Health Systems Readiness to Provide Geriatric Friendly Care Services In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Gomba District Hazard, Risk and Vulnerability Profi Le
Gomba District Hazard, Risk and Vulnerability Profi le 2016 GOMBA DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE a Acknowledgment On behalf of Office of the Prime Minister, I wish to express my sincere appreciation to all of the key stakeholders who provided their valuable inputs and support to this Multi-Hazard, Risk and Vulnerability mapping exercise that led to the production of comprehensive district Hazard, Risk and Vulnerability (HRV) profiles. I extend my sincere thanks to the Department of Relief, Disaster Preparedness and Management, under the leadership of the Commissioner, Mr. Martin Owor, for the oversight and management of the entire exercise. The HRV assessment team was led by Ms. Ahimbisibwe Catherine, Senior Disaster Preparedness Officer supported by Mr. Ogwang Jimmy, Disaster Preparedness Officer and the team of consultants (GIS/DRR specialists); Dr. Bernard Barasa, and Mr. Nsiimire Peter, who provided technical support. Our gratitude goes to UNDP for providing funds to support the Hazard, Risk and Vulnerability Mapping. The team comprised of Mr. Steven Goldfinch – Disaster Risk Management Advisor, Mr. Gilbert Anguyo - Disaster Risk Reduction Analyst, and Mr. Ongom Alfred-Early Warning system Programmer. My appreciation also goes to Gomba District Team. The entire body of stakeholders who in one way or another yielded valuable ideas and time to support the completion of this exercise. Hon. Hilary O. Onek Minister for Relief, Disaster Preparedness and Refugees GOMBA DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE i EXECUTIVE SUMMARY The multi-hazard vulnerability profile outputs from this assessment for Gomba District was a combination of spatial modeling using adaptive, sensitivity and exposure spatial layers and information captured from District Key Informant interviews and sub-county FGDs using a participatory approach. -

Ending CHILD MARRIAGE and TEENAGE PREGNANCY in Uganda
ENDING CHILD MARRIAGE AND TEENAGE PREGNANCY IN UGANDA A FORMATIVE RESEARCH TO GUIDE THE IMPLEMENTATION OF THE NATIONAL STRATEGY ON ENDING CHILD MARRIAGE AND TEENAGE PREGNANCY IN UGANDA Final Report - December 2015 ENDING CHILD MARRIAGE AND TEENAGE PREGNANCY IN UGANDA 1 A FORMATIVE RESEARCH TO GUIDE THE IMPLEMENTATION OF THE NATIONAL STRATEGY ON ENDING CHILD MARRIAGE AND TEENAGE PREGNANCY IN UGANDA ENDING CHILD MARRIAGE AND TEENAGE PREGNANCY IN UGANDA A FORMATIVE RESEARCH TO GUIDE THE IMPLEMENTATION OF THE NATIONAL STRATEGY ON ENDING CHILD MARRIAGE AND TEENAGE PREGNANCY IN UGANDA Final Report - December 2015 ACKNOWLEDGEMENTS The United Nations Children Fund (UNICEF) gratefully acknowledges the valuable contribution of many individuals whose time, expertise and ideas made this research a success. Gratitude is extended to the Research Team Lead by Dr. Florence Kyoheirwe Muhanguzi with support from Prof. Grace Bantebya Kyomuhendo and all the Research Assistants for the 10 districts for their valuable support to the research process. Lastly, UNICEF would like to acknowledge the invaluable input of all the study respondents; women, men, girls and boys and the Key Informants at national and sub national level who provided insightful information without whom the study would not have been accomplished. I ENDING CHILD MARRIAGE AND TEENAGE PREGNANCY IN UGANDA A FORMATIVE RESEARCH TO GUIDE THE IMPLEMENTATION OF THE NATIONAL STRATEGY ON ENDING CHILD MARRIAGE AND TEENAGE PREGNANCY IN UGANDA CONTENTS ACKNOWLEDGEMENTS ..................................................................................I -

