6-Local Anesthetics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 11 Local Anesthetics
Chapter LOCAL ANESTHETICS 11 Kenneth Drasner HISTORY MECHANISMS OF ACTION AND FACTORS ocal anesthesia can be defined as loss of sensation in AFFECTING BLOCK L a discrete region of the body caused by disruption of Nerve Conduction impulse generation or propagation. Local anesthesia can Anesthetic Effect and the Active Form of the be produced by various chemical and physical means. Local Anesthetic However, in routine clinical practice, local anesthesia is Sodium Ion Channel State, Anesthetic produced by a narrow class of compounds, and recovery Binding, and Use-Dependent Block is normally spontaneous, predictable, and complete. Critical Role of pH Lipid Solubility Differential Local Anesthetic Blockade Spread of Local Anesthesia after Injection HISTORY PHARMACOKINETICS Cocaine’s systemic toxicity, its irritant properties when Local Anesthetic Vasoactivity placed topically or around nerves, and its substantial Metabolism potential for physical and psychological dependence gene- Vasoconstrictors rated interest in identification of an alternative local 1 ADVERSE EFFECTS anesthetic. Because cocaine was known to be a benzoic Systemic Toxicity acid ester (Fig. 11-1), developmental strategies focused Allergic Reactions on this class of chemical compounds. Although benzo- caine was identified before the turn of the century, its SPECIFIC LOCAL ANESTHETICS poor water solubility restricted its use to topical anesthe- Amino-Esters sia, for which it still finds some limited application in Amino-Amide Local Anesthetics modern clinical practice. The -
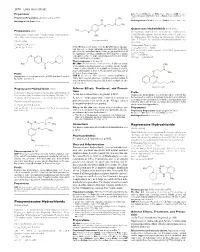
Proxymetacaine Hydrochloride Ropivacaine Hydrochloride
1870 Local Anaesthetics Preparations pore: Alcaine; Switz.: Alcaine; Turk.: Alcaine; Opticaine; USA: Ak-Taine; Alcaine; Ocu-Caine; Ophthetic; Parcaine; Venez.: Alcaine; Oftaine†; Poen- (details are given in Part 3) caina. Proprietary Preparations CH3 Multi-ingredient: Spain: Detraine. O Multi-ingredient: Canad.: Fluoracaine†; USA: Fluoracaine; Fluorocaine. N CH3 O Quinisocaine Hydrochloride (BANM, rINNM) H3C Propipocaine (rINN) O Chinisocainum Hydrochloride; Dimethisoquin Hydrochloride Propipocaína; Propipocaïne; Propipocainum; Propoxypipero- (USAN); Dimethisoquinium Chloride; Hidrocloruro de quinisocaí- NH2 caine. 3-Piperidino-4′-propoxypropiophenone. na; Quinisocaïne, Chlorhydrate de; Quinisocaini Hydrochlori- (proxymetacaine) dum. 2-(3-Butyl-1-isoquinolyloxy)-NN-dimethylethylamine hy- Пропипокаин drochloride. C17H25NO2 = 275.4. Хинизокаина Гидрохлорид CAS — 3670-68-6. NOTE. PROX is a code approved by the BP 2008 for use on single unit doses of eye drops containing proxymetacaine hydrochlo- C17H24N2O,HCl = 308.8. ride where the individual container may be too small to bear all CAS — 86-80-6 (quinisocaine); 2773-92-4 (quinisocaine the appropriate labelling information. PROXFLN is a similar hydrochloride). O code approved for eye drops containing proxymetacaine hydro- ATC — D04AB05. chloride and fluorescein sodium. ATC Vet — QD04AB05. N Pharmacopoeias. In Br. and US. BP 2008 (Proxymetacaine Hydrochloride). A white or almost H3C CH3 white, odourless or almost odourless, crystalline powder. Soluble O in water and in chloroform; very soluble in dehydrated alcohol; N practically insoluble in ether. A 1% solution in water has a pH of O CH Profile 5.7 to 6.4. Protect from light. 3 Propipocaine is a local anaesthetic (p.1850) that has been used USP 31 (Proparacaine Hydrochloride). A white to off-white, or for surface anaesthesia. -

