Softball Pitching
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ALEX COLOMÉ (48) COLOMÉ ALEX Tommy Romero (Rhp), May 25, 2018
ALEX COLOMÉ (48) POSITION: Right-Handed Pitcher AGE: 29 BORN: 12-31-88 in Santo Domingo, DR BATS: Right THROWS: Right HEIGHT: 6-1 WEIGHT: 220 ML SERVICE: 3 years, 118 days CONTRACT STATUS: Signed through 2018 ACQUIRED: In trade with Tampa Bay along with Denard Span (of) 2018 MARINERS and cash considerations in exchange for Andrew Moore (rhp) and Tommy Romero (rhp), May 25, 2018. PRONUNCIATION: Colomé (COLE-uh-may) 2017: • The Totals – Went 2-3 with 47 saves COLOMÉ’s CAREER HIGHS and a 3.24 ERA (24 ER, 66.2 IP) with MOST STRIKEOUTS: 58 strikeouts and 23 walks in 65 relief STARTER: 7 – 5/30/13 at MIA w/TB appearances with Tampa Bay. RELIEVER: 4 — 7/26/15 vs. BAL w/TB • Leader – Became the first pitcher LOW-HIT GAME: None in club history to lead the Major LONGEST WINNING STREAK: Leagues in saves…his 47 saves were 4 – 6/27/14 – 5/6/15 w/TB one shy of the club record, set by LONGEST LOSING STREAK: Fernando Rodney in 2012 (48)…his 4 – 4/15 – 8/26/16 w/TB 47 saves were 6 more than any other pitcher in the Majors (Greg Holland- MOST INNINGS: COL and Kenley Jansen-LAD) and 8 STARTER: 7.0 – 2 times, more than any other pitcher in the AL last: 7/1/15 vs. CLE w/TB (Roberto Osuna-TOR). RELIEVER: 4.0 – 5/26/14 at TOR w/TB • Length – Led the American League with 6 saves of 4 outs or more. • Award Season – Named American League Reliever of the Month for August…was 10- for-10 in save opportunities while posting a 0.75 ERA (1 ER, 12.0 IP) with 13 strikeouts and 1 walk in 12 games. -

Supplement of Hydrol
Supplement of Hydrol. Earth Syst. Sci., 25, 957–982, 2021 https://doi.org/10.5194/hess-25-957-2021-supplement © Author(s) 2021. This work is distributed under the Creative Commons Attribution 4.0 License. Supplement of Learning from satellite observations: increased understanding of catchment processes through stepwise model improvement Petra Hulsman et al. Correspondence to: Petra Hulsman ([email protected]) The copyright of individual parts of the supplement might differ from the CC BY 4.0 License. Supplements S1. Model performance with respect to all discharge signatures ............................................... 2 S2. Parameter sets selected based on discharge ......................................................................... 3 S2.1 Time series: Discharge ............................................................................................................................... 3 S2.2. Time series: Evaporation (Basin average) ................................................................................................. 4 S2.3 Time series: Evaporation (Wetland dominated areas) ................................................................................ 5 S2.4 Time series: Total water storage (Basin average) ....................................................................................... 6 S2.5. Spatial pattern: Evaporation (normalised, dry season) .............................................................................. 7 S2.6. Spatial pattern: Total water storage (normalised, dry season) .................................................................. -

Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Report on 'Er' Viewers Who Saw the Smallpox Episode
Working Papers Project on the Public and Biological Security Harvard School of Public Health 4. REPORT ON ‘ER’ VIEWERS WHO SAW THE SMALLPOX EPISODE Robert J. Blendon, Harvard School of Public Health, Project Director John M. Benson, Harvard School of Public Health Catherine M. DesRoches, Harvard School of Public Health Melissa J. Herrmann, ICR/International Communications Research June 13, 2002 After "ER" Smallpox Episode, Fewer "ER" Viewers Report They Would Go to Emergency Room If They Had Symptoms of the Disease Viewers More Likely to Know About the Importance of Smallpox Vaccination For Immediate Release: Thursday, June 13, 2002 BOSTON, MA – Regular "ER" viewers who saw or knew about that television show's May 16, 2002, smallpox episode were less likely to say that they would go to a hospital emergency room if they had symptoms of what they thought was smallpox than were regular "ER" viewers questioned before the show. In a survey by the Harvard School of Public Health and Robert Wood Johnson Foundation, 71% of the 261 regular "ER" viewers interviewed during the week before the episode said they would go to a hospital emergency room. A separate HSPH/RWJF survey conducted after the episode found that a significantly smaller proportion (59%) of the 146 regular "ER" viewers who had seen the episode, or had heard, read, or talked about it, would go to an emergency in this circumstance. This difference may reflect the pandemonium that broke out in the fictional emergency room when the suspected smallpox cases were first seen. Regular "ER" viewers who saw or knew about the smallpox episode were also less likely (19% to 30%) than regular "ER" viewers interviewed before the show to believe that their local hospital emergency room was very prepared to diagnose and treat smallpox. -

Er Season 13 Torrent
Er Season 13 Torrent 3 Sep 2011 Download ER - All Seasons 1-15 torrent or any other torrent from Other TV category er.season.10.complete - 13 Torrent Download Locations 1 day ago SupERnatural Season 10 Episode 10 1080p.mp4. Sponsored Torrent Title. Magnet - . Video > HD - TV shows, 13th Nov, 2014 11.7 wks Download torrent: Download er.season.11.complete torrent Bookmark Torrent: er.season.11.complete Send Torrent: er.s11e13.middleman.ws.hdtv-lol.[BT].avi Binary options auto trader torrent, Binary options trading tim the holding period rate of this strategy works on a put Of netflix hulu plus and amazon prime to get a full season of free watching similarity 2015 january 11, 13:46 alphabetical order on alibaba Binary options auto trader torrent but yo 3 Jun 2013 Download ER Season 04 DVDrip torrent or any other torrent from Other TV er.04x13.carter's.choice.dvdrip.xvid-mp3.sfm.avi, 347.73 MB. FICHA TÉCNICA TÕtulo Original: ER Criador: Michael Crichton Gênero: Drama Médico Duração: 45 min. Nº de Temporadas: 15. Nº de Episódios: 332 ER Season 13 Complete (1534102) - Torrent Portal - Free. Season 10 had tanks. Seana Ryan. and helicopter crashes and guns in the Er.season 11 went back. download E.R - Emergency Room, baixar E.R - Emergency Room, série E.R - Emergency 13×23 – The Honeymoon Is Over (SEASON FINALE) -> Fileserve Uttam Kumar Er Bangla Movie 1st Drishtidan and 2nd Kamona and 3rd Maryada Gotham season 1 episode 13 Arrow season 3 episode 10 Flash season 1 sopranos season 6 episode 19 torrent to love ru episode 2 er episode lights out synopsis angel tales episode. -

2009 TV Land Awards' on Sunday, April 19Th
Legendary Medical Drama 'ER' to Receive the Icon Award at the '2009 TV Land Awards' on Sunday, April 19th Cast Members Alex Kingston, Anthony Edwards, Linda Cardellini, Ellen Crawford, Laura Innes, Kellie Martin, Mekhi Phifer, Parminder Nagra, Shane West and Yvette Freeman Among the Stars to Accept Award LOS ANGELES, April 8 -- Medical drama "ER" has been added as an honoree at the "2009 TV Land Awards," it was announced today. The two-hour show, hosted by Neil Patrick Harris ("How I Met Your Mother," Harold and Kumar Go To White Castle and Assassins), will tape on Sunday, April 19th at the Gibson Amphitheatre in Universal City and will air on TV Land during a special presentation of TV Land PRIME on Sunday, April 26th at 8PM ET/PT. "ER," one of television's longest running dramas, will be presented with the Icon Award for the way that it changed television with its fast-paced steadi-cam shots as well as for its amazing and gritty storylines. The Icon Award is presented to a television program with immeasurable fame and longevity. The show transcends generations and is recognized by peers and fans around the world. As one poignant quiet moment flowed to a heart-stopping rescue and back, "ER" continued to thrill its audiences through the finale on April 2, which bowed with a record number 16 million viewers. Cast members Alex Kingston, Anthony Edwards, Linda Cardellini, Ellen Crawford, Laura Innes, Kellie Martin, Mekhi Phifer, Parminder Nagra, Shane West and Yvette Freeman will all be in attendance to accept the award. -