Instruction Notes for Compilation of BS100
INSTRUCTION NOTES FOR THE COMPILATION OF FORM BS100 FOR CREDIT INSTITUTIONS IN UGANDA FOR CREDIT INSTITUTIONS LICENSED UNDER THE FINANCIAL INSTITUTIONS ACT, 2004 (AS AMENDED) NOVEMEBER 2020 FOREWORD Institutions registered under the Financial Institutions Act (FIA), 2004 as amended and the Micro- Finance Deposit Taking Institutions (MDI) Act 2003 are required to report to the Central Bank data or information that the Bank may deem necessary for carrying out its responsibilities as spelt out in the two Acts. The Central Bank designs, and amends as necessary, forms/returns that are used to collect information from the institutions. The Form BS100 is one of the statutory returns designed by the Supervision and Research Functions of Bank of Uganda for all Credit Institutions in Uganda The BS100 collects information on financial and nonfinancial assets and liabilities broken down by detailed institutional sectors and in some instances, economic sectors and additional analytical information. The update of the BS100 is expected to capture subsequent changes in the sector as they unfold, while maintaining emphasis on having the reports manageable for the compilers and consistency across reporting institutions. In cases where further assistance or clarification is required in completing the BS100 form, one may contact telephone numbers 041-4258441, Ext. 3318 or 2175. Completed returns should be submitted through the official electronic mode of submission to: Bank of Uganda Supervision Directorate, Non-Bank Financial Institutions Department P. O. Box 7120, KAMPALA. Copy to: Bank of Uganda Research and Policy Directorate, Statistics Department P. O. Box 7120, KAMPALA. SUPERVISION DIRECTORATE BANK OF UGANDA NOVEMEBER 2020 2 TABLE OF CONTENTS FOREWORD ................................................................................................................ -

A Case Study of Kyazanga Sub County Lwengo District By
COMMUNITY PARTICIPATION AND SERVICE DELIVERY IN LOCAL GOVERNMENT: A CASE STUDY OF KYAZANGA SUB COUNTY LWENGO DISTRICT BY SSEMANDA ROBERT BPA/42695/141/DU A RESEARCH REPORT SUBMITTED TO THE COLLEGE OF HUMANITIES AND SOCIAL SCIENCES IN PARTIAL FULFILLMENT OF THE REQUIREMENT FOR THE AWARD OF BACHELOR OF PUBLIC ADMINISTRATION OF KAMPALA INTERNATIONAL UNIVERSITY MAY, 2017 DECLARATION I Ssemanda Robert declare that this is my original work and has never been presented to any other academic institution for any award Signature~ date..!~. SSEMANDA ROBERT APPROVAL This research report was done under my supervision as the university supervisor Signature ~ Date... .t~—t aS t ~c i } MISS AHEEBWA SANURA DEDICATION This piece of work is dedicated to my dear parents Mr. Kayitana Vincent (my father) and MS Mukakalera Patricia (my mother) III ACKNOWLEGEMENT The success of this study resides with the Almighty God without whose help, guidance and grace, I would not have fulfilled this academic ambition. Special thanks go to my parents Mr. Kayitana Vincent (my father), MS Mukakalera Patricia (my mother) and the Late Andrew Felix Kaweesi. I thank my supervisor Ms. Aheebwa Sanuuru who despite her busy schedule guided me to the end. It is a privilege and an honor to have accorded me her time and guidance and I am fortunate to have associated with you in this regard. I would also like to thank the members of my lecturers Mr. Muhwezi Ivan, Ms. Sauda, Mr. Achoda Denis, and Dr. Tom Mulegi. I would like to thank my course mates more especially Ngobi Swaibu for their cooperation and time during the course of study. -

Lwengo District Local Government Statistical Abstract 2018-2019
THE REPUBLIC OF UGANDA LWENGO DISTRICT LOCAL GOVERNMENT STATISTICAL ABSTRACT 2018-2019 Figure 1 Lwengo District Local Government P.O Box 1330, Masaka Tel: +256-0772454754 E-mail: [email protected] Website: www.lwengo.go.ug August 2019 ii | P a g e FOREWORD The importance of statistics in informing planning and monitoring of government programmes cannot be over emphasised. We need to know where we are, determine where we want to reach and also know whether we have reached there. The monitoring of socio-economic progress is not possible without measuring how we progress and establishing whether human, financial and other resources are being used efficiently. However, these statistics in many occasions have been National in outlook and less District specific. The development of a District-based Statistical Abstract shall go a long way to solve this gap and provide District tailored statistics and will reflect the peculiar nature of the District by looking at specific statistics which would not be possible to provide at a higher level. Data and statistics are required for designing, planning, implementing, monitoring and evaluating development programmes. For instance, statistics on school enrolment, completion rates and dropout rates etc. are vital in the monitoring of Universal Primary Education (UPE) and Universal Secondary Education (USE) programmes. Statistics are also needed for establishing grant aid to community schools, staff levels and other investments in the education programmes. The collection and use of statistics and performance indicators is critical for both the successful management and operation of the sectors, including Lower Local Governments. For data to inform planning and service delivery it should be effectively disseminated to the various users and stakeholders. -
Usaid's Malaria Action Program for Districts
USAID’S MALARIA ACTION PROGRAM FOR DISTRICTS GENDER ANALYSIS MAY 2017 Contract No.: AID-617-C-160001 June 2017 USAID’s Malaria Action Program for Districts Gender Analysis i USAID’S MALARIA ACTION PROGRAM FOR DISTRICTS Gender Analysis May 2017 Contract No.: AID-617-C-160001 Submitted to: United States Agency for International Development June 2017 USAID’s Malaria Action Program for Districts Gender Analysis ii DISCLAIMER The authors’ views expressed in this publication do not necessarily reflect the views of the United States Agency for International Development (USAID) or the United States Government. June 2017 USAID’s Malaria Action Program for Districts Gender Analysis iii Table of Contents ACRONYMS ...................................................................................................................................... VI EXECUTIVE SUMMARY ................................................................................................................... VIII 1. INTRODUCTION ...........................................................................................................................1 2. BACKGROUND ............................................................................................................................1 COUNTRY CONTEXT ...................................................................................................................3 USAID’S MALARIA ACTION PROGRAM FOR DISTRICTS .................................................................6 STUDY DESCRIPTION..................................................................................................................6 -

