Malignant Melanoma Management and Long-Term Follow-Up in Five Feet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sole Training® with Stacey Lei Krauss
Sole Training® with Stacey Lei Krauss Sole Training is a foot fitness program based on two sequences. The self –massage sequence is restorative and therapeutic; compare it to a yoga class (for your feet). The standing sequence promotes strength, endurance, flexibility and coordination; compare it to a boot-camp workout (for your feet). These exercises work; we’ve been doing them for over a decade. *The Sole Training® video download is available at willPowerMethod.com What is foot fitness? Building muscular strength, endurance, flexibility and neuro-muscular awareness in the feet and ankles. What are the benefits of foot fitness? According to Vibram FiveFingers®, exercising while barefoot, or wearing minimal shoes provide the following benefits: 1. Strengthens Muscles in the Feet and Lower Legs Wearing minimal shoes, or training barefoot will stimulate and strengthen muscles in the feet and lower legs, improving general foot health and reducing the risk of injury. 2. Improves Range of Motion in Ankles, Feet and Toes No longer 'cast' in a traditional, structured shoe, the foot and toes move more naturally. 3. Stimulates Neural Function Important to Balance and Agility When barefoot or wearing minimal shoes, thousands of neurological receptors in the feet send valuable information to the brain, improving balance and agility. 4. Eliminate Heel Lift to Align the Spine and Improve Posture By lowering the heel, your bodyweight becomes evenly distributed across the footbed, promoting proper posture and spinal alignment. 5. Allow the Foot and Body to Move Naturally Which just FEELS GOOD. [email protected] Sole Training® 1 Sole Training® with Stacey Lei Krauss Sole Training® Massage Sequence preparation: mats, blankets, blocks, towels, foot lotion time: 3-10 minutes when: prior to any workout, after any workout, before bed or upon waking EXERCISE EXECUTION FUNCTION Use your fingers to lengthen your toes: LOCALLY: Circulation, Toe flexibility and mobility leading TOE • Long stretch (3 joints except Big Toe) to enhanced balance. -

Rethinking the Evolution of the Human Foot: Insights from Experimental Research Nicholas B
© 2018. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2018) 221, jeb174425. doi:10.1242/jeb.174425 REVIEW Rethinking the evolution of the human foot: insights from experimental research Nicholas B. Holowka* and Daniel E. Lieberman* ABSTRACT presumably owing to their lack of arches and mobile midfoot joints Adaptive explanations for modern human foot anatomy have long for enhanced prehensility in arboreal locomotion (see Glossary; fascinated evolutionary biologists because of the dramatic differences Fig. 1B) (DeSilva, 2010; Elftman and Manter, 1935a). Other studies between our feet and those of our closest living relatives, the great have documented how great apes use their long toes, opposable apes. Morphological features, including hallucal opposability, toe halluces and mobile ankles for grasping arboreal supports (DeSilva, length and the longitudinal arch, have traditionally been used to 2009; Holowka et al., 2017a; Morton, 1924). These observations dichotomize human and great ape feet as being adapted for bipedal underlie what has become a consensus model of human foot walking and arboreal locomotion, respectively. However, recent evolution: that selection for bipedal walking came at the expense of biomechanical models of human foot function and experimental arboreal locomotor capabilities, resulting in a dichotomy between investigations of great ape locomotion have undermined this simple human and great ape foot anatomy and function. According to this dichotomy. Here, we review this research, focusing on the way of thinking, anatomical features of the foot characteristic of biomechanics of foot strike, push-off and elastic energy storage in great apes are assumed to represent adaptations for arboreal the foot, and show that humans and great apes share some behavior, and those unique to humans are assumed to be related underappreciated, surprising similarities in foot function, such as to bipedal walking. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Sole Solution™ Foot Treatment
NU SKIN® PRODUCT INFORMATION PAGE Sole Solution™ Foot Treatment RESTORES HEALTHY LOOKING HEELS, TOES, AND SOLES Positioning Statement people in the rainforests of Central America to relieve persistent Epoch® Sole Solution™ Foot Treatment is a therapeutic foot dry, cracked, red skin on heels, toes, and sides of feet. cream for those suffering from rough, dry, or cracked feet. • Urea—exfoliates calluses and dead cell buildup while provid- ing deep moisturization. Tagline • Papain—a proteolytic enzyme from papaya breaks down and Restores Healthy Looking Heels, Toes, and Soles loosens thick, rough patches of dry, dead skin. Concept Usage/Application 1 If you have chronically dry, cracked feet and have tried all kinds Apply liberally to affected areas on cleansed feet morning and of moisturizers, you know instead of getting better, the problem night, or as needed. Focus on rough or dry areas. Do not rinse persists or even gets worse. A persistent problem like this requires off. Allow product to remain on skin as long as possible. Best more than moisturizing. You need a product that works on the results are seen after six to eight weeks of usage as directed. underlying cause. Epoch® Sole Solution™ Foot Treatment brings the hidden solution of the rainforest to you. Epoch® Sole Solution™ Clinical Study Foot Treatment features crushed allspice berry (Pimenta dioica)— Procedure: traditionally used by the indigenous people of Central America to More than 100 study participants with dry, cracked, or problem relieve persistent dry, cracked, red skin on heels, toes, and sides feet applied Epoch® Sole Solution™ twice daily for 12 weeks. -

