How to Stabilize an Acutely Psychotic Patient
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Trusted Resources in Psychiatry Save 25% When You Order Today!
Trusted Resources in Psychiatry Save 25% when you order today! See page 5 MUST-HAVE RESOURCES for NEW Kaplan & Sadock’s Synopsis of Psychotherapy: A Practical Introduction Psychiatry, 12e 978-1-9751-2678-0 Offering unique, essential coverage of the theoretical foundations and core techniques of a variety of psychotherapies, Psychotherapy: A Practical Introduction is a one-stop resource for psychiatry residents and psychiatrists beginning practice, as well as graduate trainees in psychology and clinical social work. This practical reference is an invaluable tool for understanding the common approaches fundamental to all therapies, exploring the most frequently used therapy approaches, learning evidence-based approaches for making treatment decisions, and engaging patients in safe and effective psychotherapies, regardless of treatment setting. For faculty instructors, this brand new resource provides a readable, highly applicable core textbook for any introductory psychotherapy course or psychotherapy didactic series. Buy Now! Medical Marijuana: A Clinical Handbook 978-1-9751-4189-9 Written by experienced clinicians for practicing physicians and other health care providers, this timely handbook presents today’s available information on cannabis and its uses in all areas of patient care. Medical Marijuana: A Clinical Handbook summarizes what is currently known about the positive and negative health impacts of cannabis, detailed pharmacological profiles of both THC and CBD, considerations for each medical specialty, treatment approaches used by practicing clinicians, and insights into the history of cannabis and the current regulatory environment in the United States. This concise, easy-to-navigate guide is an invaluable resource for physicians and residents, nurse practitioners, pharmacists, and other clinicians who seek reliable clinical guidelines in this growing area of health care. -

Autism Practice Parameters
American Academy of Child and Adolescent Psychiatry AACAP is pleased to offer Practice Parameters as soon as they are approved by the AACAP Council, but prior to their publication in the Journal of the American Academy of Child and Adolescent Psychiatry (JAACAP). This article may be revised during the JAACAP copyediting, author query, and proof reading processes. Any final changes in the document will be made at the time of print publication and will be reflected in the final electronic version of the Practice Parameter. AACAP and JAACAP, and its respective employees, are not responsible or liable for the use of any such inaccurate or misleading data, opinion, or information contained in this iteration of this Practice Parameter. PRACTICE PARAMETER FOR THE ASSESSMENT AND TREATMENT OF CHILDREN AND ADOLESCENTS WITH AUTISM SPECTRUM DISORDER ABSTRACT Autism spectrum disorder (ASD) is characterized by patterns of delay and deviance in the development of social, communicative, and cognitive skills which arise in the first years of life. Although frequently associated with intellectual disability, this condition is distinctive in terms of its course, impact, and treatment. ASD has a wide range of syndrome expression and its management presents particular challenges for clinicians. Individuals with an ASD can present for clinical care at any point in development. The multiple developmental and behavioral problems associated with this condition necessitate multidisciplinary care, coordination of services, and advocacy for individuals and their families. Early, sustained intervention and the use of multiple treatment modalities are indicated. Key Words: autism, practice parameters, guidelines, developmental disorders, pervasive developmental disorders. ATTRIBUTION This parameter was developed by Fred Volkmar, M.D., Matthew Siegel, M.D., Marc Woodbury-Smith, M.D., Bryan King, M.D., James McCracken, M.D., Matthew State, M.D., Ph.D. -

