DSM Part 2 Changes to Depressive Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ch 28 Dobersek Eklund-FINAL .Pdf
Chapter 28 Social Physique Anxiety and Muscle Dysmorphia Urska Dobersek & Robert C. Eklund Social physique anxiety (SPA) and body dysmorphic disorder (BDD) have the body as a common denominator. These constructs both involve concerns with either others or one’s own perceptions about the body or specific physical features; SPA involves concern about the evaluation of others while BDD involves concern over self-perceptions. This chapter provides definitions and information on diagnostic and statistical elements of SPA, BDD, and muscle dysmorphia (MD) which is a particular type of BDD. Psychological, physiological, and environmental factors implicated in the experience of these constructs are outlined as well as potential co-morbidities. Despite the wide range of physical and psychological benefits derived from exercise and physical activity, evidence suggests that these involvements can have negative effects for some individuals with SPA and MD. Consulting, counseling, and pharmacological strategies for addressing SPA and MD are outlined including commentary on cognitive behavior therapy (CBT), antidepressants (e.g., selective serotonin reuptake inhibitors), and a combination thereof. In this chapter we first provide commentary on the theoretical background of the mechanisms that play an essential role in development of SPA and MD among exercisers and physically active individuals. Main topics and associated concepts are introduced in vignettes to illustrate experiences of SPA and MD, and how they relate to exercise and physical activity. We then describe variables that have been linked to SPA and MD, including potential causes, moderators, mediators, and other correlates. Finally, we provide theoretically grounded recommendations for the professionals working with the physically active individuals who 1 portray symptoms of SPA and/or MD and provide suggested readings for further exploration in the area. -

2 Türk Psikiyatri Dergisi 2 Turkish Journal of Psychiatry
2 Türk Psikiyatri Dergisi 2 Turkish Journal of Psychiatry CİLT | Volume 27 GÜZ | Autumn 2016 EK | Supplement 2: 52. ULUSAL PSİKİYATRİ KONGRESİ TÜRKİYE SİNİR VE ABSTRACTS RUH SAĞLIĞI ISSN 1300 – 2163 DERNEĞİ 2 Türk Psikiyatri Dergisi 2 Mart, Haziran, Eylül ve Aralık aylarında olmak üzere yılda 4 sayı çıkar Turkish Journal of Psychiatry Four issues annually: March, June, September, December CİLT | Volume 27 GÜZ | Autumn 2016 Türkiye Sinir ve Ruh Sağlığı Derneği EK | Supplement 2 tarafından yayınlanmaktadır. ISSN 1300 – 2163 www.turkpsikiyatri.com Türk Psikiyatri Dergisi Bu Sayının Yayın Yönetmeni /Editor in Chief of this Issue Doç. Dr. Semra Ulusoy Kaymak Türkiye Sinir ve Ruh Sağlığı Derneği adına Sahibi ve Sorumlu Müdürü Kongre Başkanları Published by Turkish Association of Nervous and Mental Health Prof. Dr. M. Orhan Öztürk E. Timuçin Oral - Ekrem Cüneyt Evren Düzenleme Kurulu Yayın Yönetmeni/ Editor in Chief Ekrem Cüneyt Evren (Başkan) Prof. Dr. Aygün Ertuğrul Ercan Dalbudak Selim Tümkaya Yazışma Adresi / Corresponding Address Semra Ulusoy Kaymak PK 401, Yenişehir 06442 Ankara Sinan Aydın (Genç Üye) Yönetim Yeri / Editorial Office Bu Sayının Yayın Yönetmen Yardımcıları Kenedi Cad. 98/4, Kavaklıdere, Ankara / Assoc. Editors in Chief of this Issue Telefon: (0-312) 427 78 22 Faks: (0-312) 427 78 02 Sinan Aydın Esra Kabadayı Yayın Türü / Publication Category Selim Tümkaya Yaygın, Süreli, Bilimsel Yayın Yayın Hizmetleri / Publishing Services BAYT Bilimsel Araştırmalar Reklam / Advertisements Basın Yayın ve Tanıtım Ltd. Şti. Reklam koşulları ve diğer ayrıntılar için yayın yönetmeniyle Tel (0-312) 431 30 62, Faks: (0-312) 431 36 02 ilişkiye geçilmesi gerekmektedir. E-posta: [email protected] (Dergide yer alan yazılarda belirtilen görüşlerden yazarlar sorumludur. -

