The Non-Intubated Anesthesia for Airway Surgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Surgical Management of Empysema
Surgical Management of Empysema John A Odell MB ChB, FRCS(Ed), FACS Emeritus Professor of Surgery Mayo Clinic College of Medicine Previously Surgical Director Lung Transplantation ©2013 MFMER | slide-1 Problem case. How would you manage? • 64yr male • Previous RLL bullectomy. • Recent left pneumothorax managed elsewhere with chest tube placement. • Because of continued air-leak talc pleurodesis. • Air-leak continues. ©2013 MFMER | slide-2 • On nasal oxygen. Dyspneic on walking • Significant air-leak. More dyspneic when suction applied to chest drain. • FEV1 40% predicted. DLCO 12% predicted. Options? • Thoracotomy and close air leak surgically • Videothoracoscopy and closure of air-leak • Thoracotomy and decortication • Remove chest drain • List for transplantation Historical Treatment of Emphysema • Abdominal compression belts. The stimulus was the observation that emphysematous patients lean forward when breathing. • Pneumoperitoneum. In an attempt to restore diaphragmatic curvature. • Lungs too large for the chest – costochondrectomy or transverse sternotomy to provide more room. Multiple wedge excisions. • Chest grown too large – thoracoplasty • Pleurodesis. Emphysema results from alveolar wall ischemia. • Phrenectomy. Overvigerous inspiration was ripping alveolar walls. • Hilar denervation. To decrease bronchoconstriction and mucous production mediated by the parasympathetic nervous system. • Whole lung irradiation. To increase elastic recoil by inducing fibrosis. ©2013 MFMER | slide-7 Variants of Emphysema that may be Surgically -

Effect of an Indwelling Pleural Catheter Vs Talc Pleurodesis On
This supplement contains the following items: 1. Original protocol, final protocol, summary of changes. 2. Original statistical analysis plan. There were no further changes to the original statistical analysis plan. Downloaded From: https://jamanetwork.com/ on 10/02/2021 The Australasian Malignant Pleural Effusion Trial (AMPLE) A Multicentre Randomized Study Comparing Indwelling Pleural Catheter vs Talc Pleurodesis in Patients with Malignant Pleural Effusions Ethics Registration number 2012-005 Protocol version number 1.0 Protocol date 10/01/2012 Authorised by: Name: Prof YC Gary Lee Role: Chief Investigator Signature: Date: 10/01/2012 Downloaded From: https://jamanetwork.com/ on 10/02/2021 General Information This document describes the Western Australian Randomised Malignant Effusion trial for the purpose of submission for review by the relevant human research and ethics committees. It provides information about procedures for entering patients into the trial and this protocol should not be used as a guide for the treatment of other patients; every care was taken in its drafting, but corrections or amendments may be necessary. Questions or problems relating to this study should be referred to the Chief Investigator or Trial Coordinator. Compliance The trial will be conducted in compliance with this protocol, the National Statement on Ethical Conduct in Human Research, data protection laws and other guidelines as appropriate. It will be registered with the Australia and New Zealand Clinical Trials Registry, once ethical approval is secured. -

2019 Coding and Payment Information Pleural Effusions and Ascites Management
2019 coding and payment information Pleural effusions and ascites management The information contained in this document, including Reimbursement rates shown are Medicare national the codes supplied, is provided for informational payments for 2019 and do not reflect actual payments purposes only. BD makes no statement, promise or made to individual providers, as payments are adjusted guarantee concerning the appropriateness of any codes specific to particular geographic regions. for a particular procedure, actual levels of All information is subject to change without notice. In reimbursement, payment or charge or that addition, payers or local carriers may have their own reimbursement will be made. coding and billing requirements. Consult your payer This is not intended to be a comprehensive guide to all organization with regard to local reimbursement policies. coding and payment information. 2019 Medicare outpatient facility rates CPT® 2019 APC OPPS 2019 ASC Description APC Status code base rate* base rate Pleural catheter procedures 32550 Insertion of indwelling tunneled pleural catheter 5341 J1 $2,947 $1,790 32552 Removal of indwelling tunneled pleural catheter with cuff 5181 Q2 $620 $319 32560 Instillation via chest tube/catheter, agent for pleurodesis 5181 T $620 N/A 32650 Thoracoscopy, surgical, with pleurodesis (e.g., mechanical or chemical) N/A; inpatient procedure Peritoneal catheter procedures Insertion of tunneled intraperitoneal catheter (e.g., dialysis, intraperitoneal chemotherapy instillation, management of ascites), 49418 -
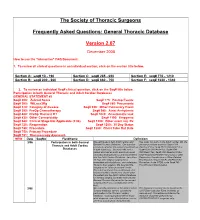
FAQ Document
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -

Nonintubated Thoracoscopic Surgery Using Regional Anesthesia and Vagal Block and Targeted Sedation
Original Article Nonintubated thoracoscopic surgery using regional anesthesia and vagal block and targeted sedation Ke-Cheng Chen1,2, Ya-Jung Cheng3, Ming-Hui Hung3, Yu-Ding Tseng1, Jin-Shing Chen1,2 1Department of Surgery, National Taiwan University Hospital Yun-Lin Branch, Yun-Lin County, Taiwan; 2Division of Thoracic Surgery, Department of Surgery, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan; 3Department of Anesthesiology, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan Corresponding to: Dr. Jin-Shing Chen. Department of Surgery, National Taiwan University Hospital, No. 7, Chung Shan South Road, Taipei, Taiwan. Email: [email protected]. Objective: Thoracoscopic surgery without endotracheal intubation is a novel technique for diagnosis and treatment of thoracic diseases. This study reported the experience of nonintubated thoracoscopic surgery in a tertiary medical center in Taiwan. Methods: From August 2009 through August 2013, 446 consecutive patients with lung or pleural diseases were treated by nonintubated thoracoscopic surgery. Regional anesthesia was achieved by thoracic epidural anesthesia or internal intercostal blockade. Targeted sedation was performed with propofol infusion to achieve a bispectral index value between 40 and 60. The demographic data and clinical outcomes were evaluated by retrospective chart review. Results: Thoracic epidural anesthesia was used in 290 patients (65.0%) while internal intercostal blockade was used in 156 patients (35.0%). The final diagnosis were primary lung cancer in 263 patients (59.0%), metastatic lung cancer in 38 (8.5%), benign lung tumor in 140 (31.4%), and pneumothorax in 5 (1.1%). The median anesthetic induction time was 30 minutes by thoracic epidural anesthesia and was 10 minutes by internal intercostal blockade. -

Your Lung Operation Booklet
1 AMERICAN COLLEGE OF SURGEONS DIVISION OF EDUCATION SURGICAL PATIENT EDUCATION Table of Contents Welcome ...................................................................................1 Your Lungs ...............................................................................2 Lung Cancer ...........................................................................3 SURGICAL Understanding Your Operation ........................................4 PATIENT Preoperative Tests ................................................................5 EDUCATION Home Preparation ................................................................8 The Day of Your Operation ...............................................13 After Your Operation ..........................................................14 Your Recovery and Discharge .........................................17 When to Call Your Doctor .................................................19 Welcome You and your family are important members of the surgical team. The American College of Surgeons (ACS) “Your Lung Operation: Education for a Better Recovery” program will help you prepare for your operation and recovery. You and your family will know what to expect. You will learn how to work with your surgical team to ensure that you have the best surgical outcomes. COMPLETE THE “YOUR LUNG OPERATION” EDUCATION PROGRAM: Watch the DVD Read the booklet Review the Medication List and Quit Smoking Resources (inside front cover) Complete the Activity Log (inside front cover) Send us your evaluation after -