8–16–01 Vol. 66 No. 159 Thursday Aug. 16, 2001 Pages 42929
8–16–01 Thursday Vol. 66 No. 159 Aug. 16, 2001 Pages 42929–43064 VerDate 11-MAY-2000 19:13 Aug 15, 2001 Jkt 194001 PO 00000 Frm 00001 Fmt 4710 Sfmt 4710 E:\FR\FM\16AUWS.LOC pfrm11 PsN: 16AUWS 1 II Federal Register / Vol. 66, No. 159 / Thursday, August 16, 2001 The FEDERAL REGISTER is published daily, Monday through SUBSCRIPTIONS AND COPIES Friday, except official holidays, by the Office of the Federal Register, National Archives and Records Administration, PUBLIC Washington, DC 20408, under the Federal Register Act (44 U.S.C. Subscriptions: Ch. 15) and the regulations of the Administrative Committee of Paper or fiche 202–512–1800 the Federal Register (1 CFR Ch. I). The Superintendent of Assistance with public subscriptions 512–1806 Documents, U.S. Government Printing Office, Washington, DC 20402 is the exclusive distributor of the official edition. General online information 202–512–1530; 1–888–293–6498 Single copies/back copies: The Federal Register provides a uniform system for making available to the public regulations and legal notices issued by Paper or fiche 512–1800 Federal agencies. These include Presidential proclamations and Assistance with public single copies 512–1803 Executive Orders, Federal agency documents having general FEDERAL AGENCIES applicability and legal effect, documents required to be published Subscriptions: by act of Congress, and other Federal agency documents of public interest. Paper or fiche 523–5243 Assistance with Federal agency subscriptions 523–5243 Documents are on file for public inspection in the Office of the Federal Register the day before they are published, unless the issuing agency requests earlier filing. -

WO 2016/140629 Al 9 September 2016 (09.09.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2016/140629 Al 9 September 2016 (09.09.2016) P O P C T (51) International Patent Classification: (74) Agent: BULUT, Pinar; FarmaPatent Limited Sirketi, A61K 36/28 (2006.01) A61P 17/02 (2006.01) GMK Bulvari No:42/5, Maltepe, 06440 Ankara (TR). A61K 36/38 (2006.01) A61P 23/00 (2006.01) (81) Designated States (unless otherwise indicated, for every A61K 31/167 (2006.01) kind of national protection available): AE, AG, AL, AM, (21) International Application Number: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, PCT/TR20 15/000088 BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 5 March 2015 (05.03.2015) KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (25) Filing Language: English MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, (26) Publication Language: English SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, (71) Applicant: PHARMACTFVE ILAC SANAYI VE Tl- TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. CARET A. S. [TR/TR]; Mahmutbey Mah. Dilmenler Cad., (84) Designated States (unless otherwise indicated, for every Aslanoba Plaza No: 19 K:3, Bagcilar/istanbul (TR). -

Title 16. Crimes and Offenses Chapter 13. Controlled Substances Article 1
TITLE 16. CRIMES AND OFFENSES CHAPTER 13. CONTROLLED SUBSTANCES ARTICLE 1. GENERAL PROVISIONS § 16-13-1. Drug related objects (a) As used in this Code section, the term: (1) "Controlled substance" shall have the same meaning as defined in Article 2 of this chapter, relating to controlled substances. For the purposes of this Code section, the term "controlled substance" shall include marijuana as defined by paragraph (16) of Code Section 16-13-21. (2) "Dangerous drug" shall have the same meaning as defined in Article 3 of this chapter, relating to dangerous drugs. (3) "Drug related object" means any machine, instrument, tool, equipment, contrivance, or device which an average person would reasonably conclude is intended to be used for one or more of the following purposes: (A) To introduce into the human body any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (B) To enhance the effect on the human body of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; (C) To conceal any quantity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state; or (D) To test the strength, effectiveness, or purity of any dangerous drug or controlled substance under circumstances in violation of the laws of this state. (4) "Knowingly" means having general knowledge that a machine, instrument, tool, item of equipment, contrivance, or device is a drug related object or having reasonable grounds to believe that any such object is or may, to an average person, appear to be a drug related object. -