Popliteal Fossa, Back of Leg & Sole of Foot
Popliteal fossa, back of leg & Sole of foot Musculoskeletal block- Anatomy-lecture 16 Editing file Color guide : Only in boys slides in Blue Objectives Only in girls slides in Purple important in Red Doctor note in Green By the end of the lecture, students should be able to: Extra information in Grey ✓ The location , boundaries & contents of the popliteal fossa. ✓ The contents of posterior fascial compartment of the leg. ✓ The structures hold by retinacula at the ankle joint. ✓ Layers forming in the sole of foot & bone forming the arches of the foot. Popliteal Fossa Is a diamond-shaped intermuscular space at the back of the knee Boundaries Contents Tibial nerve Common peroneal nerve Semitendinosus Laterally Medially Roof Floor From medial to lateral (above) (above) 1.Skin 1.popliteal surface 1. Popliteal vessels (artery/vein) biceps femoris. semimembranosus 2.superficial of femur 2. Small saphenous vein & semitendinosus fascia & deep 2.posterior ligament 3. Tibial nerve fascia of the of knee joint 4. Common peroneal nerve. (Below) (Below) thigh. 3.popliteus muscle. 5. Posterior cut. nerve of thigh Lateral head of Medial head of 6. Connective tissue & popliteal lymph gastrocnemius gastrocnemius nodes. & plantaris The deepest structure is popliteal artery.* (VERY IMPORTANT) CONTENTS OF THE POSTERIOR FASCIAL COMPARTMENT OF THE LEG The transverse intermuscular septum of the leg is a septum divides the muscles of the posterior Transverse section compartment into superficial and deep groups. Contents 1. Superficial group of muscles 2. Deep group of muscles 3. Posterior tibial artery transverse intermuscular 4. Tibial nerve septum Superficial group Deep group 1. Gastrocnemius 1. -

Left Flank Pain As the Sole Manifestation of Acute Pancreatitis
452 CASE REPORTS Emerg Med J: first published as 10.1136/emj.2003.013847 on 23 May 2005. Downloaded from Left flank pain as the sole manifestation of acute pancreatitis: a report of a case with an initial misdiagnosis J-H Chen, C-H Chern, J-D Chen, C-K How, L-M Wang, C-H Lee ............................................................................................................................... Emerg Med J 2005;22:452–453 On further review of the patient’s case 2 hours after the Acute pancreatitis is not an uncommon disease in an ultrasound examination, a decision was made to obtain a emergency department (ED). It manifests as upper abdominal computed tomography (CT) scan due to concern over the pain, sometimes with radiation of pain to the back and flank limitation of ultrasound studies in some clinical conditions. region. Isolated left flank pain being the sole manifestation of The CT showed abnormal fluid collection over the peri-renal acute pancreatitis is very rare and not previously identified in space and pancreatic tail as well as necrotic changes and the literature. In this report, we present a case of acute swelling of the pancreatic tail (fig 1). Serum pancreatic pancreatitis presenting solely with left flank pain. Having enzymes revealed a normal amylase (90 u/L) and a slightly negative findings on an ultrasound initially, she was elevated lipase level (336 u/L). The patient was diagnosed to misdiagnosed as having possible ‘‘acute pyelonephritis or have acute pancreatitis and admitted for supportive treat- other renal diseases’’. A second radiographic evaluation ment and monitoring. During her admission she was also with computed tomography showed pancreatitis in the tail noted to have hyperlipidemia (triglyceride 980 mg/dL and with abnormal fluid collected extending to the left peri-renal cholesterol 319 mg/dL). -