Muscle Dysmorphia: Under-Researched and Potentially
Muscle Dysmorphia: Under-researched and potentially Over-diagnosed Muscle Dysmorphia is a recently described psychiatric disorder, characterized by a pathological preoccupation with muscle size. [1] This paper aims to define Muscle Dysmorphia and explore its aetiology and ramifications, including psychological distress and an association with the use and abuse of Androgenic Anabolic Steroids. Muscle Dysmorphia is often referred to as a subtype of Body Dysmorphia, with features that correlate with an Eating Disorder and Obsessive-Compulsive Disorder. I will look into the diagnostic criteria of these disorders, and highlight the suggested similarities they share with Muscle Dysmorphia. I believe there is a lack of definitive diagnostic criteria for Muscle Dysmorphia, which fails to clearly distinguish between what is normal and what is not when it comes to bodybuilding. The media has sensationalized this disorder, and portrayed a stereotyped, over-generalized view of what Muscle Dysmorphia is and the individuals who are affected by it. I believe this is due to the general public being uniformed, and there is a need for someone who is informed to explore this topic in depth in order to avoid over-diagnosis. I will explore the mindset of normal athletes - i.e. those who enjoy building muscle, highlight the flaws with the current diagnostic criteria, and suggest necessary future research. What is Muscle Dysmorphia An individual affected by Muscle Dysmorphia is overly concerned with his or her degree of muscularity, whereby there is a pervasive belief that they are insufficiently large and lack adequate muscularity. This preoccupation with muscle building leads to a never-ending quest to become bigger and more muscular. -

Muscle Dysmorphia: Current Insights 1
MUSCLE DYSMORPHIA: CURRENT INSIGHTS 1 REVIEW Short running header: MUSCLE DYSMORPHIA Tod et al Muscle Dysmorphia: Current insights David Tod1 Christian Edwards2 Ieuan Cranswick3 1School of Sport and Exercise Science, Liverpool John Moores University, Liverpool, Merseyside, United Kingdom; 2Institute of Sport and Exercise Science, University of Worcester, Worcester, Worcestershire, United Kingdom; 3School of Sport and Exercise Science, Liverpool John Moores University, Liverpool, Merseyside, United Kingdom Correspondence: David Tod School of Sport and Exercise Science, Byrom Street Liverpool John Moores University Byrom Street Liverpool Merseyside United Kingdom L3 3AF Tel +44 151 904 6241 Email [email protected] MUSCLE DYSMORPHIA: CURRENT INSIGHTS 2 Abstract: Since 1997, there has been increasing research focused on Muscle Dysmorphia, a condition underpinned by people’s beliefs they have insufficient muscularity, in both the Western and non- western medical and scientific communities. Much of this empirical interest has surveyed nonclinical samples, and there is limited understanding of people with the condition beyond knowledge about their characteristics. Much existing knowledge about people with the condition is unsurprising and inherent in the definition of the disorder, such as dissatisfaction with muscularity and adherence to muscle-building activities. Only recently have investigators started to explore questions beyond these limited tautological findings that may give rise to substantial knowledge advances, such as the examination of masculine and feminine norms. There is limited understanding of additional topics such as etiology, prevalence, nosology, prognosis, and treatment. Further, the evidence is largely based on a small number of unstandardized case reports and descriptive studies (involving small samples), largely confined to Western (North American, British, and Australian) males. -
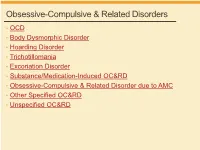
Obsessive-Compulsive & Related Disorders
Obsessive-Compulsive & Related Disorders • OCD • Body Dysmorphic Disorder • Hoarding Disorder • Trichotillomania • Excoriation Disorder • Substance/Medication-Induced OC&RD • Obsessive-Compulsive & Related Disorder due to AMC • Other Specified OC&RD • Unspecified OC&RD B Chow 2019 OCD OCD – Diagnostic Criteria A. Obsessions, compulsions, or both: 1. Obsessions (2/2) • Recurrent thoughts/urges/images, intrusive + unwanted, distressing • Attempts to supress, ignore or neutralize 2. Compulsions (2/2) • Repetitive behaviors, feels driven to do, due to obsession or rules • Aimed to prevent anxiety/distress, but not connected or excessive B. Time-consuming, or sig distress/impairment C. Not due to substance or AMC D. Not better explained by AMD DSM5 OCD – Diagnostic Specifiers • Specify if: • With good or fair insight: recognizes definitely/probably not true • With poor insight: thinks probably true • With absent insight/delusional beliefs: convinced beliefs are true • Specify if: • Tic-related: current OR past hx of tic disorder DSM5 OCD – Diagnostic Specifiers • Dysfunctional beliefs • Inflated sense of responsibility, tendency to overestimate threat • Perfectionism, intolerance of uncertainty • Over-importance of thoughts, need to control thoughts • Degree of insight → accuracy of beliefs, can vary over course • Good/fair insight → many • Poor insight → some • Absent insight/delusional beliefs → 4% or less • Poorer insight → worse long-term outcome • Tic disorders → 30% of OCD have lifetime tic disorder • Most common in MALES with childhood-onset -