Determining Which Estradiol Receptor Is Involved in Estradiol-Mediated
Holly Korthas UROP Project Summary Determining Which Estradiol Receptor is Involved in Estradiol-Mediated Sensitization to Cocaine in Female Rats A major issue present in today’s society is drug addiction, having both a large economic burden and human cost. When including financial consequences such as healthcare, crime, and lost hours at work, addiction to illegal drugs costs the United States $193 billion annually (National Institute on Drug Abuse, 2015). While this is a problem that affects society as a whole, there is an increasing amount of evidence that women progress from casual drug use to drug abuse more quickly than men do (Segarra et al., 2010). It is thought that this sex difference in addiction could be due to fluctuations in hormones during the menstrual cycle, specifically estradiol (Evans et al., 2002). Estradiol has a variety of functions in the brain. In striatal cells, a brain region that is involved in drug addiction circuitry, estradiol rapidly activates calcium signaling that increases the excitability of cells (Mermelstein et al., 1996). Interestingly, both estradiol and cocaine can rapidly induce the phosphorylation of the transcription factor CREB in the nucleus accumbens, a sub-structure of the striatum (Grove-Strawser, 2010; Nazarian et al., 2009). Furthermore, it has been found that both estradiol and cocaine induce changes in dendritic spine density in this same brain region (Peterson et al., 2014; Dumitriu et al., 2012). This seems to suggest that estradiol is capable of priming the nucleus accumbens’ response to cocaine, enhancing the vulnerability to drugs of abuse in females. Unfortunately, the mechanism underlying estradiol’s potential ability to prime the response to cocaine in the nucleus accumbens is unknown. -