Manicure and Pedicure Services 77 Respiratory Venous Arterial
Manicure and 3 Pedicure Services INTRODUCTION The two most common services that are provided by beauty parlours are ‘manicure’ and ‘pedicure’. A Beauty Therapist is expected to be proficient in providing these services. ‘Manicure’ is a treatment that improves the appearance of nails and hands, and softens them, whereas, ‘pedicure’ has the same impact on feet. Since manicure and pedicure relax the muscles and skin of the hand and feet, respectively, it is important to understand some basics about the anatomy of the hand and feet. The Beauty Therapist, in particular, must know about the following: • anatomical structure, functions and characteristics of nails, and the process of nail growth. The structure of the nail includes: ▫ Nail root matrix ▫ Nail mantle ▫ Nail plate ▫ Nail wall ▫ Nail grooves ▫ Nail bed ▫ Lunula ▫ Free edge ▫ Hyponychium ▫ Cuticle • anatomical structure of the skin and its functions. NOTES The structure of the skin includes: ▫ layers of the epidermis — dermis and subcutaneous layer ▫ hair follicle, hair shaft, sebaceous gland, arrector pili muscle, sweat gland and sensory nerve endings • names and position of bones in the lower leg and feet • names and position of bones in the wrist, hands, fingers and forearm • structure and functions of lymphatic vessels in the lower leg, feet, hands and arms • position of arteries and veins in the lower leg, feet, hands and arms • location of muscles in the lower leg, feet, hands and arms • nail diseases and disorders • nail and skin analysis by visual or manual examination to identify treatable conditions and contra-indications, restricting or preventing a service SESSION 1: ANATOMY OF THE NAIL, HAND AND FEET Anatomy is the study of the structure of the body of humans and animals, what it is made of, i.e., bones, muscles and skin. -
Hoof Mapping Protocol 3
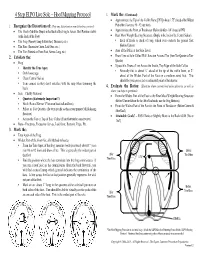
4 Step ELPO Live Sole – Hoof Mapping Protocol 3. Mark the: (Continued) • Approximate the Tip of the Coffin Bone [PIII] (About 1.75” ahead of the Widest 1. Recognize the Distortions of: (Note any distortions or non-distortions you see!) Part of the Foot on a #0 - #2 size foot) • The Heels (Mark the Dimple in the Back of the Frog to Assess Heel Position relative • Approximate the Point of Breakover (Before & After - 1/4” ahead of PIII) to the Back of the Foot) • Rear Most Weight Bearing Structure (Dimple in the back of the Central Sulcus) • The Frog (Narrow, Long & Stretched, Diseased, etc.) ∗ Back of Heels or Back of Frog, which ever contacts the ground first • The Bars (Excessive Curve, Laid Over, etc.) (Before/Current) • The Toe (Pointed on Front Foot, Seems Long, etc.) • Area of the Pillar at the Sole Level 2. Exfoliate the: • Draw Line at Sole Callus/Wall Junction Around Toe (from Toe-Quarter to Toe- Quarter) • Frog • If possible, Draw a Line Across the Inside, Top Edge of the Sole Callus ∗ Identify the True Apex. ∗ Normally this is about ¼” ahead of the tip of the coffin bone, or 2” ∗ Only loose tags. ahead of the Widest Part of the Foot on a medium sized foot. This ∗ Clean Central Sulcus should be your projected or estimated point of breakover. ∗ Trim corners so they don’t interfere with the rasp when trimming the heels. 4. Evaluate the Ratios: (Illustrate where current heel & breakover is, as well as where you hope to get them!) • Sole – Chalky Material • From the Widest Part of the Foot to the Rear Most Weight Bearing Structure -

Study on Impact of Hardness of Sole on Force on Feet During Active Falling
Advances in Social Science, Education and Humanities Research (ASSEHR), volume 199 2018 International Conference on Sports, Arts, Education and Management Engineering (SAEME 2018) Study on Impact of Hardness of Sole on Force on Feet during Active Falling Sicheng Ke1, Hong Xie1, *, Guangwu Sun1, Jiecong Li1 1College of Fashion, Shanghai University of Engineering Science, Shanghai, China. *[email protected] (Hong Xie). Keywords: Active Falling, sole, force on feet, shock absorption. Abstract. The purpose is to study effect of sole on force on feet as an additional factor when human body actively falls at different heights. Methods: 12 male subjects respectively wore three pairs of shoes with different cushioning performances and fell actively at the heights 20cm, 40cm and 60cm. Ground reaction force, pressure distribution on feet, and angle of ankle motion during impact from falling were acquired and analyzed synchronously. Results: Compared with ordinary soles, softer soles can effectively reduce the peak impact force during the impact process, prolong the time interval between the first peak and the second peak of the impact force, and at the same time reduce the maximum and maximum intensity of pressure on the plant, increase the area where plant is in contact with sole, and reduce range of motion of ankle. Conclusions: In comparison with sports shoes with ordinary sole, wearing sports shoes with softer sole can effectively reduce intensity of plantar peak pressure, intensity of mean pressure, peak pressure, and play a good role in shock absorption. Therefore, the softer sole of sports shoes can effectively relieve the burden on the feet, enhance the comfort of the feet, and reduce the chance of sports injuries. -

