Invited Review Tryptophan Metabolism: a Versatile
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Remodeling Adipose Tissue Through in Silico Modulation of Fat Storage For
Chénard et al. BMC Systems Biology (2017) 11:60 DOI 10.1186/s12918-017-0438-9 RESEARCHARTICLE Open Access Remodeling adipose tissue through in silico modulation of fat storage for the prevention of type 2 diabetes Thierry Chénard2, Frédéric Guénard3, Marie-Claude Vohl3,4, André Carpentier5, André Tchernof4,6 and Rafael J. Najmanovich1* Abstract Background: Type 2 diabetes is one of the leading non-infectious diseases worldwide and closely relates to excess adipose tissue accumulation as seen in obesity. Specifically, hypertrophic expansion of adipose tissues is related to increased cardiometabolic risk leading to type 2 diabetes. Studying mechanisms underlying adipocyte hypertrophy could lead to the identification of potential targets for the treatment of these conditions. Results: We present iTC1390adip, a highly curated metabolic network of the human adipocyte presenting various improvements over the previously published iAdipocytes1809. iTC1390adip contains 1390 genes, 4519 reactions and 3664 metabolites. We validated the network obtaining 92.6% accuracy by comparing experimental gene essentiality in various cell lines to our predictions of biomass production. Using flux balance analysis under various test conditions, we predict the effect of gene deletion on both lipid droplet and biomass production, resulting in the identification of 27 genes that could reduce adipocyte hypertrophy. We also used expression data from visceral and subcutaneous adipose tissues to compare the effect of single gene deletions between adipocytes from each -

Electronic Supplementary Material (ESI) for Metallomics
Electronic Supplementary Material (ESI) for Metallomics. This journal is © The Royal Society of Chemistry 2018 Uniprot Entry name Gene names Protein names Predicted Pattern Number of Iron role EC number Subcellular Membrane Involvement in disease Gene ontology (biological process) Id iron ions location associated 1 P46952 3HAO_HUMAN HAAO 3-hydroxyanthranilate 3,4- H47-E53-H91 1 Fe cation Catalytic 1.13.11.6 Cytoplasm No NAD biosynthetic process [GO:0009435]; neuron cellular homeostasis dioxygenase (EC 1.13.11.6) (3- [GO:0070050]; quinolinate biosynthetic process [GO:0019805]; response to hydroxyanthranilate oxygenase) cadmium ion [GO:0046686]; response to zinc ion [GO:0010043]; tryptophan (3-HAO) (3-hydroxyanthranilic catabolic process [GO:0006569] acid dioxygenase) (HAD) 2 O00767 ACOD_HUMAN SCD Acyl-CoA desaturase (EC H120-H125-H157-H161; 2 Fe cations Catalytic 1.14.19.1 Endoplasmic Yes long-chain fatty-acyl-CoA biosynthetic process [GO:0035338]; unsaturated fatty 1.14.19.1) (Delta(9)-desaturase) H160-H269-H298-H302 reticulum acid biosynthetic process [GO:0006636] (Delta-9 desaturase) (Fatty acid desaturase) (Stearoyl-CoA desaturase) (hSCD1) 3 Q6ZNF0 ACP7_HUMAN ACP7 PAPL PAPL1 Acid phosphatase type 7 (EC D141-D170-Y173-H335 1 Fe cation Catalytic 3.1.3.2 Extracellular No 3.1.3.2) (Purple acid space phosphatase long form) 4 Q96SZ5 AEDO_HUMAN ADO C10orf22 2-aminoethanethiol dioxygenase H112-H114-H193 1 Fe cation Catalytic 1.13.11.19 Unknown No oxidation-reduction process [GO:0055114]; sulfur amino acid catabolic process (EC 1.13.11.19) (Cysteamine -

Remodeling Adipose Tissue Through in Silico Modulation of Fat Storage For