Cognitive-Behavioural Therapy of Obsessive- Compulsive Disorder
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Veterinary medicine - Repository of PHD, master's thesis UNIVERSITY OF ZAGREB SCHOOL OF MEDICINE Veronika Nives Zoric Cognitive-Behavioural Therapy of Obsessive- Compulsive Disorder GRADUATE THESIS Zagreb, 2017. This graduate thesis was made at the Department of Psychiatry KBC Zagreb, University of Zagreb School of Medicine, mentored by prof. dr. sc. Dražen Begić and was submitted for evaluation in the 2016/2017 academic year. Mentor: prof. dr. sc. Dražen Begić ABBREVIATIONS USED IN THE TEXT: Behaviour Therapy (BT) Bibliotherapy administered CBT (bCBT) Cognitive-Behavioural Therapy (CBT) Cognitive Therapy (CT) Computerized CBT (cCBT) Danger Ideation Reduction Therapy (DIRT) Deep Brain Stimulation (DBS) Diagnostic and Statistical Manual of Mental Disorders (DSM-5) Exposure and Response Prevention (ERP) Generalized Anxiety Disorder (GAD) International Classification of Disease (ICD-10) Internet-administered CBT (iCBT) Major Depressive Disorder (MDD) Monoamine Oxidase Inhibitors (MAO) Obsessive-Compulsive Disorder (OCD) Obsessive-Compulsive Personality Disorder (OCPD) Selective Serotonin Reuptake Inhibitor (SSRI) Serotonin; 5-hydroxytryptamine (5HT) Serotonin Reuptake Inhibitor (SRI) Subjective Units of Distress Scale (SUDS) Telephone administered CBT (tCBT) Tricyclic Antidepressants (TCA) Videoconferencing administered CBT (vCBT) Yale-Brown Obsessive-Compulsive Scale (Y-BOCS) TABLE OF CONTENTS 1. SUMMARY 2. SAŽETAK 3. INTRODUCTION ............................................................................................................ -