ALEX COLOMÉ (48) COLOMÉ ALEX Tommy Romero (Rhp), May 25, 2018
ALEX COLOMÉ (48) POSITION: Right-Handed Pitcher AGE: 29 BORN: 12-31-88 in Santo Domingo, DR BATS: Right THROWS: Right HEIGHT: 6-1 WEIGHT: 220 ML SERVICE: 3 years, 118 days CONTRACT STATUS: Signed through 2018 ACQUIRED: In trade with Tampa Bay along with Denard Span (of) 2018 MARINERS and cash considerations in exchange for Andrew Moore (rhp) and Tommy Romero (rhp), May 25, 2018. PRONUNCIATION: Colomé (COLE-uh-may) 2017: • The Totals – Went 2-3 with 47 saves COLOMÉ’s CAREER HIGHS and a 3.24 ERA (24 ER, 66.2 IP) with MOST STRIKEOUTS: 58 strikeouts and 23 walks in 65 relief STARTER: 7 – 5/30/13 at MIA w/TB appearances with Tampa Bay. RELIEVER: 4 — 7/26/15 vs. BAL w/TB • Leader – Became the first pitcher LOW-HIT GAME: None in club history to lead the Major LONGEST WINNING STREAK: Leagues in saves…his 47 saves were 4 – 6/27/14 – 5/6/15 w/TB one shy of the club record, set by LONGEST LOSING STREAK: Fernando Rodney in 2012 (48)…his 4 – 4/15 – 8/26/16 w/TB 47 saves were 6 more than any other pitcher in the Majors (Greg Holland- MOST INNINGS: COL and Kenley Jansen-LAD) and 8 STARTER: 7.0 – 2 times, more than any other pitcher in the AL last: 7/1/15 vs. CLE w/TB (Roberto Osuna-TOR). RELIEVER: 4.0 – 5/26/14 at TOR w/TB • Length – Led the American League with 6 saves of 4 outs or more. • Award Season – Named American League Reliever of the Month for August…was 10- for-10 in save opportunities while posting a 0.75 ERA (1 ER, 12.0 IP) with 13 strikeouts and 1 walk in 12 games. -

Supplement of Hydrol
Supplement of Hydrol. Earth Syst. Sci., 25, 957–982, 2021 https://doi.org/10.5194/hess-25-957-2021-supplement © Author(s) 2021. This work is distributed under the Creative Commons Attribution 4.0 License. Supplement of Learning from satellite observations: increased understanding of catchment processes through stepwise model improvement Petra Hulsman et al. Correspondence to: Petra Hulsman ([email protected]) The copyright of individual parts of the supplement might differ from the CC BY 4.0 License. Supplements S1. Model performance with respect to all discharge signatures ............................................... 2 S2. Parameter sets selected based on discharge ......................................................................... 3 S2.1 Time series: Discharge ............................................................................................................................... 3 S2.2. Time series: Evaporation (Basin average) ................................................................................................. 4 S2.3 Time series: Evaporation (Wetland dominated areas) ................................................................................ 5 S2.4 Time series: Total water storage (Basin average) ....................................................................................... 6 S2.5. Spatial pattern: Evaporation (normalised, dry season) .............................................................................. 7 S2.6. Spatial pattern: Total water storage (normalised, dry season) .................................................................. -
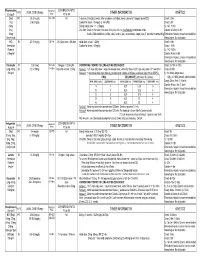
Medication Conversion Chart
Fluphenazine FREQUENCY CONVERSION RATIO ROUTE USUAL DOSE (Range) (Range) OTHER INFORMATION KINETICS Prolixin® PO to IM Oral PO 2.5-20 mg/dy QD - QID NA ↑ dose by 2.5mg/dy Q week. After symptoms controlled, slowly ↓ dose to 1-5mg/dy (dosed QD) Onset: ≤ 1hr 1mg (2-60 mg/dy) Caution for doses > 20mg/dy (↑ risk EPS) Cmax: 0.5hr 2.5mg Elderly: Initial dose = 1 - 2.5mg/dy t½: 14.7-15.3hr 5mg Oral Soln: Dilute in 2oz water, tomato or fruit juice, milk, or uncaffeinated carbonated drinks Duration of Action: 6-8hr 10mg Avoid caffeinated drinks (coffee, cola), tannics (tea), or pectinates (apple juice) 2° possible incompatibilityElimination: Hepatic to inactive metabolites 5mg/ml soln Hemodialysis: Not dialyzable HCl IM 2.5-10 mg/dy Q6-8 hr 1/3-1/2 po dose = IM dose Initial dose (usual): 1.25mg Onset: ≤ 1hr Immediate Caution for doses > 10mg/dy Cmax: 1.5-2hr Release t½: 14.7-15.3hr 2.5mg/ml Duration Action: 6-8hr Elimination: Hepatic to inactive metabolites Hemodialysis: Not dialyzable Decanoate IM 12.5-50mg Q2-3 wks 10mg po = 12.5mg IM CONVERTING FROM PO TO LONG-ACTING DECANOATE: Onset: 24-72hr (4-72hr) Long-Acting SC (12.5-100mg) (1-4 wks) Round to nearest 12.5mg Method 1: 1.25 X po daily dose = equiv decanoate dose; admin Q2-3wks. Cont ½ po daily dose X 1st few mths Cmax: 48-96hr 25mg/ml Method 2: ↑ decanoate dose over 4wks & ↓ po dose over 4-8wks as follows (accelerate taper for sx of EPS): t½: 6.8-9.6dy (single dose) ORAL DECANOATE (Administer Q 2 weeks) 15dy (14-100dy chronic administration) ORAL DOSE (mg/dy) ↓ DOSE OVER (wks) INITIAL DOSE (mg) TARGET DOSE (mg) DOSE OVER (wks) Steady State: 2mth (1.5-3mth) 5 4 6.25 6.25 0 Duration Action: 2wk (1-6wk) Elimination: Hepatic to inactive metabolites 10 4 6.25 12.5 4 Hemodialysis: Not dialyzable 20 8 6.25 12.5 4 30 8 6.25 25 4 40 8 6.25 25 4 Method 3: Admin equivalent decanoate dose Q2-3wks. -

