Foot and Ankle Disorders Capturing Motion with Ultrasound
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Piriformis Syndrome Is Overdiagnosed 11 Robert A
American Association of Neuromuscular & Electrodiagnostic Medicine AANEM CROSSFIRE: CONTROVERSIES IN NEUROMUSCULAR AND ELECTRODIAGNOSTIC MEDICINE Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 AANEM COURSE F AANEM 52ND Annual Scientific Meeting Monterey, California CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Loren M. Fishman, MD, B.Phil Robert A.Werner, MD, MS Scott J. Primack, DO Willam S. Pease, MD Ernest W. Johnson, MD Lawrence R. Robinson, MD 2005 COURSE F AANEM 52nd Annual Scientific Meeting Monterey, California AANEM Copyright © September 2005 American Association of Neuromuscular & Electrodiagnostic Medicine 421 First Avenue SW, Suite 300 East Rochester, MN 55902 PRINTED BY JOHNSON PRINTING COMPANY, INC. ii CROSSFIRE: Controversies in Neuromuscular and Electrodiagnostic Medicine Faculty Loren M. Fishman, MD, B.Phil Scott J. Primack, DO Assistant Clinical Professor Co-director Department of Physical Medicine and Rehabilitation Colorado Rehabilitation and Occupational Medicine Columbia College of Physicians and Surgeons Denver, Colorado New York City, New York Dr. Primack completed his residency at the Rehabilitation Institute of Dr. Fishman is a specialist in low back pain and sciatica, electrodiagnosis, Chicago in 1992. He then spent 6 months with Dr. Larry Mack at the functional assessment, and cognitive rehabilitation. Over the last 20 years, University of Washington. Dr. Mack, in conjunction with the Shoulder he has lectured frequently and contributed over 55 publications. His most and Elbow Service at the University of Washington, performed some of the recent work, Relief is in the Stretch: End Back Pain Through Yoga, and the original research utilizing musculoskeletal ultrasound in order to diagnose earlier book, Back Talk, both written with Carol Ardman, were published shoulder pathology. -

Sensory Conduction in Medial and Lateral Plantar Nerves
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.51.2.188 on 1 February 1988. Downloaded from Journal ofNeurology, Neurosurgery, and Psychiatry 1988;51:188-191 Sensory conduction in medial and lateral plantar nerves S N PONSFORD From the Department of Clinical Neurophysiology, Walsgrave Hospital, Coventry, UK SUMMARY A simple and reliable method of recording medial and lateral plantar nerve sensory action potentials is described. Potentials are recorded with surface electrodes at the ankle using surface electrodes stimulating orthodromically at the sole. The normal values obtained are higher in amplitude than those obtained by the method described by Guiloff and Sherratt and are detectable in older subjects aged over 80 years. The procedure is valuable in the diagnosis of early peripheral neuropathy, mononeuritig multiplex; tarsal tunnel syndrome and in differentiation between pre and post ganglionic L5 SI lesions. The value of medial plantar sensory action potential EL53051 applied to the sole just lateral to the first meta-guest. Protected by copyright. (SAP) recording in the diagnosis of peripheral neuro- tarsal, the anode level with metatarsophalangeal joint, the pathy and investigation of root or individual nerve cathode thus overlying the first common digital nerve sub- lesions involving the leg or foot was clearly estab- serving contiguous surfaces ofthe great and second toes. For the lateral plantar, the stimulator was placed between the lished by Guiloff and Sherratt.1 However, their fourth and fifth metatarsals, the anode-again level with the method of stimulating at the big toe and recording at metatarsophalangeal joint, overlying the fourth common the ankle gives potentials of relatively small ampli- digital nerve supplying contiguous surfaces of the fourth and tude (mean amplitude 2-3 pv, range 0-8- 1). -

