A Case Study on the Use of Athletic Performance Strategies in an Elite Athlete’S Management of Pancreatic Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Popular Repertoire (1960’S – Present Day)
! " Popular repertoire (1960’s – present day) 9 To 5 – Dolly Parton Billie Jean – Michael Jackson 500 Miles – The Proclaimers Bittersweet Symphony - The Verve Adventure Of A Lifetime - Coldplay Blackbird – The Beatles Agadoo – Black Lace Blowers Daughter – Damien Rice Ain’t No Mountain High Enough – Ashford/ Simpson Bohemian Rhapsody - Queen All About That Bass – Meghan Trainor Brown Eyed Girl – Van Morrison All About You - McFly Budapest – George Ezra All I Want Is You – U2 Build Me Up Buttercup – The Foundations All Of Me – John Legend Burn – Ellie Goulding All The Small Things – Blink 182 Can’t Help Falling In Love – Elvis Presley All You Need Is Love – The Beatles Can’t Stop The Feeling – Justin Timberlake Always a Woman – Billy Joel Can’t Take My Eyes Off You – Bob Crewe/Bob Gaudio Always On My Mind – Elvis Presley Chasing Cars – Snow Patrol Amazing (Just The Way You Are) – Bruno Mars Cheerleader - OMI Amazed - Lonestar Close To You - America – Razorlight Burt Bacharach Apologize – One Republic Come On Eileen – Dexy’s Midnight Runners At Last – Etta James Common People – Pulp Back for Good - Take That Copacabana – Barry Manilow Bad Romance – Lady Gaga Crazy In Love – Beyonce Beat It – Michael Jackson Crazy Little Thing Called Love - Queen Beautiful Day – U2 Dancing Queen - Abba Beautiful In White - Westlife Despacito – Justin Bieber/Luis Fonsi Ben – Michael Jackson Don’t Stop Believing - Journey Beneath Your Beautiful – Emeli Sande/ Labyrinth Don't Stop Me Now - Queen Best Day Of My Life – American Authors Don’t Stop Movin’ – S Club -

Rolling Stone Magazine's Top 500 Songs
Rolling Stone Magazine's Top 500 Songs No. Interpret Title Year of release 1. Bob Dylan Like a Rolling Stone 1961 2. The Rolling Stones Satisfaction 1965 3. John Lennon Imagine 1971 4. Marvin Gaye What’s Going on 1971 5. Aretha Franklin Respect 1967 6. The Beach Boys Good Vibrations 1966 7. Chuck Berry Johnny B. Goode 1958 8. The Beatles Hey Jude 1968 9. Nirvana Smells Like Teen Spirit 1991 10. Ray Charles What'd I Say (part 1&2) 1959 11. The Who My Generation 1965 12. Sam Cooke A Change is Gonna Come 1964 13. The Beatles Yesterday 1965 14. Bob Dylan Blowin' in the Wind 1963 15. The Clash London Calling 1980 16. The Beatles I Want zo Hold Your Hand 1963 17. Jimmy Hendrix Purple Haze 1967 18. Chuck Berry Maybellene 1955 19. Elvis Presley Hound Dog 1956 20. The Beatles Let It Be 1970 21. Bruce Springsteen Born to Run 1975 22. The Ronettes Be My Baby 1963 23. The Beatles In my Life 1965 24. The Impressions People Get Ready 1965 25. The Beach Boys God Only Knows 1966 26. The Beatles A day in a life 1967 27. Derek and the Dominos Layla 1970 28. Otis Redding Sitting on the Dock of the Bay 1968 29. The Beatles Help 1965 30. Johnny Cash I Walk the Line 1956 31. Led Zeppelin Stairway to Heaven 1971 32. The Rolling Stones Sympathy for the Devil 1968 33. Tina Turner River Deep - Mountain High 1966 34. The Righteous Brothers You've Lost that Lovin' Feelin' 1964 35. -