Psychiatric Emergency & Crisis Services
APA Task Force on Psychiatric Emergency Services Michael H. Allen, M.D., Chair Peter Forster, M.D. Joseph Zealberg, M.D. Glenn Currier, M.D. Report and Recommendations Regarding Psychiatric Emergency and Crisis Services A Review and Model Program Descriptions August 2002 THE HISTORY OF THIS TASK FORCE AND A SUMMARY OF AVAILABLE DATA .........................4 Introduction ................................................................................................................................ 4 Toward "Organizationally Unique Treatment Facilities"........................................................... 4 Lack of Standards .................................................................................................................... 5 Funding Problems .................................................................................................................... 5 THE HISTORY OF THE TASK FORCE .....................................................................................7 A REVIEW OF THE LITERATURE ...........................................................................................8 Psychiatric Emergency Defined ............................................................................................... 8 Conceptualizing Emergency Services...................................................................................... 8 Hospital Based Services .......................................................................................................... 9 Consultation Liaison ............................................................................................................ -

Specificity of Psychosis, Mania and Major Depression in A
Molecular Psychiatry (2014) 19, 209–213 & 2014 Macmillan Publishers Limited All rights reserved 1359-4184/14 www.nature.com/mp ORIGINAL ARTICLE Specificity of psychosis, mania and major depression in a contemporary family study CL Vandeleur1, KR Merikangas2, M-PF Strippoli1, E Castelao1 and M Preisig1 There has been increasing attention to the subgroups of mood disorders and their boundaries with other mental disorders, particularly psychoses. The goals of the present paper were (1) to assess the familial aggregation and co-aggregation patterns of the full spectrum of mood disorders (that is, bipolar, schizoaffective (SAF), major depression) based on contemporary diagnostic criteria; and (2) to evaluate the familial specificity of the major subgroups of mood disorders, including psychotic, manic and major depressive episodes (MDEs). The sample included 293 patients with a lifetime diagnosis of SAF disorder, bipolar disorder and major depressive disorder (MDD), 110 orthopedic controls, and 1734 adult first-degree relatives. The diagnostic assignment was based on all available information, including direct diagnostic interviews, family history reports and medical records. Our findings revealed specificity of the familial aggregation of psychosis (odds ratio (OR) ¼ 2.9, confidence interval (CI): 1.1–7.7), mania (OR ¼ 6.4, CI: 2.2–18.7) and MDEs (OR ¼ 2.0, CI: 1.5–2.7) but not hypomania (OR ¼ 1.3, CI: 0.5–3.6). There was no evidence for cross-transmission of mania and MDEs (OR ¼ .7, CI:.5–1.1), psychosis and mania (OR ¼ 1.0, CI:.4–2.7) or psychosis and MDEs (OR ¼ 1.0, CI:.7–1.4). -
2021 Psychiatry CERT Content Specifications
CERTIFICATION EXAMINATION IN PSYCHIATRY Beginning in 2017, the American Board of Psychiatry and Neurology, Inc. (ABPN) issued two- dimensional content specifications for the psychiatry, neurology and child neurology certification examinations. Questions for the September 2021 psychiatry, neurology and child neurology certification examinations will conform to these content specifications. Within the two-dimensional format, one dimension is comprised of disorders and topics while the other is comprised of competencies and mechanisms that cut across the various disorders of the first dimension. By design, the two dimensions are interrelated and not independent of each other. All of the questions on the examination will fall into one of the disorders/topics and will be aligned with a competency/mechanism. For example, an item on substance use could focus on treatment, or it could focus on systems-based practice. The psychiatry, neurology and child neurology content specifications can be accessed from the specialty certification section of our website. Candidates should use the detailed content specifications as a guide to prepare for a certification examination. Scores for these examinations will be reported in a standardized format rather than the previous percent correct format. Starting in 2018, all future examinations given by the ABPN will gradually conform to the two- dimensional content specification. The American Board of Psychiatry and Neurology, Inc. is a not-for-profit corporation dedicated to serving the public interest and the professions of psychiatry and neurology by promoting excellence in practice through certification and continuing certification processes. For more information, please contact us at [email protected] or visit our website at www.abpn.com. -