Ultrasound of Medial Tarsal Tunnel by Lisa Howell
Ultrasound of Medial Tarsal Tunnel by Lisa Howell Medial Tarsal Tunnel Syndrome Medial Tarsal Tunnel Syndrome (Posterior Tibial Neuralgia) is a compression neuropathy Occurs when Posterior Tibial Nerve (PTN) and / or its branches are entrapped within Tarsal Tunnel of Medial ankle Proximal syndrome compression main trunk of PTN, affects entire foot Distal syndrome compression of divisional branches of PTN Medial TTS: -More complex than carpal tunnel syndrome in wrist -Diagnosis and treatment of TTS depends on cause, and severity -Pain typically radiates down medial ankle to heel and/or plantar aspect of foot -Symptoms occur whilst standing, during exercise, and at night when patient is at rest [Ref: 1, 6] Anatomy Medial Ankle Medial Tarsal Tunnel MTT Fibro-osseous tunnel of medial ankle, posterior and inferior to medial malleolus (MM) Tendons of medial ankle Tibialis posterior (PTT), Flexor digitorum longus (FDL), and Flexor hallucis longus (FHL) Ligaments of medial ankle Deltoid ligament is fan shaped, and originates at MM It is divided into a deep and superficial layers Deep layer : Anterior tibiotalar lig, and Posterior tibiotalar lig Superficial layer: Tibionavicular lig, Tibiospring lig, and Tibiocalcaneal lig Neurovascular bundle Posterior tibial nerve (PTN), Posterior tibial artery (PTA), and Posterior tibial veins (PTV) [Ref : 1,6 ] Anatomy of PTN Posterior Tibial Nerve (PTN) branch of Sciatic nerve divides at medial ankle into three branches : ● Medial Calcaneal Nerve ● Medial Plantar Nerve ● Lateral Plantar Nerve Proximal Medial Tarsal Tunnel Flexor Retinaculum (FR) forms the roof of prox MTT Medial Calcaneal nerve (MCN) first branch of PTN MCN superficial to Abductor Hallucis muscle (AHM) Innervates posterior medial part of calcaneus, and posterior fat pad of foot Distal Medial Tarsal Tunnel Lateral Plantar nerve (LPN), and Medial Plantar nerve (MPN) are the terminal branches of PTN [Ref: 1,6] Frank.H.Netter, MD. -
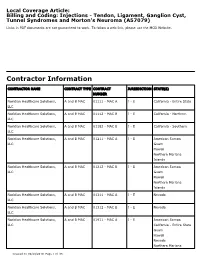
Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079)
Local Coverage Article: Billing and Coding: Injections - Tendon, Ligament, Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma (A57079) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Noridian Healthcare Solutions, A and B MAC 01111 - MAC A J - E California - Entire State LLC Noridian Healthcare Solutions, A and B MAC 01112 - MAC B J - E California - Northern LLC Noridian Healthcare Solutions, A and B MAC 01182 - MAC B J - E California - Southern LLC Noridian Healthcare Solutions, A and B MAC 01211 - MAC A J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01212 - MAC B J - E American Samoa LLC Guam Hawaii Northern Mariana Islands Noridian Healthcare Solutions, A and B MAC 01311 - MAC A J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01312 - MAC B J - E Nevada LLC Noridian Healthcare Solutions, A and B MAC 01911 - MAC A J - E American Samoa LLC California - Entire State Guam Hawaii Nevada Northern Mariana Created on 09/28/2019. Page 1 of 33 CONTRACTOR NAME CONTRACT TYPE CONTRACT JURISDICTION STATE(S) NUMBER Islands Article Information General Information Original Effective Date 10/01/2019 Article ID Revision Effective Date A57079 N/A Article Title Revision Ending Date Billing and Coding: Injections - Tendon, Ligament, N/A Ganglion Cyst, Tunnel Syndromes and Morton's Neuroma Retirement Date N/A Article Type Billing and Coding AMA CPT / ADA CDT / AHA NUBC Copyright Statement CPT codes, descriptions and other data only are copyright 2018 American Medical Association. -

Tarsal Tunnel Syndrome: a Still Challenge Condition
Rev Bras Neurol. 55(1):12-17, 2019 TARSAL TUNNEL SYNDROME: A STILL CHALLENGE CONDITION SÍNDROME DO TÚNEL DO TARSO: UMA CONDIÇÃO AINDA DESAFIADORA Celmir de Oliveira Vilaça1,2, Bruno Pessoa3, Janaína de Moraes Silva4, Victor Hugo Bastos5, Diandra Martins5, Silmar Teixeira6, Victor Marinho6, Rossano Fiorelli7, Vanessa de Albuquerque Dinoa8; Marco Orsini7, 9 ABSTRACT RESUMO Tarsal tunnel syndrome is a rare, under diagnosed and often confu- A Síndrome do túnel do tarso é uma rara e subdiagnosticada neuro- sed neuropathy with other clinical entities. There is a lack of popula- patia geralmente confundida com outras entidades clínicas. Há falta tion studies on this disease. Herein, we performed a non-systematic de estudos populacionais sobre a doença. Assim sendo, realizamos review of articles between January 1992 and February 2018. Althou- uma revisão da literatura de artigos entre Janeiro de 1992 e fevereiro gh with a less complex anatomy comparing to the carpal tunnel, the de 2018. Apesar de possuir uma anatomia de menor complexidade tarsal tunnel is source of pain and some other conditions. Treatment comparada ao túnel do carpo, o túnel do tarso é origem de dor e involves conservative measures such as analgesics and physical the- algumas outras condições. O tratamento envolve medidas conserva- rapy rehabilitation or surgical procedures in case of conservative doras como analgésicos e terapia de reabilitação ou procedimentos treatment failure. Randomized control studies are lack and manda- cirúrgicos, em caso de falha do tratamento conservador. Estudos ran- tory for uncover the best modality of treatment for this condition. domizados são escassos e necessários para descoberta da melhor modalidade de tratamento desta condição. -