Chénard et al. BMC Systems Biology (2017) 11:60 DOI 10.1186/s12918-017-0438-9 RESEARCHARTICLE Open Access Remodeling adipose tissue through in silico modulation of fat storage for the prevention of type 2 diabetes Thierry Chénard2, Frédéric Guénard3, Marie-Claude Vohl3,4, André Carpentier5, André Tchernof4,6 and Rafael J. Najmanovich1* Abstract Background: Type 2 diabetes is one of the leading non-infectious diseases worldwide and closely relates to excess adipose tissue accumulation as seen in obesity. Specifically, hypertrophic expansion of adipose tissues is related to increased cardiometabolic risk leading to type 2 diabetes. Studying mechanisms underlying adipocyte hypertrophy could lead to the identification of potential targets for the treatment of these conditions. Results: We present iTC1390adip, a highly curated metabolic network of the human adipocyte presenting various improvements over the previously published iAdipocytes1809. iTC1390adip contains 1390 genes, 4519 reactions and 3664 metabolites. We validated the network obtaining 92.6% accuracy by comparing experimental gene essentiality in various cell lines to our predictions of biomass production. Using flux balance analysis under various test conditions, we predict the effect of gene deletion on both lipid droplet and biomass production, resulting in the identification of 27 genes that could reduce adipocyte hypertrophy. We also used expression data from visceral and subcutaneous adipose tissues to compare the effect of single gene deletions between adipocytes from each -

Computational Analyses of Small Molecules Activity from Phenotypic Screens
Computational analyses of small molecules activity from phenotypic screens Azedine Zoufir Hughes Hall This dissertation is submitted for the degree of Doctor of Philosophy July 2018 Declaration This thesis is submitted as the result of my own work and includes nothing which is the outcome of work done in collaboration except where specifically indicated in the text. It is not substantially the same as any that I have submitted, or, is being concurrently submitted for a degree or diploma or other qualification at the University of Cambridge or any other University or similar institution except as declared in the preface and specified in the text. I further state that no substantial part of my dissertation has already been submitted, or, is being concurrently submitted for any such degree, diploma or other qualification at the University of Cambridge or any other University or similar institution except as declared in the Preface and specified in the text. This dissertation does not exceed the word limit of 60,000 words. Azedine Zoufir July 2018 Summary Title: Computational analyses of small molecules activity from phenotypic screens Author: Azedine Zoufir Drug discovery is no longer relying on the one gene-one disease paradigm nor on target-based screening alone to discover new drugs. Phenotypic-based screening is regaining momentum to discover new compounds since those assays provide an environment closer to the physiological state of the disease and allow to better anticipate off-target effects and other factors that can limit the efficacy of the drugs. However, uncovering the mechanism of action of the compounds active in those assays relies on in vitro techniques that are expensive and time- consuming. -
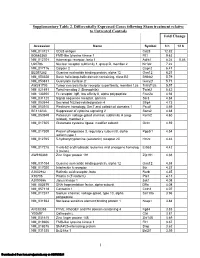
Supplementary Table 2
