Coronaviruses in Australian Bats
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
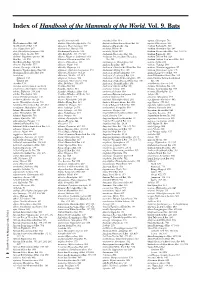
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A. -

O HÁBITO ALIMENTAR DOS MORCEGOS (Mammalia, Chiroptera) E SUA RELAÇÃO COM a DIVERSIDADE VIRAL
UNIVERSIDADE DE BRASÍLIA INSTITUTO DE CIÊNCIAS BIOLÓGICAS PROGRAMA DE PÓS - GRADUAÇÃO EM ZOOLOGIA O HÁBITO ALIMENTAR D OS MORCEGOS (Mammalia, Chiroptera) E SUA RELAÇÃO COM A DIVERSIDADE VIRAL PAULA GALVÃO TEIXEIRA BRASÍLIA, DF 2016 UNIVERSIDADE DE BRASÍLIA INSTITUTO DE CIÊNCIAS BIOLÓGICAS PROGRAMA DE PÓS - GRADUAÇÃO EM ZOOLOGIA O HÁBITO ALIMENTAR D OS MORCEGOS (Mammalia, Chiroptera) E SUA RELAÇÃO COM A DIVERSIDADE VIRAL PAULA GALVÃO TEIXEIRA Orientador a: Prof. Dra. Ludmilla M. S. Aguiar Coorientador: Dr. Fernando Lucas Melo Dissertação apresentada ao programa de Pós - Graduação em Zoologia do Instituto de Ciências Biológicas da Universidade de Brasília como requisito parcial à obtenção do título de Mestr e em Zoologia. BRASÍLIA, DF 2016 Dedico este trabalho a todos os morcegos que perderam suas vidas a fim de possibilitar que o mundo os conhecesse um pouco melhor. Com certeza não foi em vão. AGRADECIMENTOS Voltar para a universidade depois de dez anos de formada, foi um desafio. Encarar um mestrado em área diferente a da minha formação, Medicina Veterinária, foi um desafio ainda maior. Confesso que nunca me interessei pela área acadêmica, mas como amante dos animais que sempre fui, me sinto extremamente gratificada por contribuir para que se conheça mais sobre a vida dos morcegos. Mas, por que logo os morcegos, que não passaram nem perto do meu currículo no curso de Medicina Veterinária? E aqui começam os meu s agradecimentos, primeiramente ao IBAMA, não só por ter concedido o meu afastamento integral, como também por despertar em mim, ao longo dos quase nove anos de carreira, o interesse pelos animais silvestres. -

A Taxonomic Review of Hipposideros Halophyllus Hill and Yenbutra, 1984
A Taxonomic Review of Hipposideros halophyllus Hill and Yenbutra, 1984, Hipposideros ater Templeton, 1848, and Hipposideros cineraceus Blyth, 1853 (Chiroptera: Hipposideridae) in Thailand and Myanmar Bounsavane Douangboubpha A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Science in Ecology (International Program) Prince of Songkla University 2008 Copyright of Prince of Songkla University i Thesis Title A Taxonomic Review of Hipposideros halophyllus Hill and Yenbutra, 1984, Hipposideros ater Templeton, 1848, and Hipposideros cineraceus Blyth, 1853 (Chiroptera: Hipposideridae) in Thailand and Myanmar Author Mr. Bounsavane Douangboubpha Major Program Ecology (International Program) Major Advisor Examining Committee: ………………………………………. .....………………………...Committee (Asst. Prof. Dr. Sara Bumrungsri) (Assoc. Prof. Dr. Kitichate Sridith) .....………………………...Committee Co-advisor (Dr. Chavalit Vidthayanon) ………………………………………. .....………………………...Committee (Assoc. Prof. Dr. Chutamas Satasook) (Asst. Prof. Dr. Sara Bumrungsri) ………………………………………. .....………………………...Committee (Dr. Paul J. J. Bates) (Assoc. Prof. Dr. Chutamas Satasook) The Graduate School, Prince of Songkla University, has approved this thesis as partial fulfillment of the requirements for the Master of Science Degree in Ecology (International Program). ………………………………………... (Assoc. Prof. Dr. Krerkchai Thongnoo) Dean of Graduate School ii Thesis Title A Taxonomic Review of Hipposideros halophyllus Hill and Yenbutra, 1984, Hipposideros ater Templeton, 1848, and -