Perspectives from Urban and Rural Contexts in Uganda
UvA-DARE (Digital Academic Repository) The dilemmas and complexities of implementing language-in-education policies: perspectives from urban and rural contexts in Uganda Altinyelken, H.K.; Moorcroft, S.; van der Draai, H. DOI 10.1016/j.ijedudev.2013.11.001 Publication date 2014 Document Version Submitted manuscript Published in International Journal of Educational Development Link to publication Citation for published version (APA): Altinyelken, H. K., Moorcroft, S., & van der Draai, H. (2014). The dilemmas and complexities of implementing language-in-education policies: perspectives from urban and rural contexts in Uganda. International Journal of Educational Development, 36, 90-99. https://doi.org/10.1016/j.ijedudev.2013.11.001 General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE -

WHO UGANDA BULLETIN February 2016 Ehealth MONTHLY BULLETIN
WHO UGANDA BULLETIN February 2016 eHEALTH MONTHLY BULLETIN Welcome to this 1st issue of the eHealth Bulletin, a production 2015 of the WHO Country Office. Disease October November December This monthly bulletin is intended to bridge the gap between the Cholera existing weekly and quarterly bulletins; focus on a one or two disease/event that featured prominently in a given month; pro- Typhoid fever mote data utilization and information sharing. Malaria This issue focuses on cholera, typhoid and malaria during the Source: Health Facility Outpatient Monthly Reports, Month of December 2015. Completeness of monthly reporting DHIS2, MoH for December 2015 was above 90% across all the four regions. Typhoid fever Distribution of Typhoid Fever During the month of December 2015, typhoid cases were reported by nearly all districts. Central region reported the highest number, with Kampala, Wakiso, Mubende and Luweero contributing to the bulk of these numbers. In the north, high numbers were reported by Gulu, Arua and Koti- do. Cholera Outbreaks of cholera were also reported by several districts, across the country. 1 Visit our website www.whouganda.org and follow us on World Health Organization, Uganda @WHOUganda WHO UGANDA eHEALTH BULLETIN February 2016 Typhoid District Cholera Kisoro District 12 Fever Kitgum District 4 169 Abim District 43 Koboko District 26 Adjumani District 5 Kole District Agago District 26 85 Kotido District 347 Alebtong District 1 Kumi District 6 502 Amolatar District 58 Kween District 45 Amudat District 11 Kyankwanzi District -

Table of Contents List of Tables
TABLE OF CONTENTS 6 PROJECT IMPACTS ................................................................................................................ 138 Introduction ............................................................................................................................... 138 Summary of Impacts ................................................................................................................. 138 Impacts on Land ....................................................................................................................... 143 6.3.1 Land Requirements and Land Use Context ......................................................................... 143 Impacts on houses – Physical Displacement ........................................................................... 149 Impacts on other structures ...................................................................................................... 153 Impacts on Communal Buildings .............................................................................................. 159 Graves and Cultural Heritage Assets ....................................................................................... 160 Impacts on Crops and Economic Trees .................................................................................... 160 Impacts on Livelihood Activities – Economic Displacement ..................................................... 166 Impacts on Public Utilities/Infrastructure .................................................................................. -