Supplementary Table 2. Differentially Expressed Genes following Sham treatment relative to Untreated Controls Fold Change Accession Name Symbol 3 h 12 h NM_013121 CD28 antigen Cd28 12.82 BG665360 FMS-like tyrosine kinase 1 Flt1 9.63 NM_012701 Adrenergic receptor, beta 1 Adrb1 8.24 0.46 U20796 Nuclear receptor subfamily 1, group D, member 2 Nr1d2 7.22 NM_017116 Calpain 2 Capn2 6.41 BE097282 Guanine nucleotide binding protein, alpha 12 Gna12 6.21 NM_053328 Basic helix-loop-helix domain containing, class B2 Bhlhb2 5.79 NM_053831 Guanylate cyclase 2f Gucy2f 5.71 AW251703 Tumor necrosis factor receptor superfamily, member 12a Tnfrsf12a 5.57 NM_021691 Twist homolog 2 (Drosophila) Twist2 5.42 NM_133550 Fc receptor, IgE, low affinity II, alpha polypeptide Fcer2a 4.93 NM_031120 Signal sequence receptor, gamma Ssr3 4.84 NM_053544 Secreted frizzled-related protein 4 Sfrp4 4.73 NM_053910 Pleckstrin homology, Sec7 and coiled/coil domains 1 Pscd1 4.69 BE113233 Suppressor of cytokine signaling 2 Socs2 4.68 NM_053949 Potassium voltage-gated channel, subfamily H (eag- Kcnh2 4.60 related), member 2 NM_017305 Glutamate cysteine ligase, modifier subunit Gclm 4.59 NM_017309 Protein phospatase 3, regulatory subunit B, alpha Ppp3r1 4.54 isoform,type 1 NM_012765 5-hydroxytryptamine (serotonin) receptor 2C Htr2c 4.46 NM_017218 V-erb-b2 erythroblastic leukemia viral oncogene homolog Erbb3 4.42 3 (avian) AW918369 Zinc finger protein 191 Zfp191 4.38 NM_031034 Guanine nucleotide binding protein, alpha 12 Gna12 4.38 NM_017020 Interleukin 6 receptor Il6r 4.37 AJ002942 -
Delaying Aging and the Aging-Associated Decline in Protein Homeostasis by Inhibition of Tryptophan Degradation
Delaying aging and the aging-associated decline in protein homeostasis by inhibition of tryptophan degradation Annemieke T. van der Goota, Wentao Zhub, Rafael P. Vázquez-Manriquec,1, Renée I. Seinstraa, Katja Dettmerb, Helen Michelsa, Francesca Farinac, Jasper Krijnend, Ronald Melkie, Rogier C. Buijsmanf, Mariana Ruiz Silvaa, Karen L. Thijssena, Ido P. Kemad, Christian Neric, Peter J. Oefnerb, and Ellen A. A. Nollena,g,2 Departments of aGenetics and dLaboratory Medicine, University of Groningen, University Medical Centre Groningen, 9700 RB, Groningen, The Netherlands; bInstitute of Functional Genomics, University of Regensburg, 93053 Regensburg, Germany; cInstitut National de la Santé et de la Recherche Médicale, Unit 894, Laboratory of Neuronal Cell Biology and Pathology, 75014 Paris, France; eLaboratoire d’Enzymologie et Biochimie Structurales, Centre National de la Recherche Scientifique, 91190 Gif-sur-Yvette, France; fTranslational Research Centre B.V., 5342 AC, Oss, The Netherlands; and gUniversity of Groningen, University Medical Centre Groningen, European Research Institute for the Biology of Aging, 9700 AD, Groningen, The Netherlands Edited by F. Ulrich Hartl, Max Planck Institute of Biochemistry, Martinsried, Germany, and approved July 20, 2012 (received for review February 26, 2012) Toxicity of aggregation-prone proteins is thought to play an im- Results portant role in aging and age-related neurological diseases like Knockdown of tdo-2 Suppresses Toxicity of α-Synuclein in C. elegans. Parkinson and Alzheimer’s diseases. Here, we identify tryptophan α-Synuclein is an aggregation-prone protein that is involved in 2,3-dioxygenase (tdo-2), the first enzyme in the kynurenine path- Parkinson disease and other synucleinopathies (14, 15). We have way of tryptophan degradation, as a metabolic regulator of age- previously identified 80 genes that modify α-synuclein inclusion α related -synuclein toxicity in a Caenorhabditis elegans model. -

Effects of Pro-Inflammatory Cytokines on Expression of Kynurenine