O Hábito Alimentar Dos Morcegos
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Repositório Institucional da Universidade de Brasília UNIVERSIDADE DE BRASÍLIA INSTITUTO DE CIÊNCIAS BIOLÓGICAS PROGRAMA DE PÓS - GRADUAÇÃO EM ZOOLOGIA O HÁBITO ALIMENTAR D OS MORCEGOS (Mammalia, Chiroptera) E SUA RELAÇÃO COM A DIVERSIDADE VIRAL PAULA GALVÃO TEIXEIRA BRASÍLIA, DF 2016 UNIVERSIDADE DE BRASÍLIA INSTITUTO DE CIÊNCIAS BIOLÓGICAS PROGRAMA DE PÓS - GRADUAÇÃO EM ZOOLOGIA O HÁBITO ALIMENTAR D OS MORCEGOS (Mammalia, Chiroptera) E SUA RELAÇÃO COM A DIVERSIDADE VIRAL PAULA GALVÃO TEIXEIRA Orientador a: Prof. Dra. Ludmilla M. S. Aguiar Coorientador: Dr. Fernando Lucas Melo Dissertação apresentada ao programa de Pós - Graduação em Zoologia do Instituto de Ciências Biológicas da Universidade de Brasília como requisito parcial à obtenção do título de Mestr e em Zoologia. BRASÍLIA, DF 2016 Dedico este trabalho a todos os morcegos que perderam suas vidas a fim de possibilitar que o mundo os conhecesse um pouco melhor. Com certeza não foi em vão. AGRADECIMENTOS Voltar para a universidade depois de dez anos de formada, foi um desafio. Encarar um mestrado em área diferente a da minha formação, Medicina Veterinária, foi um desafio ainda maior. Confesso que nunca me interessei pela área acadêmica, mas como amante dos animais que sempre fui, me sinto extremamente gratificada por contribuir para que se conheça mais sobre a vida dos morcegos. Mas, por que logo os morcegos, que não passaram nem perto do meu currículo no curso de Medicina Veterinária? E aqui começam os meu s agradecimentos, primeiramente ao IBAMA, não só por ter concedido o meu afastamento integral, como também por despertar em mim, ao longo dos quase nove anos de carreira, o interesse pelos animais silvestres. -

A Common Name for the Bat Family Rhinonycteridae—The Trident Bats
Zootaxa 4179 (1): 115–117 ISSN 1175-5326 (print edition) http://www.mapress.com/j/zt/ Correspondence ZOOTAXA Copyright © 2016 Magnolia Press ISSN 1175-5334 (online edition) http://doi.org/10.11646/zootaxa.4179.1.7 http://zoobank.org/urn:lsid:zoobank.org:pub:7085A89F-8EEE-45DB-B0E2-E42EAC124507 A common name for the bat family Rhinonycteridae—the Trident Bats KYLE N. ARMSTRONG1,2,8, STEVEN M. GOODMAN3,4, PETR BENDA5,6 & SUZANNE J. HAND7 1Australian Centre for Evolutionary Biology and Biodiversity, University of Adelaide, South Australia 5005. E-mail: [email protected] 2South Australian Museum, Adelaide, South Australia 5000. 3Field Museum of Natural History, 1400 South Lake Shore Drive, Chicago, Illinois 60605, USA. E-mail: [email protected] 4Association Vahatra, BP 3972, Antananarivo 101, Madagascar. 5Department of Zoology, National Museum (Natural History), Vaclavske nam. 68, 115 79 Praha 1, Czech Republic. E-mail: [email protected] 6Department of Zoology, Faculty of Science, Charles University, Vinicna 7, 128 44 Praha 2, Czech Republic. 7PANGEA (Palaeontology, Geobiology and Earth Archives) Research Centre, School of Biological, Earth and Environmental Sciences, UNSW Australia, Sydney, 2052. E-mail: [email protected] 8Corresponding author Recent elevation in the rank of J.E. Gray’s (1866) ‘Leaf-nosed Bats’ the Rhinonycterina to family level recognised the phylogenetic uniqueness of bats in the extant genera Cloeotis, Paratriaenops, Rhinonicteris and Triaenops, and the fossil genera Brachipposideros and Brevipalatus (Foley et al. 2015). In the systematic summary of that paper, attention was drawn to the issue of correct nomenclature because of past ambiguity around the appropriate spelling of the type genus Rhinonicteris (see also Simmons 2005; Armstrong 2006). -