Chapter 1 COMMITMENT 第1
The Cyclist’s Training Bible (3rd edition) 自行车训练圣经(第三版) Chapter 1 COMMITMENT 第 1 章 承诺 Chapter 1 COMMITMENT 第 1 章 承诺 At the base of the climb, which was 12 kilometers 这是一段 12 公里长的上坡,在山脚下,我开始 long, I started to look around and saw Ullrich, 环顾四周并看到乌尔里希,潘塔尼,维廉切,里 Pantani, Virenque, Riis, Escartin, and Jimenez – all 斯,斯卡丁及希门尼斯 ―― 全都是总排名前 10 in the top 10 of the general classification – and then 位的高手 ―― 还有我。我没掉队!我是第一次 me. I was hanging, I was there with these guys for 跟这一帮人骑在一起。 the first time. -- BOBBY JULICH, commenting on the moment ――BOBBY JULICH,在 1997 年的环法赛中,当 in the 1997 Tour de France when he realized he 他意识到自己有机会争夺名次时的评论 was a contender Talk is cheap. It’s easy to have big dreams and 嘴巴说说是毫不费力的。在比赛前拥有一个 set high goals before the racing starts. But the 大梦及设定很高的目标也很简单。但是真正 true test of a commitment to better racing 对所承诺的更好比赛成绩的考验,不是靠 results is not in the talking, but in the doing. It 说,而是靠做。它并不是从这个赛季的第一 doesn’t start with the first race of the season – 场比赛开始 ―― 它是你现在所做的所有使 it’s all the things you do today to get stronger, faster, and more enduring. Real commitment 你变得更强壮,更快,耐力更好的所有事 means 365 days a year and 24 hours a day. 情。真正的承诺体现在一年 365 天和一天 24 小时。 Talk to the best riders you know, Ask 和你知道的最好的车手交谈,听听他们 them about commitment. Once you probe past 关于承诺的看法。 过滤掉那些“噢,什 all of the “aw, shucks” stuff, you’ll discover 么!”之类的废话后,你会发现骑自行车在 how big a role cycling plays in their lives. The 他们的生活中是扮演着多大的一个角色。他 better they are, the more you’ll hear about life 们越出色,你就会听到越多围绕运动的生活 revolving around the sport. -

Mobile Beat Top 200
Mobile Beat Top 200 Top 200 Most Requested Songs of the Past Year Rank Artist Song 1 Whitney Houston I Wanna Dance With Somebody (Who Loves Me) 2 Mark Ronson Feat. Bruno Mars Uptown Funk 3 Journey Don't Stop Believin' 4 Cupid Cupid Shuffle 5 Neil Diamond Sweet Caroline (Good Times Never Seemed So Good) 6 Walk The Moon Shut Up And Dance 7 Justin Timberlake Can't Stop The Feeling! 8 Earth, Wind & Fire September 9 Usher Feat. Ludacris & Lil' Jon Yeah 10 V.I.C. Wobble 11 DJ Casper Cha Cha Slide 12 Outkast Hey Ya! 13 Black Eyed Peas I Gotta Feeling 14 Bon Jovi Livin' On A Prayer 15 ABBA Dancing Queen 16 Bruno Mars 24k Magic 17 Garth Brooks Friends In Low Places 18 Spice Girls Wannabe 19 AC/DC You Shook Me All Night Long 20 Kenny Loggins Footloose 21 Backstreet Boys Everybody (Backstreet's Back) 22 Isley Brothers Shout 23 B-52's Love Shack 24 Van Morrison Brown Eyed Girl 25 Bruno Mars Marry You 26 Miley Cyrus Party In The U.S.A. 27 Taylor Swift Shake It Off 28 Luis Fonsi & Daddy Yankee Feat. Justin Bieber Despacito 29 Montell Jordan This Is How We Do It 30 Beatles Twist And Shout 31 Ed Sheeran Thinking Out Loud 32 Sir Mix-A-Lot Baby Got Back 33 Maroon 5 Sugar 34 Ed Sheeran Perfect 35 Def Leppard Pour Some Sugar On Me 36 Killers Mr. Brightside 37 Pharrell Williams Happy 38 Toto Africa 39 Chris Stapleton Tennessee Whiskey 40 Flo Rida Feat. -

Michael Jackson the Perform a N C
MICHAEL JACKSON 101 THE PERFORMANCES MICHAEL JACKSON 101 THE PERFORMANCES &E Andy Healy MICHAEL JACKSON 101 THE PERFORMANCES . Andy Healy 2016 Michael gave the world a wealth of music. Songs that would become a part of our collective sound track. Under the Creative Commons licence you are free to share, copy, distribute and transmit this work with the proviso that the work not be altered in any way, shape or form and that all And for that the 101 series is dedicated to Michael written works are credited to Andy Healy as author. This Creative Commons licence does not and all the musicians and producers who brought the music to life. extend to the copyrights held by the photographers and their respective works. This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. This special Performances supplement is also dedicated to the choreographers, dancers, directors and musicians who helped realise Michael’s vision. I do not claim any ownership of the photographs featured and all rights reside with the original copyright holders. Images are used under the Fair Use Act and do not intend to infringe on the copyright holders. By a fan for the fans. &E 101 hat makes a great performance? Is it one that delivers a wow factor? W One that stays with an audience long after the houselights have come on? One that stands the test of time? Is it one that signifies a time and place? A turning point in a career? Or simply one that never fails to give you goose bumps and leave you in awe? Michael Jackson was, without doubt, the consummate performer. -