Agenda Item 5
List A (O) Respiratory system treatments and procedures. (1) Biopsy and/or excision (removal) of lesion of larynx, vocal cords, trachea (A) Loss or change of voice. (B) Swallowing or breathing difficulties. (C) Perforation (hole) or fistula (connection) in esophagus (tube from throat to stomach). (2) Rhinoplasty (surgery to change the shape of the nose) or nasal reconstruction with or without septoplasty A) Deformity of skin, bone or cartilage. (B) Creation of new problems, such as perforation of the nasal septum (hole in wall between the right and left halves of the nose) or breathing difficulty. (3) Submucous resection of nasal septum or nasal septoplasty (surgery to remove blockage in or straighten the nose) (A) Persistence, recurrence or worsening of the obstruction. (B) Perforation of nasal septum (hole in wall between the right and left halves of the nose) with dryness and crusting. (C) External deformity of the nose. (4) Sinus surgery/endoscopic sinus surgery (A) Spinal fluid leak (B) Visual loss or other eye injury (C) Numbness in front teeth and palate (D) Loss or reduction in sense of taste or smell (E) Recurrence of disease (F) Empty Nose Syndrome (sensation of nasal congestion, sensation of not being able to take in adequate air through nose) (G) Injury to tear duct causing drainage of tears down the cheek (H) Brain injury and/or infection (I) Injury to nasal septum (J) Nasal obstruction (5) Lung biopsy (A) Air leak with pneumothorax (leak of air from lung to inside of chest causing the lung to collapse) with need for insertion of chest drainage tube into space between lung and chest wall or repeat surgery. -

Hyperbaric Medicine Center During the Actual Questions About the Treatment Process Are Treatment Process, for All Patients’ Confidentiality, No Always Welcomed
Patient Label / Name HBO - HYPERBARIC OXYGEN PATIENT EDUCATION - Page | 1 FAQs HBO is a medical treatment which enhances the body’s natural healing process by inhalation of 100% oxygen in a total body chamber, where atmospheric pressure is WHAT IS HBO? increased and controlled. It is used for a wide variety of treatments usually as an adjunctive part of an overall HBO or HBOT stands for: Hyperbaric Oxygen Therapy medical care plan that can be done on an inpatient or WHAT DOES IT DO? outpatient basis. HBO or HBOT, simply, HBOT is a means of providing WAIT! CAN YOU TELL ME MORE ABOUT THE additional oxygen to your body tissues. “ENTIRELY CLOSED PRESSURE CHAMBER”? HOW DOES IT WORK? Your entire body will go in a closely monitored, TRANSPARENT, 100% ACRYLIC topped, sealed chamber. By exposing the Most patients have plenty of room to get comfortable entire body to and can enjoy their 1.5-2 hour treatments while watching oxygen under TV (installed on each chamber with internal speakers) or increased napping. atmospheric A highly qualified Hyperbaric Tech will be in the room pressure. with you at all times during your treatment, and you will be closely monitored before, during and after all HBO The patient is entirely enclosed in a pressure chamber Treatments. breathing 100% oxygen (O2) at greater than one atmosphere HBO Chambers have microphones that allow your HBO (atm) pressure. Tech to hear you without need to push any buttons. SO, HOW DOES THAT HELP? Simply call out and you will be heard. If you should need to cut your treatment short or want to get out at any HBO therapy serves 4 PRIMARY FUNCTIONS: time, your HBO Tech is always right there to safely decompress the chamber and help you out and call for 1. -

Answer Key Chapter 1
Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 1 of 101 Answer Key Chapter 1 Introduction to Clinical Coding 1.1: Self-Assessment Exercise 1. The patient is seen as an outpatient for a bilateral mammogram. CPT Code: 77055-50 Note that the description for code 77055 is for a unilateral (one side) mammogram. 77056 is the correct code for a bilateral mammogram. Use of modifier -50 for bilateral is not appropriate when CPT code descriptions differentiate between unilateral and bilateral. 2. Physician performs a closed manipulation of a medial malleolus fracture—left ankle. CPT Code: 27766-LT The code represents an open treatment of the fracture, but the physician performed a closed manipulation. Correct code: 27762-LT 3. Surgeon performs a cystourethroscopy with dilation of a urethral stricture. CPT Code: 52341 The documentation states that it was a urethral stricture, but the CPT code identifies treatment of ureteral stricture. Correct code: 52281 4. The operative report states that the physician performed Strabismus surgery, requiring resection of the medial rectus muscle. CPT Code: 67314 The CPT code selection is for resection of one vertical muscle, but the medial rectus muscle is horizontal. Correct code: 67311 5. The chiropractor documents that he performed osteopathic manipulation on the neck and back (lumbar/thoracic). CPT Code: 98925 Note in the paragraph before code 98925, the body regions are identified. The neck would be the cervical region; the thoracic and lumbar regions are identified separately. Therefore, three body regions are identified. Correct code: 98926 Instructor's Guide AC210610: Basic CPT/HCPCS Exercises Page 2 of 101 6. -