Diversity and Diversification Across the Global Radiation of Extant Bats
Diversity and Diversification Across the Global Radiation of Extant Bats by Jeff J. Shi A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Ecology and Evolutionary Biology) in the University of Michigan 2018 Doctoral Committee: Professor Catherine Badgley, co-chair Assistant Professor and Assistant Curator Daniel Rabosky, co-chair Associate Professor Geoffrey Gerstner Associate Research Scientist Miriam Zelditch Kalong (Malay, traditional) Pteropus vampyrus (Linnaeus, 1758) Illustration by Gustav Mützel (Brehms Tierleben), 19271 1 Reproduced as a work in the public domain of the United States of America; accessible via the Wikimedia Commons repository. EPIGRAPHS “...one had to know the initial and final states to meet that goal; one needed knowledge of the effects before the causes could be initiated.” Ted Chiang; Story of Your Life (1998) “Dr. Eleven: What was it like for you, at the end? Captain Lonagan: It was exactly like waking up from a dream.” Emily St. John Mandel; Station Eleven (2014) Bill Watterson; Calvin & Hobbes (October 27, 1989)2 2 Reproduced according to the educational usage policies of, and direct correspondence with Andrews McMeel Syndication. © Jeff J. Shi 2018 [email protected] ORCID: 0000-0002-8529-7100 DEDICATION To the memory and life of Samantha Jade Wang. ii ACKNOWLEDGMENTS All of the research presented here was supported by a National Science Foundation (NSF) Graduate Research Fellowship, an Edwin H. Edwards Scholarship in Biology, and awards from the University of Michigan’s Rackham Graduate School and the Department of Ecology & Evolutionary Biology (EEB). A significant amount of computational work was funded by a Michigan Institute for Computational Discovery and Engineering fellowship; specimen scanning, loans, and research assistants were funded by the Museum of Zoology’s Hinsdale & Walker fund and an NSF Doctoral Dissertation Improvement Grant. -

A Comparative Genomics Multitool for Scientific Discovery and Conservation
Analysis https://doi.org/10.1038/s41586-020-2876-6 Supplementary information A comparative genomics multitool for scientific discovery and conservation In the format provided by the authors and unedited Nature | www.nature.com/nature Supplementary Table 1 Supplementary Table 1. Genome assembly statistics for all attemped and successful Zoonomia Project genomes. Of 173 species and subspecies initially planned for inclusion in the Zoonomia Project, genome assemblies have been generated and released for 132. For the remainder, acquisition of high quality samples was a major impediment. Set A: Discovar only genomes; Set B: Genomes upgraded to longer contiguity; Set C: Assembly failed; Set D: Sample failed QC; Set E: Sample not found; ** Genome assembly statistics output by DISCOVAR de novo. All samples were collected and shipped in compliance with the applicable regulations for sample collection, transfer, export and import. Contig Size (Gb; Mean Busco BUSCO Provider Provider Sequencing N50 (bp) Scaffold contigs base Complete Single BUSCO BUSCO BUSCO Set Species Common Name Order Family IUCN Biosample Institution contact location Genbank accession ** N50 (bp)** >1kb)** quality** Coverage** (n=4104) Copy Duplicated Fragmented Missing Liverpool Solenodon Hispaniolan School of Nicholas Uppsala A Eulipotyphla Solenodontidae Endangered SAMN07678062 GCA_004363575.1 244,273 422,311 2.05 35.8 29.3 90.4% 90.1% 0.3% 6.9% 2.7% paradoxus solenodon Tropical Casewell University Medicine Crocidura Indochinese University of Kevin Uppsala A Eulipotyphla -
Hipposideridae
FAUNA of AUSTRALIA 41. HIPPOSIDERIDAE LESLIE S. HALL 1 41. HIPPOSIDERIDAE 2 41. HIPPOSIDERIDAE DEFINITION AND GENERAL DESCRIPTION Like their close relatives, the rhinolophids, members of the Hipposideridae possess an ornate noseleaf and have broad mobile ears. The noseleaf is basically a horseshoe shape, but it lacks a definite lancet and there is no structure that might be construed as the equivalent of the rhinolophid sella. Behind the anterior leaf, there is an intermediate swollen area which sometimes has a small central projection or ‘wart’. The intermediate leaf forms a base for a thinner, more elaborate, erect posterior element. This posterior leaf is not pointed, as in rhinolophids, but is usually rounded or flat across the top. In addition, the face of the posterior leaf may have several thin-walled compartments. The complexity of the noseleaf may be further enhanced by secondary foliations of skin from under the edges of the horseshoe. In general, most hipposiderids are some shade of brown or reddish-brown, but fur colour can vary intraspecifically. The Orange Horseshoe-bat, Rhinonycteris aurantius, can be bright orange, brown, to almost white with brown tips. The Diadem Horseshoe-bat, Hipposideros diadema, often has pale shoulder patches. The internal morphology of this group is similar to that of the Rhinolophidae, but the pectoral and pelvic girdles are more highly modified, the toes have two phalanges each and the lumbar vertebrae show a marked tendency to become fused into a solid rod. In the pectoral girdle, the fusion of the first and second ribs involves the entire bone, up to and including the corresponding thoracic vertebrae. -