Daum Law Office
. RECEIVED APR 11 Z005 DAUM LAW OFFICE LCWTED5773TES Sponsorship Agreement 102590-96-Z-0739 U.S. POSTAL SERVICE CYCLING TEAM Services Purchasing Room 4541 475 L'Enfant Plaza SW Washington DC 20260-6237 RESPONDENTS 4 the Company that the Contract Term will not be further extended, which notice shall be provided to the Company on or before such July 1. 5. Indemnification. The Company agrees to indemnify, defend and hold the Sponsor, its subsidiaries and the affiliates of each such entity, as well as each officer, agent, distributor, employee; attorney, dealer, consultant, representative, contractor, successor and assign of any of the above, harmless from and against any and all expenses, damages, ; claims, suits, losses, actions, judgments, liabilities and costs whatsoever .(including, without limitation, attorneys' fees) arising out of: (i) the Company's breach, misrepresentation or non-performance under this Agreement; and (ii) any claim or action for personal injury, death, bodily injury, property damage or otherwise, suffered by participants, patrons or others at the Company; other than as a result of the; Sponsor's actions or negligence. 6. Insurance. The Company agrees to carry full insurance coverage (including comprehensive general liability) for all activities reasonably connected with this Agreement naming the Sponsor as an additional insured. 7. Trademark. (a) The Sponsor hereby grants to the Company the right to use such . trademarks, trade names, service marks or logos.owned by the Sponsor in connection with the implementation of this Agreement, as may be agreed to •- in writing from time to time by Sponsor and the Company. The Company shall have no interest in or right to the use of such names, marks or logos, except for .any limited right of usage which the Sponsor may grant in writing pursuant to this Agreement. -

Take 2 Dance Band Current Song List
TAKE 2 DANCE BAND CURRENT PLAYLIST 24K MAGIC BRUNO MARS 25 OR 6 TO 4 CHICAGO AFRICA TOTO AIN’T IT FUN PARAMORE AIN’T NO MOUNTAIN HIGH ENOUGH GAYE & TERRELL AIN’T NO OTHER MAN CHRISTINA AGUILERA AIN’T NOBODY CHAKA KHAN AIN’T THAT A KICK IN THE HEAD DEAN MARTIN AMERICAN GIRL TOM PETTY ANOTHER ONE BITES THE DUST QUEEN ANY WAY YOU WANT IT JOURNEY ARE YOU GONNA BE MY GIRL JET AT LAST ETTA JAMES ATTENTION CHARLIE PLUTH BABY ONE MORE TIME BRITNEY SPEARS BACK IN LOVE AGAIN L.T.D. BEAT IT MICHAEL JACKSON BEST OF MY LOVE THE EMOTIONS BILLIE JEAN MICHAEL JACKSON BLACK CAT JANET JACKSON BLURRED LINES ROBIN THICKE BOOGIE OOGIE OOGIE TASTE OF HONEY BORDERLINE MADONNA BORN TO BE WILD STEPPENWOLF BROKENHEARTED KARMIN CAKE BY THE OCEAN DNCE CALIFORNIA GIRLS KATY PERRY CALIFORNIA LOVE 2PAC CALL ME MAYBE CARLY RAE JEPSEN CALLING BATON ROUGE GARTH BROOKS CAN’T STOP THIS FEELING JUSTIN TIMBERLAKE CAR WASH ROLLS ROYCE CELEBRITY SKIN HOLE CLOSER CHAINSMOKERS COME OUT & PLAY OFFSPRING CRAZY IN LOVE BEYONCE DA YA THINK I’M SEXY STEWART & DNCE DANCE TO THE MUSIC SLY/FAMILY STONE DER KOMMISSAR AFTER THE FIRE DIE YOUNG KE$HA DON’T PHUNK WITH MY HEART BLACKEYED PEAS DON’T STOP BELIEVING JOURNEY DREAMS FLEETWOOD MAC ESCAPADE JANET JACKSON EVERYBODY BACKSTREET BOYS EVERYBODY WANTS YOU BILLY SQUIRE FAITHFULLY FAME DAVID BOWIE FEEL FOR YOU CHAKA KHAN FEELS CALVIN HARRIS FINALLY CECE PENISTON FINESSE BRUNO MARS FORGET YOU CEE LO GREEN GAME OF LOVE SANTANA GENIE IN A BOTTLE CHRISTINA AUGILERA GET DOWN ON IT KOOL & THE GANG GET INTO THE GROOVE MADONNA GET LUCKY DAFT PUNK GIRLS JUST WANNA HAVE FUN CINDI LAUPER GOOD VIBRATIONS MARKY MARK GOT TO BE REAL CHERYL LYNN GROOVE LINE HEATWAVE H.O.L.Y. -