Asp et al. Journal of Inflammation 2011, 8:25 http://www.journal-inflammation.com/content/8/1/25 RESEARCH Open Access Effects of pro-inflammatory cytokines on expression of kynurenine pathway enzymes in human dermal fibroblasts Linnéa Asp1, Anne-Sofie Johansson1, Amandeep Mann1, Björn Owe-Larsson2, Ewa M Urbanska3,4, Tomasz Kocki3, Magdalena Kegel5, Göran Engberg5, Gabriella BS Lundkvist1 and Håkan Karlsson1* Abstract Background: The kynurenine pathway (KP) is the main route of tryptophan degradation in the human body and generates several neuroactive and immunomodulatory metabolites. Altered levels of KP-metabolites have been observed in neuropsychiatric and neurodegenerative disorders as well as in patients with affective disorders. The purpose of the present study was to investigate if skin derived human fibroblasts are useful for studies of expression of enzymes in the KP. Methods: Fibroblast cultures were established from cutaneous biopsies taken from the arm of consenting volunteers. Such cultures were subsequently treated with interferon (IFN)-g 200 U/ml and/or tumor necrosis factor (TNF)-a, 100 U/ml for 48 hours in serum-free medium. Levels of transcripts encoding different enzymes were determined by real-time PCR and levels of kynurenic acid (KYNA) were determined by HPLC. Results: At base-line all cultures harbored detectable levels of transcripts encoding KP enzymes, albeit with considerable variation across individuals. Following cytokine treatment, considerable changes in many of the transcripts investigated were observed. For example, increases in the abundance of transcripts encoding indoleamine 2,3-dioxygenase, kynureninase or 3-hydroxyanthranilic acid oxygenase and decreases in the levels of transcripts encoding tryptophan 2,3-dioxygenase, kynurenine aminotransferases or quinolinic acid phosphoribosyltransferase were observed following IFN-g and TNF-a treatment. -

The Interplay Between Cytokines and the Kynurenine Pathway in T Inflammation and Atherosclerosis ⁎ Roland Baumgartner , Maria J
Cytokine 122 (2019) 154148 Contents lists available at ScienceDirect Cytokine journal homepage: www.elsevier.com/locate/cytokine The interplay between cytokines and the Kynurenine pathway in T inflammation and atherosclerosis ⁎ Roland Baumgartner , Maria J. Forteza, Daniel F.J. Ketelhuth Cardiovascular Medicine Unit, Center for Molecular Medicine, Department of Medicine, Karolinska Institute and Karolinska University Hospital, SE-17176 Stockholm, Sweden ARTICLE INFO ABSTRACT Keywords: The kynurenine pathway (KP) is the major metabolic route of tryptophan (Trp) metabolism. Indoleamine 2,3- Atherosclerosis dioxygenase (IDO1), the enzyme responsible for the first and rate-limiting step in the pathway, as well asother Inflammation enzymes in the pathway, have been shown to be highly regulated by cytokines. Hence, the KP has been im- Cytokine plicated in several pathologic conditions, including infectious diseases, psychiatric disorders, malignancies, and Kynurenine autoimmune and chronic inflammatory diseases. Additionally, recent studies have linked the KP with athero- Tryptophan sclerosis, suggesting that Trp metabolism could play an essential role in the maintenance of immune homeostasis in the vascular wall. This review summarizes experimental and clinical evidence of the interplay between cy- tokines and the KP and the potential role of the KP in cardiovascular diseases. 1. Introduction 2. The atherosclerotic process The kynurenine pathway (KP) is the major metabolic route of de- CVDs, which are largely due to atherosclerosis, are the -

Co-Treatments to Boost IDO Activity and Inhibit Production of Downstream Catabolites Induce Durable Suppression of Experimental Autoimmune Encephalomyelitis