Binningup Bat Survey
Fortescue North Star Survey – April 2013 Fortescue Metals Group North Star Project, Pilbara leaf-nosed bat colony survey April 2013 Prepared for Fortescue Metals Group Limited Bat Call WA Pty Ltd ABN 26 146 117 839 43 Murray Drive Hillarys Western Australia 6025 [email protected] +61 8 9402 1987 +61 488 930 735 Prepared by: R. D. Bullen – Bat Call WA Issue 2 18 July 2013 This document has been prepared to the requirements of Fortescue Metals Group. It may be cited for the purposes of scientific research or other reasonable use. It may not be reproduced or distributed to any third party by hardcopy or electronic means without the permission of the client or Bat Call WA. BAT CALL WA 1 of 38 18/07/2013 Fortescue North Star Survey – April 2013 Contents Executive Summary 4 Introduction 6 Project Background Climate Topography and Geology Surface Water Bats of conservation significance The Pilbara leaf-nosed bat Scope of Works Summary of previous district fauna surveys that detected Pilbara leaf-nosed bats Methodology 14 Survey team Survey timing and weather Habitat assessment Cave Assessment Bat observations Survey Limitations Results 20 Activity at cave 13 Activity at caves 2, 11 and 14 on the deposit Activity at cave 6 and other sites Pilbara leaf-nosed bat dispersal pattern Other conservation significant species detected during the study Discussion of Results 29 References 31 Appendix A SM2 audio settings used during the survey Appendix B Bat detection site details Appendix C Characteristics of caves assessed during this study BAT CALL WA 2 of 38 18/07/2013 Fortescue North Star Survey – April 2013 List of Tables Table 1 Summary of Pilbara leaf-nosed bat records in the North Star district Table 2 Caves nominated as potential Pilbara leaf-nosed bat roosts at North Star Table 3 Criteria for categorising bat records into activity levels. -

Published Version
PUBLISHED VERSION Nicole M. Foley, Vu Dinh Thong, Pipat Soisook, Steven M. Goodman, Kyle N. Armstrong, David S. Jacobs, Sébastien J. Puechmaille and Emma C. Teeling How and why overcome the impediments to resolution: lessons from rhinolophid and hipposiderid bats Molecular Biology and Evolution, 2015; 32(2):313-333 © The Author 2014. Published by Oxford University Press on behalf of the Society for Molecular Biology and Evolution. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits non-commercial re-use, distribution, and reproduction in any medium, provided the original work is properly cited. Originally published at: http://doi.org/10.1093/molbev/msu329 PERMISSIONS http://creativecommons.org/licenses/by-nc/4.0/ 2 December 2016 http://hdl.handle.net/2440/102268 How and Why Overcome the Impediments to Resolution: Lessons from rhinolophid and hipposiderid Bats Nicole M. Foley,1 Vu Dinh Thong,2 Pipat Soisook,3 Steven M. Goodman,4,5 Kyle N. Armstrong,6,7 David S. Jacobs,8 Sebastien J. Puechmaille,*,y,1,9 and Emma C. Teeling*,y,1 1School of Biology & Environmental Science, University College Dublin, Belfield, Dublin, Ireland 2Institute of Ecology and Biological Resources, Vietnam Academy of Science and Technology, Hanoi, Vietnam 3Princess Maha Chakri Sirindhorn Natural History Museum, Prince of Songkla University, Hat Yai, Songkhla, Thailand 4Field Museum of Natural History, Chicago, IL, USA 5Association Vahatra, Antananarivo, Madagascar 6Australian Centre for Evolutionary Biology & Biodiversity, The University of Adelaide, Adelaide, South Australia, Australia 7South Australian Museum, Adelaide, South Australia, Australia 8Department of Biological Sciences, University of Cape Town, Rondebosch, South Africa 9Zoological Institute and Museum, Greifswald University, Greifswald, Germany y These authors are co-senior authors. -