Introduction to Bigorexia
journal homepage: http://kont.zsf.jcu.cz SOciaL SciENCES IN HEALTH DOI: 10.32725/kont.2021.014 KONTakT / Journal of nursing and social sciences related to health and illness Review article Introduction to bigorexia Šárka Tovt, Alena Kajanová * University of South Bohemia in České Budějovice, Institute of Social and Special-paedagogical Sciences, České Budějovice, Czech Republic Abstract Bigorexia was first mentioned in the early 20th century in the USA. It is an unanchored disease with elements of obsessive-compulsive disorder. It is characterized by an obsession with the appearance of one’s body, fear of not having enough muscles, and the urgent need for excessive physical exercise. The disorder can cause other serious illnesses and is also often associated with dependence on anabolic steroids or other addictive substances. The aim of this article is to provide basic information about the problem of bigorexia, including the diagnosis and treatment. It also deals with the possible health and social risks in people suffering from bigorexia. This article presents a set of results of the existing literature in the field of muscle dysmorphia from Web of Science, PubMed, Scopus and other related scientific databases. The studied professional articles were not limited by the date of publication, as the original works provide insight into the initial investigation of bigorexia and the mapping of this disease. The search was performed using keywords related to the issue. The scientific articles were supplemented by diagnostic and statistical manuals and monographs. The research revealed that the issue of bigorexia is mainly dealt with in foreign countries. In the Czech Republic, relevant data regarding this disease is currently lacking. -
DSM-V Overview 1.2 Section II: Diagnostic Criteria and Codes
DSM-V Overview 1.2 Section II: diagnostic criteria and codes 1.2.1 Neurodevelopmental disorders "Mental retardation" has a new name: "intellectual disability (intellectual developmental disorder)."[4] Phonological disorder and stuttering are now called communication disorders—which include language disorder, speech sound disorder, childhood-onset fluency disorder, and a new condition characterized by impaired social verbal and nonverbal communication called social (pragmatic) communication disorder.[4] Autism spectrum disorder incorporates Asperger disorder, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (PDD-NOS) - see Diagnosis of Asperger syndrome#Proposed changes to DSM-5.[5] A new sub-category, motor disorders, encompasses developmental coordination disorder, stereotypic movement disorder, and the tic disorders including Tourette syndrome.[6] 1.2.2 Schizophrenia spectrum and other psychotic disorders All subtypes of schizophrenia were deleted (paranoid, disorganized, catatonic, undifferentiated, and residual).[2] A major mood episode is required for schizoaffective disorder (for a majority of the disorder's duration after criterion A [related to delusions, hallucinations, disorganized speech or behavior, and negative symptoms such as avolition] is met).[2] Criteria for delusional disorder changed, and it is no longer separate from shared delusional disorder.[2] Catatonia in all contexts requires 3 of a total of 12 symptoms. Catatonia may be a specifier for depressive, bipolar, -

Body Dysmorphic Disorder (BDD)
© Mind 2018 Body dysmorphic disorder (BDD) Explains what body dysmorphic disorder (BDD) is, the symptoms and possible causes of BDD and how you can access treatment and support. Includes tips for helping yourself, and advice for friends and family. If you require this information in Word document format for compatibility with screen readers, please email: [email protected] Contents What is body dysmorphic disorder (BDD)? .......................................................................... 2 What are the common signs and symptoms of BDD? .......................................................... 2 What causes BDD? .............................................................................................................. 4 What treatments are available for BDD? ............................................................................. 6 What can I do to help myself? .............................................................................................. 8 How can friends and family help?........................................................................................ 9 Useful contacts .................................................................................................................... 10 1 © Mind 2018 What is body dysmorphic disorder (BDD)? Body dysmorphic disorder (BDD) is an anxiety disorder related to body image. You might be given a diagnosis of BDD if you: experience obsessive worries about one or more perceived flaws in your physical appearance, and the flaw cannot be seen by others or -

A Single Subject Investigation of Behavioral and Cognitive Therapies for Body Dysmorphic Disorder April O'grady
The University of Maine DigitalCommons@UMaine Electronic Theses and Dissertations Fogler Library 5-2002 A Single Subject Investigation of Behavioral and Cognitive Therapies for Body Dysmorphic Disorder April O'Grady Follow this and additional works at: http://digitalcommons.library.umaine.edu/etd Part of the Cognitive Psychology Commons Recommended Citation O'Grady, April, "A Single Subject Investigation of Behavioral and Cognitive Therapies for Body Dysmorphic Disorder" (2002). Electronic Theses and Dissertations. 61. http://digitalcommons.library.umaine.edu/etd/61 This Open-Access Dissertation is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of DigitalCommons@UMaine. A SINGLE SUBJECT INVESTIGATION OF BEHAVIORAL AND COGNITIVE THERAPIES FOR BODY DYSMORPHIC DISORDER BY April O'Grady B.Sc. Memorial University of Newfoundland, 1993 A THESIS Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy (in Psychology) The Graduate School The University of Maine May, 2002 Advisory Committee: Jeffrey Hecker, Associate Professor of Psychology, Co-Chair Geoffrey Thorpe, Professor of Psychology, Co-Chair Bruce Hale, Cooperating Associate Professor of Psychology Alan Rosenwasser, Professor of Psychology Sandra Sigmon, Associate Professor of Psychology Alan Stubbs, Professor of Psychology A SINGLE-SUBJECT INVESTIGATION OF BEHAVIORAL AND COGNITIVE THERAPIES FOR BODY DYSMORPHIC DISORDER By April O'Grady Thesis Co-Advisors: Dr. Jeffrey Hecker, Dr. Geoffrey Thorpe An Abstract of the Thesis Presented In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy (in Psychology) May 2002 Body dysmorphic disorder (BDD), a psychological disorder characterized by an intense preoccupation with an imagined physical defect, causes extreme distress and leads to depression, divorce, and suicide. -