Tarsal Tunnel Syndrome
MICHAEL J. BAKER, D.P.M. JASON D. GRAY, D.P.M. GREGORY W. BOAKE, D.P.M JESSICA R TAULMAN, D.P.M BFS BUSINESS OFFICE P O BOX 330. Tarsal Tunnel Syndrome Fortville, IN 46040-0330 Tel 317.863.2556 Fax 317.203.0420 Tarsal tunnel syndrome is an entrapment neuropathy (pressure on nerve) of the tibial nerve as it courses through the inside COMMUNITY FOOT & ANKLE CENTER aspect of the foot and ankle. 1221 Medical Arts Blvd. Anderson, IN 46011 Tel 765.641.0001 Symptoms. Pain, numbness, burning and electrical sensations Fax 765.641.0003 may occur along the course of the nerve, which includes the EAST FOOT & inside of the ankle, heel, arch and bottom of foot. Symptoms are ANKLE CENTER usually worsened with increased activity such as walking or 161B Washington Point Dr. Indianapolis, IN 46229 exercise. Prolonged standing in one place may also be an Tel 317.898.6624 aggravating factor. Fax 317.898.6636 FOOT & ANKLE AT WESTVIEW HOSPITAL 3520 Guion Rd., Ste 102 Indianapolis, IN 46222 Tel 317.920.3240 Fax 317.920.3243 MARION FOOT CENTER 330 N. Wabash Ave, Ste 460A Marion, IN 46952 Tel 765.664.1413 Fax 765.965.6530 BAKER FOOT SOLUTIONS SATILLITE FOOT CLINICS BROWNSBURG Tel 317.920.3240 Causes. There are a variety of factors that may cause tarsal Fax 317.920.3243 tunnel syndrome. These may include repetitive stress with GEIST FAMILY PRACTICE activities, flat feet, and excess weight. Additionally, any lesion Tel 317.898.6624 Fax 317.898.6636 that occupies space within the tarsal tunnel region may cause NEW CASTLE pressure on the nerve and subsequent symptoms. -

Focal Entrapment Neuropathies in Diabetes
Reviews/Commentaries/Position Statements REVIEW ARTICLE Focal Entrapment Neuropathies in Diabetes 1 1 AARON VINIK, MD, PHD LAWRENCE COLEN, MD millimeters]) is a risk factor (8,9). It used 1 2 ANAHIT MEHRABYAN, MD ANDREW BOULTON, MD to be associated with work-related injury, but now seems to be common in people in sedentary positions and is probably re- lated to the use of keyboards and type- MONONEURITIS AND because the treatment may be surgical (2) writers (dentists are particularly prone) ENTRAPMENT SYNDROMES — (Table 1). (10). As a corollary, recent data (3) in 514 Peripheral neuropathies in diabetes are a patients with CTS suggest that there is a diverse group of syndromes, not all of CARPAL TUNNEL threefold risk of having diabetes com- which are the common distal symmetric SYNDROME — Carpal tunnel syn- pared with a normal control group. If rec- polyneuropathy. The focal and multifocal drome (CTS) is the most common entrap- ognized, the diagnosis can be confirmed neuropathies are confined to the distribu- ment neuropathy encountered in diabetic by electrophysiological studies. Therapy tion of single or multiple peripheral patients and occurs as a result of median is simple, with diuretics, splints, local ste- nerves and their involvement is referred nerve compression under the transverse roids, and rest or ultimately surgical re- to as mononeuropathy or mononeuritis carpal ligament. It occurs thrice as fre- lease (11). The unaware physician seldom multiplex. quently in a diabetic population com- realizes that symptoms may spread to the Mononeuropathies are due to vasculitis pared with a normal healthy population whole hand or arm in CTS, and the signs and subsequent ischemia or infarction of (3,4). -