Lessons from Rhinolophid and Hipposiderid Bats
How and Why Overcome the Impediments to Resolution: Lessons from rhinolophid and hipposiderid Bats Nicole M. Foley,1 Vu Dinh Thong,2 Pipat Soisook,3 Steven M. Goodman,4,5 Kyle N. Armstrong,6,7 David S. Jacobs,8 Sebastien J. Puechmaille,*,y,1,9 and Emma C. Teeling*,y,1 1School of Biology & Environmental Science, University College Dublin, Belfield, Dublin, Ireland 2Institute of Ecology and Biological Resources, Vietnam Academy of Science and Technology, Hanoi, Vietnam 3Princess Maha Chakri Sirindhorn Natural History Museum, Prince of Songkla University, Hat Yai, Songkhla, Thailand 4Field Museum of Natural History, Chicago, IL, USA 5Association Vahatra, Antananarivo, Madagascar 6Australian Centre for Evolutionary Biology & Biodiversity, The University of Adelaide, Adelaide, South Australia, Australia 7South Australian Museum, Adelaide, South Australia, Australia 8Department of Biological Sciences, University of Cape Town, Rondebosch, South Africa 9Zoological Institute and Museum, Greifswald University, Greifswald, Germany yThese authors are co-senior authors. *Corresponding author: E-mail: [email protected]; [email protected]. Associate editor: Claudia Russo Abstract The phylogenetic and taxonomic relationships among the Old World leaf-nosed bats (Hipposideridae) and the closely related horseshoe bats (Rhinolophidae) remain unresolved. In this study, we generated a novel approximately 10-kb molecular data set of 19 nuclear exon and intron gene fragments for 40 bat species to elucidate the phylogenetic relationships within the families Rhinolophidae and Hipposideridae. We estimated divergence times and explored po- tential reasons for any incongruent phylogenetic signal. We demonstrated the effects of outlier taxa and genes on phylogenetic reconstructions and compared the relative performance of intron and exon data to resolve phylogenetic relationships. -

HANDBOOK of the MAMMALS of the WORLD Families of Volume 9: Bats
HANDBOOK OF THE MAMMALS OF THE WORLD Families of Volume 9: Bats Family Family English Subfamily Tribe Group name Species Genera Scientific name name number Megaerops Short-nosed Fruit Cynopterini 14 species Cynopterus Bats and relatives Ptenochirus Cynopterinae Dyacopterus Sphaerias Balionycteris Aethalops Pygmy Fruit Bats and Thoopterus Balionycterini 17 species Alionycteris relatives Haplonycteris Otopteropus Latidens Chironax Penthetor African Rainforest Scotonycteris Scotonycterini 6 species Fruit Bats Casinycteris Eonycterini Dawn Bats 3 species Eonycteris Old World Fruit PTEROPODIDAE Bats Rousettini Roussette Fruit Bats 8 species Rousettus Rousettinae Stenonycterini Long-haired Fruit Bat 1 species Stenonycteris Megaloglossus Collared Fruit Bats Myonycterini 7 species Lissonycteris and relatives Myonycteris Plerotini Broad-faced Fruit Bat 1 species Plerotes Hypsignathus Epauletted Fruit Bats Epomops Epomophorini 15 species and relatives Nanonycteris Epomophorus Family Family English Subfamily Tribe Group name Species Genera Scientific name name number Long-tongued Macroglossus Macroglossinae 5 species Blossom Bats Syconycteris Boneia Harpy and Bare- Harpyionycteris Harpyionycterinae 17 species backed Fruit Bats Aproteles Dobsonia Straw-colored Fruit Eidolinae 2 species Eidolon Bats Old World Fruit PTEROPODIDAE Bats Tube-nosed Fruit Paranyctimene Nyctimeninae 17 species Bats Nyctimene Notopterinae Long-tailed Fruit Bats 2 species Notopteris Desmalopex Mirimiri Pteralopex Melonycteris Flying Foxes and Pteropodinae 76 species Nesonycteris