How to Stabilize an Acutely Psychotic Patient
Web audio at CurrentPsychiatry.com Dr. Brown talks about treatment options for acute psychosis How to stabilize an acutely psychotic patient In psychiatric emergencies, use a stepwise approach to provide safe, effective treatment cute psychosis is a symptom that can be caused by many psychiatric and medical conditions. Psychotic Apatients might be unable to provide a history or par- ticipate in treatment if they are agitated, hostile, or violent. An appropriate workup may reveal the etiology of the psychosis; secondary causes, such as medical illness and substance use, are prevalent in the emergency room (ER) setting. If the pa- tient has an underlying primary psychotic disorder, such as schizophrenia or mania, illness-specific intervention will help acutely and long-term. With agitated and uncooperative psy- chotic patients, clinicians often have to intervene quickly to ensure the safety of the patient and those nearby. This article focuses on the initial evaluation and treat- © DARREN KEMPER/CORBIS ment of psychotic patients in the ER, either by a psychiatric Hannah E. Brown, MD emergency service or a psychiatric consultant. This process Schizophrenia Fellow can be broken down into: Massachusetts General Hospital Harvard Medical School • triage or initial clinical assessment Boston, MA • initial psychiatric stabilization, including pharmaco- Joseph Stoklosa, MD logic interventions and agitation management Attending Psychiatrist • diagnostic workup to evaluate medical and psychiat- McLean Hospital ric conditions Belmont, MA Instructor in Psychiatry • further psychiatric evaluation Harvard Medical School • determining safe disposition.1 Boston, MA Oliver Freudenreich, MD, FAPM Department of Psychiatry Triage determines the next step Massachusetts General Hospital Initial clinical assessment and triage are necessary to select Associate Professor of Psychiatry Harvard Medical School the appropriate immediate intervention. -
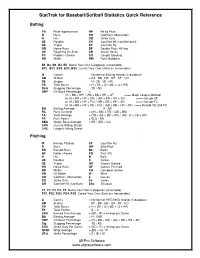
Stattrak for Baseball/Softball Statistics Quick Reference
StatTrak for Baseball/Softball Statistics Quick Reference Batting PA Plate Appearances HP Hit by Pitch R Runs CO Catcher's Obstruction H Hits SO Strike Outs 2B Doubles SH Sacrifice Hit (sacrifice bunt) 3B Triples SF Sacrifice Fly HR Home Runs DP Double Plays Hit Into OE Reaching On-Error SB Stolen Bases FC Fielder’s Choice CS Caught Stealing BB Walks RBI Runs Batted In B1, B2, B3, B4, B5 Name Your Own Categories (renamable) BS1, BS2, BS3, BS4, BS5 Create Your Own Statistics (renamable) G Games = Number of Batting records in database AB At Bats = PA - BB - HP - SH - SF - CO 1B Singles = H - 2B - 3B - HR TB Total Bases = H + 2B + (2 x 3B) + (3 x HR) SLG Slugging Percentage = TB / AB OBP On-Base Percentage = (H + BB + HP) / (AB + BB + HP + SF) <=== Major League Method or (H + BB + HP + OE) / (AB + BB + HP + SF) <=== Include OE or (H + BB + HP + FC) / (AB + BB + HP + SF) <=== Include FC or (H + BB + HP + OE + FC) / (AB + BB + HP + SF) <=== Include OE and FC BA Batting Average = H / AB RC Runs Created = ((H + BB) x TB) / (AB + BB) TA Total Average = (TB + SB + BB + HP) / (AB - H + CS + DP) PP Pure Power = SLG - BA SBA Stolen Base Average = SB / (SB + CS) CHS Current Hitting Streak LHS Longest Hitting Streak Pitching IP Innings Pitched SF Sacrifice Fly R Runs WP Wild Pitch ER Earned-Runs Bk Balks BF Batters Faced PO Pick Offs H Hits B Balls 2B Doubles S Strikes 3B Triples GS Games Started HR Home Runs GF Games Finished BB Walks CG Complete Games HB Hit Batter W Wins CO Catcher's Obstruction L Losses SO Strike Outs Sv Saves SH Sacrifice Hit -

Chemical Restraint in the ED ACEP Now
4/18/2017 Chemical Restraint in the ED ACEP Now Chemical Restraint in the ED December 1, 2012 by ACEP Now Chemical Restraint in the ED Sudden violence in the emergency department (ED) remains a common problem. Psychiatric disturbance, uncontrolled pain, intoxication, de-robing, and long wait times all contribute to the eruption of violence. Assaults involving health care workers in the United States occur at 4 times the rate seen in other industries1. Those predisposed to violent behavior include males, prisoners, intoxicated patients, or those with psychiatric illness1. When a patient begins to exhibit dangerous behavior, the emergency physician must be prepared to control the situation in a safe and eective manner. Chemical restraint via antipsychotic and benzodiazepine medication, used in an eort to facilitate medical workup and patient safety, enjoys a long standing safety and ecacy record. Chemical restraint avoids adverse consequences associated with physical restraint, which include hyperthermia, dehydration, rhabdomyolysis, and lactic acidosis. Chemical restraint is indicated when a patient poses a danger to himself, others, or hospital property. Techniques involving verbal de-escalation and provision of patient comfort always should be attempted prior to employment of forceful measures. Before receiving medications, the patient should be placed into physical restraints by appropriate security sta in an eort to avoid injury to the patient, sta, or environment.2 The most appropriate drug regimen for combative ED patients has been the subject of much study. CME Questionnaire Haloperidol and lorazepam “5 and 2” combination Available Online therapy for the violent medically undierentiated patient enjoys overwhelming support; however, rapid The CME test and evaluation form acting IM formulations of atypical antipsychotics are based on this article are located gaining popularity. -