Kalungu District
National Population and Housing Census 2014 Area Specific Profiles Kalungu District April 2017 National Population and Housing Census 2014 Area Specific Profiles – Kalungu District This report presents findings of National Population and Housing Census (NPHC) 2014 undertaken by the Uganda Bureau of Statistics (UBOS). Additional information about the Census may be obtained from the UBOS Head Office, Statistics House. Plot 9 Colville Street, P. O. Box 7186, Kampala, Uganda; Telephone: +256-414 706000 Fax: +256-414 237553; E-mail: [email protected]; Website: www.ubos.org Cover Photos: Uganda Bureau of Statistics Recommended Citation Uganda Bureau of Statistics 2017, The National Population and Housing Census 2014 – Area Specific Profile Series, Kampala, Uganda. National Population and Housing Census 2014 Area Specific Profiles – Kalungu District FOREWORD Demographic and socio-economic data are useful for planning and evidence-based decision making in any country. Such data are collected through Population Censuses, Demographic and Socio-economic Surveys, Civil Registration Systems and other Administrative sources. In Uganda, however, the Population and Housing Census remains the main source of demographic data, especially at the sub-national level. Population Census taking in Uganda dates back to 1911 and since then the country has undertaken five such Censuses. The most recent, the National Population and Housing Census 2014, was undertaken under the theme ‘Counting for Planning and Improved Service Delivery’. The enumeration for the 2014 Census was conducted in August/September 2014. The Uganda Bureau of Statistics (UBOS) worked closely with different Government Ministries, Departments and Agencies (MDAs) as well as Local Governments (LGs) to undertake the census exercise. -
Population by Parish
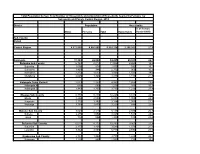
Total Population by Sex, Total Number of Households and proportion of Households headed by Females by Subcounty and Parish, Central Region, 2014 District Population Households % of Female Males Females Total Households Headed HHS Sub-County Parish Central Region 4,672,658 4,856,580 9,529,238 2,298,942 27.5 Kalangala 31,349 22,944 54,293 20,041 22.7 Bujumba Sub County 6,743 4,813 11,556 4,453 19.3 Bujumba 1,096 874 1,970 592 19.1 Bunyama 1,428 944 2,372 962 16.2 Bwendero 2,214 1,627 3,841 1,586 19.0 Mulabana 2,005 1,368 3,373 1,313 21.9 Kalangala Town Council 2,623 2,357 4,980 1,604 29.4 Kalangala A 680 590 1,270 385 35.8 Kalangala B 1,943 1,767 3,710 1,219 27.4 Mugoye Sub County 6,777 5,447 12,224 3,811 23.9 Bbeta 3,246 2,585 5,831 1,909 24.9 Kagulube 1,772 1,392 3,164 1,003 23.3 Kayunga 1,759 1,470 3,229 899 22.6 Bubeke Sub County 3,023 2,110 5,133 2,036 26.7 Bubeke 2,275 1,554 3,829 1,518 28.0 Jaana 748 556 1,304 518 23.0 Bufumira Sub County 6,019 4,273 10,292 3,967 22.8 Bufumira 2,177 1,404 3,581 1,373 21.4 Lulamba 3,842 2,869 6,711 2,594 23.5 Kyamuswa Sub County 2,733 1,998 4,731 1,820 20.3 Buwanga 1,226 865 2,091 770 19.5 Buzingo 1,507 1,133 2,640 1,050 20.9 Maziga Sub County 3,431 1,946 5,377 2,350 20.8 Buggala 2,190 1,228 3,418 1,484 21.4 Butulume 1,241 718 1,959 866 19.9 Kampala District 712,762 794,318 1,507,080 414,406 30.3 Central Division 37,435 37,733 75,168 23,142 32.7 Bukesa 4,326 4,711 9,037 2,809 37.0 Civic Centre 224 151 375 161 14.9 Industrial Area 383 262 645 259 13.9 Kagugube 2,983 3,246 6,229 2,608 42.7 Kamwokya -

FY 2020/21 Vote:600 Bukomansimbi District
LG Approved Workplan Vote:600 Bukomansimbi District FY 2020/21 Foreword We are pleased to present our Draft Performance Contract for the Financial year 2020.2021.This is in line with the relevant laws including the Constitution, Local Government Act, and the Public Finance and Management Act. Going forward we acknowledge the Contribution of the Ministries, Departments and agencies that have supported us since the birth of this District Local Government. Special thanks also go to Development Partners namely Korea Foundation for International Development for their enormous contribution to our Health sector in the Emergency and Obstetrics Care. Rakai School of Health Sciences for their Contribution towards mitigation of HIV/AIDS. GAVI, WHO, UNICEF, Dutch Council, and TASO; to you we say thank you. Towards the end of March,2020, the country and this District were caught unaware with the Deadly Corvid 19 Virus, the Floods that resulted from heavy rains, which destroyed peoples property. Although so far we have not yet registered a single positive case in the District, we should not tire to keep alert, continue with the surveillance, educate the massses (that are becoming adamant). Lastly let me thank the Executive, District Council and all the members of Staff for your tireless efforts in serving the people of Bukomansimbi District and the Country at large. For God and my Country. Masereka Amis Asuman (Mr) Generated on 11/06/2020 05:25 1 LG Approved Workplan Vote:600 Bukomansimbi District FY 2020/21 SECTION A: Workplans for HLG Workplan 1a