ORIGINAL RESEARCH published: 17 June 2020 doi: 10.3389/fimmu.2020.01256 Co-treatments to Boost IDO Activity and Inhibit Production of Downstream Catabolites Induce Durable Suppression of Experimental Autoimmune Encephalomyelitis 1 2 1 1 3 Edited by: Henrique Lemos , Eslam Mohamed , Rong Ou , Caroline McCardle , Xiaozhong Zheng , 3 4 3 1 Kutty Selva Nandakumar, Kris McGuire , Natalie Z. M. Homer , Damian J. Mole , Lei Huang * and 1 Southern Medical University, China Andrew L. Mellor * Reviewed by: 1 Immune Metabolism Laboratory, Faculty of Medical Sciences, Translational and Clinical Research Institute, Newcastle Ursula Grohmann, University, Newcastle upon Tyne, United Kingdom, 2 H. Lee Moffitt Cancer Center & Research Institute, Tampa, FL, University of Perugia, Italy United States, 3 Centre for Inflammation Research, University of Edinburgh, Edinburgh, United Kingdom, 4 Mass Sergio Rutella, Spectrometry Core, Edinburgh Clinical Research Facility, Centre for Cardiovascular Sciences, Queen’s Medical Research Nottingham Trent University, Institute, Edinburgh, United Kingdom United Kingdom Gilles J. Guillemin, Macquarie University, Australia Reinforcing defective tolerogenic processes slows progression of autoimmune (AI) *Correspondence: diseases and has potential to promote drug-free disease remission. Previously, Lei Huang we reported that DNA nanoparticles (DNPs) and cyclic dinucleotides (CDNs) slow [email protected] Andrew L. Mellor progression of experimental autoimmune encephalomyelitis (EAE), a mouse model of [email protected] -

A Structural and Mechanistic Study of Two Members of Cupin Family Protein
Georgia State University ScholarWorks @ Georgia State University Chemistry Dissertations Department of Chemistry Summer 6-18-2013 A Structural and Mechanistic Study of Two Members of Cupin Family Protein Fange Liu Georgia State university Follow this and additional works at: https://scholarworks.gsu.edu/chemistry_diss Recommended Citation Liu, Fange, "A Structural and Mechanistic Study of Two Members of Cupin Family Protein." Dissertation, Georgia State University, 2013. https://scholarworks.gsu.edu/chemistry_diss/79 This Dissertation is brought to you for free and open access by the Department of Chemistry at ScholarWorks @ Georgia State University. It has been accepted for inclusion in Chemistry Dissertations by an authorized administrator of ScholarWorks @ Georgia State University. For more information, please contact [email protected]. A STRUCTURAL AND MECHANISTIC STUDY OF TWO MEMBERS OF CUPIN FAMILY PROTEIN by FANGE (KATHERINE) LIU Under the Direction of Dr. Aimin Liu ABSTRACT Cupin superfamily is a functionally diverse large group of proteins sharing a jelly roll β-barrel fold. An enzymatic member 3-hydroxyanthranilate-3,4-dioxygenase (HAO) and a non-enzymatic member pirin, which is a human nuclear metalloprotein of unknown function present in all human tissues, were selected for structural and functional studies in this dissertation work. HAO is an important enzyme for tryptophan catabolism and for 2-nitrobenzoic acid biodegradation. In this work, seven catalytic intermediate were captured in HAO single crystals, enabling for the first time a nearly complete structural snapshot viewing of the entire molecular oxygen activation and insertion mechanism in an iron- and O 2-depedent enzyme. The rapid catalytic turnover rate was found achieved in large part by protein dynamics that facilitates O 2 binding to the catalytic iron, which is bound to the enzyme by a facile 2-His-1-carboxylate ligand motif. -