Local Anesthetics
Local Anesthetics Introduction and History Cocaine is a naturally occurring compound indigenous to the Andes Mountains, West Indies, and Java. It was the first anesthetic to be discovered and is the only naturally occurring local anesthetic; all others are synthetically derived. Cocaine was introduced into Europe in the 1800s following its isolation from coca beans. Sigmund Freud, the noted Austrian psychoanalyst, used cocaine on his patients and became addicted through self-experimentation. In the latter half of the 1800s, interest in the drug became widespread, and many of cocaine's pharmacologic actions and adverse effects were elucidated during this time. In the 1880s, Koller introduced cocaine to the field of ophthalmology, and Hall introduced it to dentistry Overwiev Local anesthetics (LAs) are drugs that block the sensation of pain in the region where they are administered. LAs act by reversibly blocking the sodium channels of nerve fibers, thereby inhibiting the conduction of nerve impulses. Nerve fibers which carry pain sensation have the smallest diameter and are the first to be blocked by LAs. Loss of motor function and sensation of touch and pressure follow, depending on the duration of action and dose of the LA used. LAs can be infiltrated into skin/subcutaneous tissues to achieve local anesthesia or into the epidural/subarachnoid space to achieve regional anesthesia (e.g., spinal anesthesia, epidural anesthesia, etc.). Some LAs (lidocaine, prilocaine, tetracaine) are effective on topical application and are used before minor invasive procedures (venipuncture, bladder catheterization, endoscopy/laryngoscopy). LAs are divided into two groups based on their chemical structure. The amide group (lidocaine, prilocaine, mepivacaine, etc.) is safer and, hence, more commonly used in clinical practice. -

Local Anesthetics – Substances with Multiple Application in Medicine
ISSN 2411-958X (Print) European Journal of January-April 2016 ISSN 2411-4138 (Online) Interdisciplinary Studies Volume 2, Issue 1 Local Anesthetics – Substances with Multiple Application in Medicine Rodica SÎRBU Ovidius University of Constanta, Faculty of Pharmacy, Campus Corp B, University Alley No. 1, Constanta, Romania Emin CADAR UMF Carol Davila Bucharest, Faculty of Pharmacy, Str. Traian Vuia No. 6, Sector 2, Bucharest, Romania Cezar Laurențiu TOMESCU Ovidius University of Constanta, Faculty of Medicine, Campus Corp B, University Alley No. 1, Constanta, Romania Cristina-Luiza ERIMIA Corresponding author, [email protected] Ovidius University of Constanta, Faculty of Pharmacy, Campus Corp B, University Alley No. 1, Constanta, Romania Stelian PARIS Ovidius University of Constanta, Faculty of Pharmacy, Campus Corp B, University Alley No. 1, Constanta, Romania Aneta TOMESCU Ovidius University of Constanta, Faculty of Medicine, Campus Corp B, University Alley No. 1, Constanta, Romania Abstract Local anesthetics are substances which, by local action groups on the runners, cause loss of reversible a painful sensation, delimited corresponding to the application. They allow small surgery, short in duration and the endoscopic maneuvers. May be useful in soothe teething pain of short duration and in the locking of the nervous disorders in medical care. Local anesthesia is a process useful for the carrying out of surgery and of endoscopic maneuvers, to soothe teething pain in certain conditions, for depriving the temporary structures peripheral nervous control. Reversible locking of the transmission nociceptive, the set of the vegetative and with a local anesthetic at the level of the innervations peripheral nerve, roots and runners, a trunk nervous, around the components of a ganglion or coolant is cefalorahidian practice anesthesia loco-regional. -