Comorbid Psychiatric Disorders in Children with Autism: Interview Development and Rates of Disorders
J Autism Dev Disord (2006) 36:849–861 DOI 10.1007/s10803-006-0123-0 ORIGINAL PAPER Comorbid Psychiatric Disorders in Children with Autism: Interview Development and Rates of Disorders Ovsanna T. Leyfer Æ Susan E. Folstein Æ Susan Bacalman Æ Naomi O. Davis Æ Elena Dinh Æ Jubel Morgan Æ Helen Tager-Flusberg Æ Janet E. Lainhart Published online: 15 July 2006 Ó Springer Science+Business Media, Inc. 2006 Abstract The Kiddie Schedule for Affective Disorders sample demonstrated a high prevalence of specific phobia, and Schizophrenia was modified for use in children and obsessive compulsive disorder, and ADHD. The rates of adolescents with autism by developing additional screening psychiatric disorder in autism are high and are associated questions and coding options that reflect the presentation of with functional impairment. psychiatric disorders in autism spectrum disorders. The modified instrument, the Autism Comorbidity Interview- Keywords Psychopathology Æ Autism Æ Psychiatric Present and Lifetime Version (ACI-PL), was piloted and interview Æ Comorbidity frequently diagnosed disorders, depression, ADHD, and OCD, were tested for reliability and validity. The ACI-PL provides reliable DSM diagnoses that are valid based on clinical psychiatric diagnosis and treatment history. The Children with autism frequently have problematic emo- tional reactions and behaviors along with the features that O. T. Leyfer Department of Psychological and Brain Sciences, University define autism. Disturbances of emotion, attention, activity, of Louisville, Louisville, KY, USA and thought, and associated behavioral problems occur in children with autism of all ages (Lainhart, 1999). It is not S. E. Folstein yet known how often these additional difficulties are due to Department of Psychiatry, Johns Hopkins University, Baltimore, MD, USA comorbid psychiatric disorders. -

First-Episode Psychosis: a Clinical Approach
J Am Board Fam Pract: first published as 10.3122/15572625-13-6-430 on 1 November 2000. Downloaded from First-Episode Psychosis: A Clinical Approach S. Charles Schulz, MD, Deanna Bass, MD, and Cynthia S. Vrabel, MD Background: Psychotic illnesses, such as schizophrenia and bipolar illness, are relatively common and clearly devastating diseases. Most scientific literature focuses on research and care of patients suffering from psychotic illnesses in the middle age-group; subsequently, the first episode or early stages of psy chotic illnesses have been relatively ignored, especially the issues of early diagnosis and inten-ention. The purpose of this article is to highlight issues of first-episode schizophrenia for the family physician and to discuss (1) diagnosis, (2) neuropsychiatry research, (3) new medications, and (4) family issues. Methods: To approach the issues of first-episode schizophrenia, we describe a case of a young woman who suffered her first episode of psychosis. Relevant literature related to the early stages of psychosis, including new pharmacologic treatments, is addressed. Results: This report of our patient, a 19-year-old woman, illustrates the problems of a long prodro mal phase of her illness, the use of medications that might have worsened her condition, and the suc cessful use of new antipsychotic medications. Her family's issues as the patient went through this phase of her illness and recovery are reviewed. Conclusions: Patients at the outset of a psychotic illness are frequently first seen by a family physi cian. Familiarity with current diagnostic criteria and effectiveness of new treatments can lead to im proved detection and overall outcome. -