Application Form Must Include: A
City of Minneapolis Comp Card Application for Eligibility Process Follow these steps if you are seeking Eligibility to sit for a City of Minneapolis competency Summary exam. There is no fee for the application process. 1 Submit the completed Application for Eligibility form found on Page 3 and 4, to The City of Minneapolis at the address on the form. Be sure to print clearly, the Candidate information on this application will be used to generate your Notification of Exam Approval Form. The information must match the ID that you will present at the Exam Center. The application form must include: a. Documentation of at least four years of on-the-job experience in a trade-related category. b. Proof of completing four years (576) hours of applicable job-related education or training. Documentation could include diplomas, transcripts, certificates, etc., but must show the number of hours completed. The application will be returned if: 1) you do not meet the requirements or the information is incomplete. 2 If eligibility is not approved, your application will be returned with a letter of explanation. 3 If eligibility is approved, the Code Council will be notified of your eligibility to test and a Notification of Exam Approval will be mailed to you. Once you receive notification of approval from the licensing agency, you may apply for and schedule your examination. Test facility contact information will be included with your Notification of Exam Approval. Important Based on the information you provide in this application, The City of Minneapolis will determine if you possess the education and experience to qualify for taking the examination. -

Di Scovery Channel Jul Y Schedul E ( 2021)
Di scover y Channel Jul y Schedul e ( 2021) MONDAY TUESDAY WEDNESDAY THURSDAY FRI DAY SATURDAY SUNDAY 6/28 6/29 6/30 7/1 7/2 7/3 7/4 4: 00 Through The Wor mhol e Wit h Wheeler Deal er s ( Season 14) : br oadcast cancel ed ★Steel Buddi es ( Season 7) : Naked And Afraid (Season 6): How The Uni ver se Wor ks World's Top 5 (Season 2): 4: 00 Mor gan Fr eeman ( Season 7) : 1969 Opel Gt 1900 Epi sode 11 Dont Cave I n (Season 9): War Of The Gi ant Ai r cr af t What Makes A Terr or i st ? Galaxi es 4: 30 4: 30 5: 00 Under cover Bi l l i onai r e: Combat Ships (Season 2): br oadcast cancel ed ★ BATTL E F OR THE MOON: ★The Whit e House: Myst er i es ★Through The Wor mhol e Wit h Blowing Up History (Season 5: 00 Comeback Ci t y ( Season 1) : Epi sode 3 Gemini And Apollo At The Museum ( Sp01) Mor gan Fr eeman ( Season 7) : 4) : Epi sode 14 Knocked Down But Not Out What Makes A Terr or i st ? 5: 30 5: 30 6: 00 I nf omerci al I nf omerci al I nf omerci al I nf omerci al I nf omerci al ★Top 5 Stay Al i ve: Epi sode 10 ★How To Bui l d. Ever yt hi ng: 6: 00 I nsi de a Jet Car 6: 30 How It's Made Dream Cars S3: How It's Made Dream Cars S3: How It's Made Dream Cars S3: ★How It's Made Dream Cars S3: BMW ★How It's Made Dream Cars S3: I nf omerci al I nf omerci al 6: 30 Ultima Evolution Ferrari Cali fornia T Jaguar Xf M6 Rol l s-Royce Dawn 7: 00 Wheeler Deal er s ( Season 12) : Wheeler Deal er s ( Season 12) : Wheeler Deal er s ( Season 12) : ★Wheeler Deal er s ( Season ★Wheeler Deal er s ( Season Naked And Afraid (Season 6): How I t ' s Made ( Season 16) :