ICD9 & ICD10 Neuromuscular Codes
ICD-9-CM and ICD-10-CM NEUROMUSCULAR DIAGNOSIS CODES ICD-9-CM ICD-10-CM Focal Neuropathy Mononeuropathy G56.00 Carpal tunnel syndrome, unspecified Carpal tunnel syndrome 354.00 G56.00 upper limb Other lesions of median nerve, Other median nerve lesion 354.10 G56.10 unspecified upper limb Lesion of ulnar nerve, unspecified Lesion of ulnar nerve 354.20 G56.20 upper limb Lesion of radial nerve, unspecified Lesion of radial nerve 354.30 G56.30 upper limb Lesion of sciatic nerve, unspecified Sciatic nerve lesion (Piriformis syndrome) 355.00 G57.00 lower limb Meralgia paresthetica, unspecified Meralgia paresthetica 355.10 G57.10 lower limb Lesion of lateral popiteal nerve, Peroneal nerve (lesion of lateral popiteal nerve) 355.30 G57.30 unspecified lower limb Tarsal tunnel syndrome, unspecified Tarsal tunnel syndrome 355.50 G57.50 lower limb Plexus Brachial plexus lesion 353.00 Brachial plexus disorders G54.0 Brachial neuralgia (or radiculitis NOS) 723.40 Radiculopathy, cervical region M54.12 Radiculopathy, cervicothoracic region M54.13 Thoracic outlet syndrome (Thoracic root Thoracic root disorders, not elsewhere 353.00 G54.3 lesions, not elsewhere classified) classified Lumbosacral plexus lesion 353.10 Lumbosacral plexus disorders G54.1 Neuralgic amyotrophy 353.50 Neuralgic amyotrophy G54.5 Root Cervical radiculopathy (Intervertebral disc Cervical disc disorder with myelopathy, 722.71 M50.00 disorder with myelopathy, cervical region) unspecified cervical region Lumbosacral root lesions (Degeneration of Other intervertebral disc degeneration, -

Lower Extremity Focal Neuropathies
LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Arturo A. Leis, MD S.H. Subramony, MD Vettaikorumakankav Vedanarayanan, MD, MBBS Mark A. Ross, MD AANEM 59th Annual Meeting Orlando, Florida Copyright © September 2012 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 Printed by Johnson Printing Company, Inc. 1 Please be aware that some of the medical devices or pharmaceuticals discussed in this handout may not be cleared by the FDA or cleared by the FDA for the specific use described by the authors and are “off-label” (i.e., a use not described on the product’s label). “Off-label” devices or pharmaceuticals may be used if, in the judgment of the treating physician, such use is medically indicated to treat a patient’s condition. Information regarding the FDA clearance status of a particular device or pharmaceutical may be obtained by reading the product’s package labeling, by contacting a sales representative or legal counsel of the manufacturer of the device or pharmaceutical, or by contacting the FDA at 1-800-638-2041. 2 LOWER EXTREMITY FOCAL NEUROPATHIES Lower Extremity Focal Neuropathies Table of Contents Course Committees & Course Objectives 4 Faculty 5 Basic and Special Nerve Conduction Studies of the Lower Limbs 7 Arturo A. Leis, MD Common Peroneal Neuropathy and Foot Drop 19 S.H. Subramony, MD Mononeuropathies Affecting Tibial Nerve and its Branches 23 Vettaikorumakankav Vedanarayanan, MD, MBBS Femoral, Obturator, and Lateral Femoral Cutaneous Neuropathies 27 Mark A. Ross, MD CME Questions 33 No one involved in the planning of this CME activity had any relevant financial relationships to disclose. -