Blockade of the AHR Restricts a Treg-Macrophage Suppressive Axis Induced by L-Kynurenine
ARTICLE https://doi.org/10.1038/s41467-020-17750-z OPEN Blockade of the AHR restricts a Treg-macrophage suppressive axis induced by L-Kynurenine Luis Felipe Campesato1,2, Sadna Budhu 1,2, Jeremy Tchaicha3, Chien-Huan Weng 1,2, Mathieu Gigoux 1,2, Ivan Jose Cohen4, David Redmond1,2, Levi Mangarin1,2, Stephane Pourpe1,2, Cailian Liu1,2, Roberta Zappasodi 1,2, Dmitriy Zamarin1,2, Jill Cavanaugh3, Alfredo C. Castro3, Mark G. Manfredi3, ✉ ✉ Karen McGovern3, Taha Merghoub 1,2,5 & Jedd D. Wolchok 1,2,5 1234567890():,; Tryptophan catabolism by the enzymes indoleamine 2,3-dioxygenase 1 and tryptophan 2,3- dioxygenase 2 (IDO/TDO) promotes immunosuppression across different cancer types. The tryptophan metabolite L-Kynurenine (Kyn) interacts with the ligand-activated transcription factor aryl hydrocarbon receptor (AHR) to drive the generation of Tregs and tolerogenic myeloid cells and PD-1 up-regulation in CD8+ T cells. Here, we show that the AHR pathway is selectively active in IDO/TDO-overexpressing tumors and is associated with resistance to immune checkpoint inhibitors. We demonstrate that IDO-Kyn-AHR-mediated immunosup- pression depends on an interplay between Tregs and tumor-associated macrophages, which can be reversed by AHR inhibition. Selective AHR blockade delays progression in IDO/TDO- overexpressing tumors, and its efficacy is improved in combination with PD-1 blockade. Our findings suggest that blocking the AHR pathway in IDO/TDO expressing tumors would overcome the limitation of single IDO or TDO targeting agents and constitutes a personalized approach to immunotherapy, particularly in combination with immune checkpoint inhibitors. 1 Swim Across America and Ludwig Collaborative Laboratory, Immunology Program, Parker Institute for Cancer Immunotherapy, Memorial Sloan Kettering Cancer Center, New York, NY, USA. -

Electronic Supplementary Material (ESI) for Molecular Omics
Electronic Supplementary Material (ESI) for Molecular Omics. This journal is © The Royal Society of Chemistry 2020 SUPPLEMENTARY INFORMATION Supplementary Table S2. GO analysis for the 289 overlapping genes based on DAVID database. ID Category Term Genes PValue HSD3B2, CYP24A1, ME3, SORD, ADHFE1, CYP2C44, PAH, HIBADH, MTHFD1, ALDH1A1, PECR, CYP4A12A, FMO1, MIOX, CYP2J11, HAAO, BC089597, ALDH4A1, BDH2, DAO, NQO1, BDH1, SARDH, HPD, 1 BP GO:0055114~oxidation reduction 1.18E-17 NOX4, GCDH, SUOX, AKR1E1, QDPR, CMAH, HGD, FADS2, AKR1C21, PPARGC1A, TET1, DDO, NNT, HAO2, CYP2D26, HSD11B2, DIO1, RDH16, CYP4A14, STEAP1, DCXR, PRODH SLC12A6, SLC2A13, SLC5A2, SLC12A1, SLC5A1, SLC22A7, SLC22A8, RHBG, SLC7A9, AQP6, SLC26A4, GO:0055085~transmembrane 2 BP SLC23A1, SLC16A7, SLC2A4, RHCG, SLC7A1, 1.28E-07 transport SLC25A10, SLC2A2, SLC16A9, SLC5A9, SLC13A2, SLC25A37, SLC13A3, SLC46A1, SLC5A12 PDK2, SLC37A4, PDK4, CMAH, PGAM2, ADIPOQ, GO:0005996~monosaccharide 3 BP HIBADH, PCK1, GALM, G6PC, PPP1R1A, GYS2, MYC, 1.25E-06 metabolic process DCXR, XYLB SLC12A6, SLC5A2, SLC23A1, SLC12A1, SLC5A1, 4 BP GO:0006814~sodium ion transport SLC9A3, SLC5A9, SLC13A2, SLC13A3, SLC10A2, 3.05E-06 SLC4A4, SLC5A12 SLC5A2, G6PC, SLC2A4, SLC2A2, SLC5A1, SLC37A4, 5 BP GO:0015758~glucose transport 3.22E-06 STXBP4 SLC5A2, G6PC, SLC2A4, SLC2A2, SLC5A1, SLC37A4, 6 BP GO:0008645~hexose transport 4.95E-06 STXBP4 GO:0015749~monosaccharide SLC5A2, G6PC, SLC2A4, SLC2A2, SLC5A1, SLC37A4, 7 BP 6.06E-06 transport STXBP4 GO:0006006~glucose metabolic PDK2, G6PC, PPP1R1A, PDK4, SLC37A4, GYS2,