Report on 'Er' Viewers Who Saw the Smallpox Episode
Working Papers Project on the Public and Biological Security Harvard School of Public Health 4. REPORT ON ‘ER’ VIEWERS WHO SAW THE SMALLPOX EPISODE Robert J. Blendon, Harvard School of Public Health, Project Director John M. Benson, Harvard School of Public Health Catherine M. DesRoches, Harvard School of Public Health Melissa J. Herrmann, ICR/International Communications Research June 13, 2002 After "ER" Smallpox Episode, Fewer "ER" Viewers Report They Would Go to Emergency Room If They Had Symptoms of the Disease Viewers More Likely to Know About the Importance of Smallpox Vaccination For Immediate Release: Thursday, June 13, 2002 BOSTON, MA – Regular "ER" viewers who saw or knew about that television show's May 16, 2002, smallpox episode were less likely to say that they would go to a hospital emergency room if they had symptoms of what they thought was smallpox than were regular "ER" viewers questioned before the show. In a survey by the Harvard School of Public Health and Robert Wood Johnson Foundation, 71% of the 261 regular "ER" viewers interviewed during the week before the episode said they would go to a hospital emergency room. A separate HSPH/RWJF survey conducted after the episode found that a significantly smaller proportion (59%) of the 146 regular "ER" viewers who had seen the episode, or had heard, read, or talked about it, would go to an emergency in this circumstance. This difference may reflect the pandemonium that broke out in the fictional emergency room when the suspected smallpox cases were first seen. Regular "ER" viewers who saw or knew about the smallpox episode were also less likely (19% to 30%) than regular "ER" viewers interviewed before the show to believe that their local hospital emergency room was very prepared to diagnose and treat smallpox. -

Workbook Psychiatry and Narcology
Kharkiv National Medical University Department of Psychiatry, Narcology and Medical Psychology WORKBOOK MANUAL FOR INDIVIDUAL WORK FOR MEDICAL STUDENTS PSYCHIATRY AND NARCOLOGY (Part 2) Student ___________________________________________________________ Faculty _________________________________________________________ Course _________________ Group _____________________________________ Kharkiv 2019 Затверджено вченою радою ХНМУ Протокол №5 від 23.05.2019 р. Psychiatry (Part 2) : workbook manual for individual work of students / I. Strelnikova, G. Samardacova, К. Zelenska – Kharkiv, 2019. – 103 p. Копіювання для розповсюдження в будь-якому вигляді частин або повністю можливо тільки з дозволу авторів навчального посібника. CLASS 7. NEUROTIC DISORDERS. CLINICAL FORMS. TREATMENT AND REHABILITATION. POSTTRAUMATIC STRESS DISORDER. TREATMENT AND REHABILITATION. Psychogenic diseases are a large and clinically varied group of diseases resulting from an effect of acute or long-term psychic traumas, which manifest themselves by both mental and somatoneurological disorders and, as a rule, are reversible. Psychogenic diseases are caused by a psychic trauma, i.e. some events which affect significant aspects of existence of the human being and result in deep psychological feelings. These may be subjectively significant events, i.e. those which are pathogenic for the majority of people. Besides, the psyche may be traumatized by conventionally pathogenic events, which cause feelings in an individual because of his peculiar hierarchy of values. Unfavorable psychogenic effects on the human being cause stress in him, i.e. a nonspecific reaction at the physiological, psychological and behavioural levels. Stress may exert some positive, mobilizing influence, but may result in disorganization of the organism activity. The stress, which exerts a negative influence and causes various disturbances and even diseases, is termed distress. Classification of neurotic disorders I.