Lymphangioleiomyomatosis (LAM)
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Lymphangioleiomyomatosis (LAM) What is LAM? Lymphangioleiomyomatosis (lim-FAN-jee-oh-ly-oh-my-oh-ma- Pneumothroax TOE-sis), also known as LAM, is a rare lung disease that mainly Lung Cysts affects women, usually during their childbearing years. LAM occurs in 3-8 women per million in the general population. LAM is caused by mutations in the tuberous sclerosis complex (TSC) genes. These mutations lead to growth of abnormal cells that spread by the blood stream and make their way into the lungs. Once in the lungs, these cells create holes in the lung tissue (called cysts) that can weaken breathing and the ability to take up oxygen. What are the symptoms of LAM? blood protein called vascular endothelial growth factor-D Symptoms of LAM are similar to other lung diseases. Some (VEGF-D). Elevated VEGF-D levels can help confirm the times patients can be misdiagnosed with asthma, bronchitis, diagnosis of LAM without needing a lung biopsy. Blood or emphysema. These symptoms include: levels of VEGF-D should be checked before doing invasive procedures, such as lung biopsy. ■■ Shortness of breath Lung Biopsy ■■ Fatigue In most (>70%) patients, the diagnosis of LAM can be ■■ Lung collapse, also known as a pneumothorax confirmed based on clinical and/or laboratory findings and ■■ Chest pain does not require a biopsy. However, a lung biopsy may be CLIP AND COPY AND CLIP ■■ Cough needed to confirm the diagnosis of LAM in some cases. ■■ Coughing up small amounts blood There are two ways to do a lung biopsy to diagnose LAM: How is LAM diagnosed and monitored? 1. -

Tracheotomy in COVID-19 Patients: Optimizing Patient Selection and Identifying Prognostic Indicators
Tracheotomy in COVID-19 patients: Optimizing Patient selection and identifying prognostic indicators Stubington T.J.1, Mallick A.S., Garas G.3, Stubington E.4 ,Reddy C.5 , Mansuri M.S.6 1. MBBS BMedSci MRCS(ENT) PGCert (MedEd), Department of Otorhinolaryngology - Head and Neck Surgery, Royal Derby Hospital, Uttoxeter Road, Derby, DE22 3NE, United Kingdom 2. MBBS MRCS (DOHNS) PhD, Department of Otorhinolaryngology - Head and Neck Surgery, Royal Derby Hospital, Uttoxeter Road, Derby, DE22 3NE, United Kingdom 3. PhD FRCS FEBORL-HNS, Department of Otorhinolaryngology - Head and Neck Surgery, Nottingham University Hospitals NHS Trust, Queens Medical Center Campus, Nottingham, NG7 2UH, United Kingdom 4. BSc, Mres, PhD STOR-I Centre for Doctoral Training, Lancaster university, UK 5. MBBS FANZCA, Department of Anaesthesia, Royal Derby Hospital, Uttoxeter Road, Derby, DE22 3NE 6. MBChB, Msc, Dip (RMES), FRCS (ORL), Department of Otorhinolaryngology - Head and Neck Surgery, Royal Derby Hospital, Uttoxeter Road, Derby, DE22 3NE, United Kingdom Corresponding Author: Thomas James Stubington, Dept. Head and Neck Surgery, Royal Derby Hospital, Uttoxeter Road, Derby, DE223NE [email protected] Keywords SARS-CoV-2, Coronavirus, COVID-19, Pandemic, Tracheotomy Word Count: 1787 Abstract Background Tracheotomy, through its ability to wean patients off ventilation, can shorten ICU length of stay and in doing so increase ICU bed capacity, crucial for saving lives during the COVID-19 pandemic. To date, there is a paucity of patient selection criteria and prognosticators to facilitate decision-making and enhance precious ICU capacity. Methods Prospective study of COVID-19 patients undergoing tracheotomy (n=12) over a 4-week period (March-April 2020). -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of