Strengthen Your Sole Strong Foot
Strengthen your Sole Being on your feet should be easy; it’s what you were made to do. If you experience pain or discomfort anywhere in your body (feet, knees, hips, low back, neck or shoulders) with prolonged periods of standing, walking or being active – it is time for STRONG FEET. Let’s get started… Stand with equal weight on the ball and heel of your foot – Close your eyes and raise your toes up off the floor, just the toes, and then let them fall. Make sure you have equal weight on the ball of and heel of your foot. Pay great attention to what happens to your arch height as you raise and lower your toes. Lower each toe one at a time, like you are playing the piano with your toes. Play it for 1-2 minutes multiple times/day. Strong Foot “Have you lost your sole?” The strong foot exercise (commonly referred to as ‘short foot’ exercise, developed by postural expert Vladimir Janda, MD) is designed to build strength and endurance in the muscles that support the arch/sole of the foot. 1. Take a seat, with both feet on the floor. 2. Slide your big toes toward your heel, without curling your toes or lifting your heel. You will feel your arch raise slightly. 3. Hold this ‘strong foot’ position for 5-10 seconds then relax and repeat as recommended by your ‘movement maven’ health care professional. (Often 10-20 times 5-1 0 times/day 4. Shake it up. Challenge yourself. Below is a progression example; it suggests that you master one stage before you move onto the next. -

Towards the Characterization and Literacy of Female Pelvic Organ Support
Title Page Shifting and Shaping Perceptions: Towards the Characterization and Literacy of Female Pelvic Organ Support by Deanna Christine Easley Sinex B.S. Mechanical Engineering, University of Maryland Baltimore County 2012 Submitted to the Graduate Faculty of the Swanson School of Engineering in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Pittsburgh 2021 Committee Page UNIVERSITY OF PITTSBURGH SWANSON SCHOOL OF ENGINEERING This dissertation was presented by Deanna Christine Easley Sinex It was defended on February 25, 2021 and approved by Harvey S. Borovetz, PhD Distinguished Professor, Bioengineering Renee Clark, PhD Assistant Professor, Industrial Engineering Christiane Hakim, MD, Professor, Radiology Prahlad Menon, PhD, Assistant Professor, Bioengineering Pamela Moalli, MD, PhD Professor, Obstetrics, Gynecology & Reproductive Sciences Yongjie Jessica Zhang, PhD, Professor, Mechanical Engineering Dissertation Director: Steven Abramowitch, PhD, Associate Professor, Bioengineering ii Copyright © by Deanna Christine Easley Sinex 2021 iii Abstract Shifting and Shaping Perceptions: Towards the Characterization and Literacy of Female Pelvic Organ Support Deanna Christine Easley Sinex, PhD University of Pittsburgh, 2019 Pelvic Organ Prolapse (POP) is a pelvic floor condition characterized by the unnatural descent of pelvic organs into the vagina. It occurs as the result of compromised connective tissues and musculature following vaginal delivery and/or changes in tissue composition due to aging. Approximately 50% of women in the United States experience some degree of POP during their lifetime, with symptoms that include altered urination and defecation, physical discomfort, depression, and anxiety. Over the last decade, POP treatments have gained public notoriety due to surgical complications and recurrence of prolapse after surgical repair. -

Transmission of Human Papillomavirus in Heterosexual Couples Brenda Y
RESEARCH Transmission of Human Papillomavirus in Heterosexual Couples Brenda Y. Hernandez,* Lynne R. Wilkens,* Xuemei Zhu,* Pamela Thompson,* Katharine McDuffi e,* Yurii B. Shvetsov,* Lori E. Kamemoto,† Jeffrey Killeen,‡ Lily Ning,* and Marc T. Goodman* CME ACTIVITY Medscape, LLC is pleased to provide online continuing medical education (CME) for this journal article, allowing clinicians the opportunity to earn CME credit. Medscape, LLC is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide CME for physicians. Medscape, LLC designates this educational activity for a maximum of 1.0 AMA PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity. All other clinicians completing this activity will be issued a certifi - cate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test and/or complete the evaluation at http://www.medscape.com/cme/eid; (4) view/print certifi cate. Learning Objectives Upon completion of this activity, participants will be able to: • Identify the most common baseline human papillomavirus (HPV) status of couples • Specify the most common mode of transmission of HPV between couples • Describe the role of anatomic sites in the transmission of HPV • Identify behavioral factors associated with the transmission of HPV Editor D. Peter Drotman, MD, Editor-in-Chief, Emerging Infectious Diseases. Disclosure: D. Peter Drotman, MD, has disclosed no relevant fi nancial relationships. CME Author Charles P. Vega, MD, Associate Professor; Residency Director, Department of Family Medicine, University of California, Irvine, California, USA.