Pharmaceutical Appendix to the Tariff Schedule 2
Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2007) (Rev. 2) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM LIDADRONICUM 63132-38-7 ABAFUNGIN 129639-79-8 ACIDUM SALCAPROZICUM 183990-46-7 ABAMECTIN 65195-55-3 ACIDUM SALCLOBUZICUM 387825-03-8 ABANOQUIL 90402-40-7 ACIFRAN 72420-38-3 ABAPERIDONUM 183849-43-6 ACIPIMOX 51037-30-0 ABARELIX 183552-38-7 ACITAZANOLAST 114607-46-4 ABATACEPTUM 332348-12-6 ACITEMATE 101197-99-3 ABCIXIMAB 143653-53-6 ACITRETIN 55079-83-9 ABECARNIL 111841-85-1 ACIVICIN 42228-92-2 ABETIMUSUM 167362-48-3 ACLANTATE 39633-62-0 ABIRATERONE 154229-19-3 ACLARUBICIN 57576-44-0 ABITESARTAN 137882-98-5 ACLATONIUM NAPADISILATE 55077-30-0 ABLUKAST 96566-25-5 ACODAZOLE 79152-85-5 ABRINEURINUM 178535-93-8 ACOLBIFENUM 182167-02-8 ABUNIDAZOLE 91017-58-2 ACONIAZIDE 13410-86-1 ACADESINE 2627-69-2 ACOTIAMIDUM 185106-16-5 ACAMPROSATE 77337-76-9 -

Anesthetics; Drugs of Abuse & Withdrawal
Anesthetics; Drugs of Abuse & Withdrawal Kurt Kleinschmidt, MD, FACEP, FACMT Professor of Emergency Medicine Section Chief and Program Director Medical Toxicology UT Southwestern Medical Center Much Thanks To… Sean M. Bryant, MD Associate Professor Cook County Hospital (Stroger) Department of Emergency Medicine Assistant Fellowship Director: Toxikon Consortium Associate Medical Director Illinois Poison Center Overview Anesthetics – Local – Inhalational – NM Blockers & Malignant Hyperthermia Drugs of Abuse (Pearls) Withdrawal History 1904-Procaine (short Duration of Action) 1925 (dibucaine) & 1928 (tetracaine) → potent, long acting 1943-lidocaine 1956-mepivacaine, 1959-prilocaine 1963-bupivacaine, 1971-etidocaine, 1996-ropivacaine Lipophili Intermediate Amine Substituents c Group Esters Structure 2 Distinct Groups 1) Amino Esters Amides 2) Amino Amides Local Anesthetics Toxic Reactions • Few & iatrogenic • Blood vessel administration or toxic dose AMIDES have largely replaced ESTERS • Increased stability • Relative absence of hypersensitivity reactions – ESTER hydrolysis = PABA (cross sensitivity) – AMIDES = Multidose preps → methylparabens • Chemically related to PABA with rare allergic reactions Local Anesthetics Mode of Action • Reversible & Predictable Binding • Within membrane-bound sodium channels of conducting tissue (cytoplasmic side of membrane) → Failure to form/propagate action potentials (Small-diam. fibersBLOCKADE carrying pain/temp sensation) Pain fibers - higher firing rate & longer AP → • ↑Sodium susceptible Channelto local -