Tarsal Tunnel Syndrome Masked by Painful Diabetic Polyneuropathy
CASE REPORT – OPEN ACCESS International Journal of Surgery Case Reports 15 (2015) 103–106 CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector Contents lists available at ScienceDirect International Journal of Surgery Case Reports journa l homepage: www.casereports.com Tarsal tunnel syndrome masked by painful diabetic polyneuropathy a,∗ b c Tugrul Ormeci , Mahir Mahirogulları , Fikret Aysal a Medipol University, Faculty of Medicine, Department of Radiology, Istanbul,˙ Turkey b Medipol University, Faculty of Medicine, Department of Orthopedics and Traumatology, Istanbul,˙ Turkey c Medipol University, Faculty of Medicine, Department of Neurology, Istanbul,˙ Turkey a r a t b i c l e i n f o s t r a c t Article history: INTRODUCTION: Various causes influence the etiology of tarsal tunnel syndrome including systemic Received 3 July 2015 diseases with progressive neuropathy, such as diabetes. Received in revised form 5 August 2015 PRESENTATION OF CASE: We describe a 52-year-old male patient with complaints of numbness, burning Accepted 21 August 2015 sensation and pain in both feet. The laboratory results showed that the patient had uncontrolled diabetes, Available online 28 August 2015 and the EMG showed distal symmetrical sensory-motor neuropathy and nerve entrapment at the right. Ultrasonography and MRI showed the cyst in relation to medial plantar nerve, and edema- moderate Keywords: atrophy were observed at the distal muscles of the foot. Tarsal tunnel syndrome DISCUSSION: Foot neuropathy in diabetic patients is a complex process. So, in planning the initial treat- Diabetic polyneuropathy Pain ment, medical or surgical therapy is selected based on the location and type of the pathology. -

Plantar Fasciitis Exercises
Accurate Clinic 2401 Veterans Memorial Blvd. Suite16 Kenner, LA 70062 - 4799 Phone: 504.472.6130 Fax: 504.472.6128 www.AccurateClinic.com Plantar Fasciitis Exercise Getting the right plantar fasciitis exercise is imperative to ensure the injury doesn’t continue to affect performance. If not given the attention it needs, plantar fasciitis can flair up long after an athlete thinks they’ve recovered and badly damage training plans and competition aspirations. What is plantar fascia? Plantar fascia is a thick, fibrous band of connective tissue which originates at the heel bone and runs along the bottom of the foot in a fan-like manner, attaching to the base of each of the toes. A rather tough, resilient structure, the plantar fascia takes on a number of critical functions during running and walking. Although the fascia is invested with countless sturdy 'cables' of connective tissue called collagen fibres, it is certainly not immune to injury. In fact, about 5 to 10 per cent of all running injuries are inflammations of the fascia, an incidence rate which in the United States would produce about a million cases of plantar fasciitis per year, just among runners and joggers. Basketball players, tennis players, volleyballers, step-aerobics participants, and dancers are also prone to plantar problems, as are non-athletic people who spend a lot of time on their feet or suddenly become active after a long period of lethargy. Why does the fascia flare up? Although it is a fairly rugged structure, the plantar fascia is not very receptive to stretching, and yet stretching occurs in the fascia nearly every time the foot hits the ground. -

Tarsal Tunnel Syndrome Secondary to the Posterior Tibial Nerve Schwannoma
Case Report http://dx.doi.org/10.12972/The Nerve.2015.01.01.034 www.thenerve.net Tarsal Tunnel Syndrome Secondary to the Posterior Tibial Nerve Schwannoma Jung Won Song1, Sung Han Oh1, Pyung Goo Cho1, Eun Mee Han2 Departments of 1Neurosurgey, 2Pathology, Bundang Jesaeng General Hospital, Seongnam, Korea A 77-year-old female presented with complaint of burning pain and paresthesia along the medial aspect of ankle, heel and sole of the left foot. An ankle MRI, electromyelogram (EMG) with nerve conduction velocity (NCV) and pathologic findings were all compatible with Tarsal tunnel syndrome caused by the posterior tibial nerve Schwannoma. Operative release of the Tarsal tunnel and surgical excision of Schwannoma were performed under the microscopy. It is necessary to have a possible lump in mind when Tarsal tunnel syndrome is suspected, such as posterior tibial nerve Schwannoma. Key Words: Posterior Tibial NerveㆍSchwannomaㆍTarsal Tunnel Syndrome diagnose neurofibromatosis was insufficient. An ankle magne- tic resonance imaging (MRI) revealed about a 22×19×9 mm- INTRODUCTION sized ovoid soft tissue mass in the posterior ankle connected to the posterior tibial nerve. The mass lies beneath the flexor Although Schwannomas are the most common peripheral retinaculum of ankle and showed relatively strong enhance- nerve sheath tumor, Schwannoma of the posterior tibial nerve ment (Fig. 1). and it branch is a rare etiology causing Tarsal tunnel syndrome. The NCV study showed no response sensory nerve action We report a case of Tarsal tunnel syndrome caused by the pos- potentials of the left medial and lateral plantar nerves. Motor terior tibial nerve Schwannoma and mention surgical strategy conduction study of the deep peroneal and tibial nerves was with literature review.