Letters to the Editor
Letters to the Editor Letters to the Editor © Copyright 1998 Physicians Postgraduate Press, Inc. Possible Risks Associated With 3. Witvrouw M, Schmit JC, Van Remoortel B, et al. Cell type-dependent Valproate Treatment of AIDS-Related Mania effect of sodium valproate on human immunodeficiency type 1 repli- cation in vitro. AIDS Res Hum Retroviruses 1997;13:187–192 4. Kuntz-Simon G, Obert G. Sodium valproate, an anticonvulsant drug, Sir: Recently, RachBeisel and Weintraub contributed further stimulates human cytomegalovirus replication. J Gen Virol 1995;76: to the literature on the usefulness of valproate for treating 1409–1415 AIDS-related mania.1 Contrary to current trends, they appar- ently prescribed valproic acid rather than divalproex sodium— James W. Jefferson, M.D. the former being less expensive, but generally less well Middleton, Wisconsin tolerated. Given the likelihood of preexisting gastrointestinal symptoms in this population, better tolerability rather than lower cost might make divalproex sodium the preferred prepa- Attacks of Jealousy ration. One personal copy may be printed That Responded to Clomipramine The authors suggest the need for further study of the use of valproate in patients with AIDS because of uncommon reports of thrombocytopenia, hepatic dysfunction, and pancreatitis as- Sir: Pathologic jealousy can be a manifestation of several sociated with the drug. They did not mention a further cause for psychiatric disorders. The patient described here suffered from concern, namely, that in vitro studies have found that valproate an atypical form of obsessive-compulsive disorder, had a strong stimulates HIV-1 virus replication2,3 and cytomegalovirus repli- family history of emotional disturbance and relationship diffi- cation.4 Were this to happen in AIDS patients, the course of the culties, and responded dramatically to treatment with low-dose illness could be altered unfavorably. -

Understanding Men's Muscularity-Focused Body Image Concerns Through the Lens of Gender Role Conflict and Self-Compassion
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Public Access Theses and Dissertations from the Education and Human Sciences, College of (CEHS) College of Education and Human Sciences 10-31-2016 Repairing the Broken Mirror: Understanding Men's Muscularity-Focused Body Image Concerns Through the Lens of Gender Role Conflict and Self-Compassion. Michael S. Butchko University of Nebraska - Lincoln, [email protected] Follow this and additional works at: http://digitalcommons.unl.edu/cehsdiss Part of the Counseling Psychology Commons, and the Educational Psychology Commons Butchko, Michael S., "Repairing the Broken Mirror: Understanding Men's Muscularity-Focused Body Image Concerns Through the Lens of Gender Role Conflict and Self-Compassion." (2016). Public Access Theses and Dissertations from the College of Education and Human Sciences. 290. http://digitalcommons.unl.edu/cehsdiss/290 This Article is brought to you for free and open access by the Education and Human Sciences, College of (CEHS) at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Public Access Theses and Dissertations from the College of Education and Human Sciences by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. REPAIRING THE BROKEN MIRROR: UNDERSTANDING MEN’S MUSCULARITY-FOCUSED BODY IMAGE CONCERNS THROUGH THE LENS OF GENDER ROLE CONFLICT AND SELF-COMPASSION Michael S. Butchko A DISSERTATION Presented to the Faculty of The Graduate College at the University of Nebraska In Partial Fulfillment of Requirements For the Degree of Doctor of Philosophy Major: Psychological Studies in Education (Counseling Psychology) Under the Supervision of Professor M. Meghan Davidson Lincoln, Nebraska October, 2016 REPAIRING THE BROKEN MIRROR: UNDERSTANDING MEN’S MUSCULARITY-FOCUSED BODY IMAGE CONCERNS THROUGH THE LENS OF GENDER ROLE CONFLICT AND SELF-COMPASSION Michael S.