the presence of both motor and vocal tics for more than 1 year (Case 2: Benjamin) ● Persistent (chronic) motor or vocal tic disorder: single or multiple motor or vocal tics for more than 1 year, but not both motor and vocal (Case 1: Leslie) ● Provisional tic disorder -

Letters to the Editor
Letters to the Editor Letters to the Editor © Copyright 1998 Physicians Postgraduate Press, Inc. Possible Risks Associated With 3. Witvrouw M, Schmit JC, Van Remoortel B, et al. Cell type-dependent Valproate Treatment of AIDS-Related Mania effect of sodium valproate on human immunodeficiency type 1 repli- cation in vitro. AIDS Res Hum Retroviruses 1997;13:187–192 4. Kuntz-Simon G, Obert G. Sodium valproate, an anticonvulsant drug, Sir: Recently, RachBeisel and Weintraub contributed further stimulates human cytomegalovirus replication. J Gen Virol 1995;76: to the literature on the usefulness of valproate for treating 1409–1415 AIDS-related mania.1 Contrary to current trends, they appar- ently prescribed valproic acid rather than divalproex sodium— James W. Jefferson, M.D. the former being less expensive, but generally less well Middleton, Wisconsin tolerated. Given the likelihood of preexisting gastrointestinal symptoms in this population, better tolerability rather than lower cost might make divalproex sodium the preferred prepa- Attacks of Jealousy ration. One personal copy may be printed That Responded to Clomipramine The authors suggest the need for further study of the use of valproate in patients with AIDS because of uncommon reports of thrombocytopenia, hepatic dysfunction, and pancreatitis as- Sir: Pathologic jealousy can be a manifestation of several sociated with the drug. They did not mention a further cause for psychiatric disorders. The patient described here suffered from concern, namely, that in vitro studies have found that valproate an atypical form of obsessive-compulsive disorder, had a strong stimulates HIV-1 virus replication2,3 and cytomegalovirus repli- family history of emotional disturbance and relationship diffi- cation.4 Were this to happen in AIDS patients, the course of the culties, and responded dramatically to treatment with low-dose illness could be altered unfavorably. -

The Course and Clinical Features of Obsessive Compulsive Disorder
111 THE COURSE AND CLINICAL FEATURES OF OBSESSIVE- COMPULSIVE DISORDER STEVEN A. RASMUSSEN JANE L. EISEN Twenty years have passed since the landmark National Epi- to 3% of the general population in the United States meet demiology Catchment Area Survey first demonstrated the lifetime DSM criteria for OCD (4). In a World Health prevalence of obsessive-compulsive disorder (OCD) in the Organization study that determined the leading causes of general population to be 50 to 100 times greater than had mortality and morbidity in developed countries, OCDwas been previously believed (1). This unexpected finding was found to be the eighth leading cause of disability for any instrumental in the renewed interest in and rapid growth of medical or psychiatric condition for ages 15 through 44 (5). our understanding of the clinical features, pathophysiology, Total costs of the disorder in the United States have been and treatment of OCD. Epidemiologic studies in different estimated at $8 billion in 1990, including $2.1 billion in cultures have confirmed the findings that up to 1% to 2% of direct costs and $5.9 billion in indirect costs related to lost the general population worldwide suffer from the disorder at productivity (6). any given time (2). Widespread attention in the media, in However, despite the increased recognition of the public addition to growing recognition of the disorder among health significance of OCDduring the last decade, surpris- health care professionals, has resulted in improvements in ingly little is known about the long-term course and prog- the diagnosis and treatment of large numbers of patients nosis of the disorder. -

5-HT2A Receptors in the Central Nervous System the Receptors
The Receptors Bruno P. Guiard Giuseppe Di Giovanni Editors 5-HT2A Receptors in the Central Nervous System The Receptors Volume 32 Series Editor Giuseppe Di Giovanni Department of Physiology & Biochemistry Faculty of Medicine and Surgery University of Malta Msida, Malta The Receptors book Series, founded in the 1980’s, is a broad-based and well- respected series on all aspects of receptor neurophysiology. The series presents published volumes that comprehensively review neural receptors for a specific hormone or neurotransmitter by invited leading specialists. Particular attention is paid to in-depth studies of receptors’ role in health and neuropathological processes. Recent volumes in the series cover chemical, physical, modeling, biological, pharmacological, anatomical aspects and drug discovery regarding different receptors. All books in this series have, with a rigorous editing, a strong reference value and provide essential up-to-date resources for neuroscience researchers, lecturers, students and pharmaceutical research. More information about this series at http://www.springer.com/series/7668 Bruno P. Guiard • Giuseppe Di Giovanni Editors 5-HT2A Receptors in the Central Nervous System Editors Bruno P. Guiard Giuseppe Di Giovanni Faculté de Pharmacie Department of Physiology Université Paris Sud and Biochemistry Université Paris-Saclay University of Malta Chatenay-Malabry, France Msida MSD, Malta Centre de Recherches sur la Cognition Animale (CRCA) Centre de Biologie Intégrative (CBI) Université de Toulouse; CNRS, UPS Toulouse, France The Receptors ISBN 978-3-319-70472-2 ISBN 978-3-319-70474-6 (eBook) https://doi.org/10.1007/978-3-319-70474-6 Library of Congress Control Number: 2017964095 © Springer International Publishing AG 2018 This work is subject to copyright. -

Pediatric Autoimmune Neuropsychiatric Disorder
Research Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal Infection (PANDAS): Clinical Manifestations, IVIG Treatment Outcomes, Results from a Cohort of Italian Patients Piero Pavone1, Raffaele Falsaperla1, Francesco Nicita2, Andreana Zecchini3, Chiara Battaglia1, Alberto Spalice 2, Lucia Iozzi3, Enrico Parano4, Giovanna Vitaliti1, Alberto Verrotti5, Vincenzo Belcastro6, Sung Yoon Cho7,†, Dong-Kyu Jin7, Salvatore Savasta3 Abstract Pediatric Autoimmune Neuropsychiatric Disorder associated with Streptococcal Infection (PANDAS) is characterized with main clinical features including obsessive-compulsive disorders and tics, acute-onset in prepubertal age, relapsing-remitting course, association with neurological abnormalities (mainly choreiform movements and motor hyperactivity), and temporal relationship with group A streptococcal infections. Thirty- four children with a serious- severe grade of PANDAS were enrolled in Italian Institutions with the aim to report clinical manifestations of the patients and their response to the intravenous immunoglobulin (IVIG) treatment. All patients were selected according to the Swedo‘s criteria and specific laboratory investigations as suggested by Chang for the PANS and treated with IVIG at the dosage of 2 g/kg/day for two consecutive days. At the onset, all patients presented with at least, one psychiatric manifestation including anxiety, emotional lability, bedwetting, enuresis, and phobia, and oppositional behavior including temper tantrums, personality changes, and deterioration in math skills and handwriting. At the laboratory investigations, positivity of pharyngeal swab for streptococcal infection in most of the patients and variable titers of anti-DNase B and ASO were found. In 29 patients reduction or disappearing of the motor symptoms were reached after 1 or 2 cycles of IVIG treatment, while in 5 patients the symptoms reappeared after the third cycle of IVIG.