Clinical Use and Toxicity of Local Anaesthetics
716 Review Articles Medical Education Clinical use and toxicity W. Zink · M. Ulrich of local anaesthetics Citation: Zink W, Ulrich M: Clinical use and toxicity of local anaesthetics. Anästh Intensivmed 2018;59:716727. DOI: 10.19224/ai2018.716 Summary were an early driving force in the develop ment of new substances [1,2]. Once Local anaesthetics are widely used in the chemical structure of cocaine had contemporary clinical practice. Regard been established, attempts were made to less of their specific physicochemical reduce its toxicity by changing the mo properties and chemical structures, all lecular structure – an undertaking which local anaesthetic agents block neuro succeeded in 1905 when procaine, a syn nal voltagegated sodium channels, thetic amino ester local anaesthetic, was suppressing conduction in peripheral synthesised. To this day, that substance nerves. Furthermore, these agents are is used as a reference standard for local characterised by numerous (sub)cellular anaesthetic potency. A further milestone effects. Despite the fact that local anaes was reached when in 1943 lidocaine, thetics with markedly decreased toxic one of the first amino amide type local potential have been developed, systemic anaesthetics, was introduced into clinical intoxication still may be lifethreatening. practice. Amino amide type local anaes Amongst other things, this severe com thetics provide a longer duration of action plication is the result of an unselective and are chemically more stable than ester block of neuronal and cardiac sodium types and so gained increasing clinical channels following excessive systemic significance in the decades that followed. accumulation, impairing central nervous In 1979, however, toxicity hinted at a and cardiac function. -

Local Anaesthesia Outside the Operating Room
SEMINAR PAPER SK Chan MK Karmakar Local anaesthesia outside the operating PT Chui room !"#$%&' ○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○ An increasing number of minor surgical procedures are performed under local anaesthesia in clinical settings outside the operating room, where monitoring and resuscitation equipment—as well as personnel skilled in resuscitation—may not be readily available. Serious adverse effects and even fatalities may result from the use of local anaesthetic agents, arising from a variety of causes such as systemic toxicity, allergy, vasovagal syncope, and reaction to additives present in the local anaesthetic. This article briefly reviews the pharmacology of local anaesthetic agents, and describes various techniques commonly used for local anaesthesia, with special emphasis on safety. Clinical features of toxicity, and its differential diagnosis and management, are also discussed. !"#$%&'()*+ ,-./0123456789:;<=#> !"#$%&'()*+,-./0123 4567894:;<1 = !"#$%&'(&)*+,-./0&123456789:$;<=> !"#$%&'()*+,-./012345)6789*+,-/:; !"#$%&'()*+,-./'012!3 456789:;<= Introduction Since the introduction of cocaine into clinical practice by Koller in 1884, the history of surgery has changed dramatically. Pain-free surgery can now be accomplished under local anaesthesia, with improved patient comfort and cooperation. Local anaesthesia is defined as the reversible loss of sensation in a relatively small or circumscribed area of the body, achieved by topical Key words: application or injection of agents that either depress the excitation -

Articaine: a New Alternative in Dental Hygiene Pain Control
Source: Journal of Dental Hygiene, Vol. 81, No. 3, July 2007 Copyright by the American Dental Hygienists© Association Articaine: A New Alternative in Dental Hygiene Pain Control Pamela R Overman, EdD, RDH Pamela R. Overman, EdD, RDH is Associate Professor and Associate Dean for Academic Affairs at UMKC School of Dentistry. Purpose. Local anesthesia administration is integral to pain control in dental hygiene. As of 2006, 40 licensing jurisdictions in the United States include local anesthesia administration in the scope of dental hygiene practice. While the risks associated with use of intraoral local anesthesia are not great, careful attention to recommended practices helps foster patient safety. As new products are introduced, it is important to study their advantages and limitations to see where they fit into dental hygiene practice. An amide local anesthetic agent, articaine, that has been available in Europe for over 20 years, was approved for US distribution in 2000. Methods. The purpose of this article is to review the current peer reviewed literature on the characteristics of articaine so it can be incorporated into dental hygiene practice when indicated. Results. Rather than simply using one agent for all procedures, patient care is enhanced when local anesthetics are selected based on the unique needs of the procedure, the patient and with safety and effectiveness in mind. Keywords: Local anesthetics, analgesia and anesthesia, dental hygiene car, pain control Introduction The first edition of what came to be a classic textbook in dental hygiene, Clinical Practice of the Dental Hygienist,1 was published in 1959. Esther Wilkins, RDH, DMD, and Patricia McCullough, RDH, devoted one page to the topic of pain control during scaling procedures.