ARTIST SONG AC/DC Back in Black Adele Rolling in the Deep Al Green
ARTIST SONG AC/DC Back In Black Adele Rolling In The Deep Al Green Let’s Stay Together Alanis Morrisette Ironic Alien Ant Farm Smooth Criminal Amy Winehouse Valerie Aretha Franklin Respect Bill Withers Ain’t No Sunshine Bob Dylan Knocking on Heaven's door Bob Marley I Shot The Sherriff Bon Jovi You Give Love A Bad Name Britney Spears Toxic Bruno Mars Runaway Baby Bruno Mars Treasure Carly Rae Jepsen Call Me Maybe Cee Lo Green Forget You Chic Everybody Dance Chic Le Freak Chic Good Times Deep Purple Black Night Diana Ross Ain't No Mountain High Enough Electric Six Gay Bar Eric Clapton Cocaine Etta James I’d Rather Go Blind Etta James I Just Wanna Make Love to You Foo Fighters Times Like These Fountains Of Wayne Stacy's Mom Gloria Gaynor I Will Survive Gnarls Barkley Crazy Greenday American Idiot Jaco Pastorius The Chicken John Cage's 4'33 Justin Timberlake Sexy Back Led Zeppelin Good Times Bad Times Lee Ritenour Fly By Night Linkin Park Numb Luther Vandross Never Too Much Lynyrd Skynyrd Sweet Home Alabama Maroon 5 Harder To Breathe Maroon 5 This Love Marvin Gaye Through The Grape Vine Metallica Enter Sandman Michael Jackson Beat It Michael Jackson PYT Motorhead Ace of Spades Muse Starlight Muse Time is Running Out No Doubt Don’t Speak Olly Murs Troublemaker Otis Redding Sitting on the dock of the bay Paramore Misery business Paul Simon Diamonds on the Soles of Her Shoes Pixie Lott Cry Me Out Prince Kiss Rage Against The Machine Killing In The Name Red Hot Chili Peppers Aeroplane Red Hot Chili Peppers Californication Rose Royce Car Wash -

Skyline Orchestras
PRESENTS… SKYLINE Thank you for joining us at our showcase this evening. Tonight, you’ll be viewing the band Skyline, led by Ross Kash. Skyline has been performing successfully in the wedding industry for over 10 years. Their experience and professionalism will ensure a great party and a memorable occasion for you and your guests. In addition to the music you’ll be hearing tonight, we’ve supplied a song playlist for your convenience. The list is just a part of what the band has done at prior affairs. If you don’t see your favorite songs listed, please ask. Every concern and detail for your musical tastes will be held in the highest regard. Please inquire regarding the many options available. Skyline Members: • VOCALS AND MASTER OF CEREMONIES…………………………..…….…ROSS KASH • VOCALS……..……………………….……………………………….….BRIDGET SCHLEIER • VOCALS AND KEYBOARDS..………….…………………….……VINCENT FONTANETTA • GUITAR………………………………….………………………………..…….JOHN HERRITT • SAXOPHONE AND FLUTE……………………..…………..………………DAN GIACOMINI • DRUMS, PERCUSSION AND VOCALS……………………………….…JOEY ANDERSON • BASS GUITAR, VOCALS AND UKULELE………………….……….………TOM MCGUIRE • TRUMPET…….………………………………………………………LEE SCHAARSCHMIDT • TROMBONE……………………………………………………………………..TIM CASSERA • ALTO SAX AND CLARINET………………………………………..ANTHONY POMPPNION www.skylineorchestras.com (631) 277 – 7777 DANCE: 24K — BRUNO MARS A LITTLE PARTY NEVER KILLED NOBODY — FERGIE A SKY FULL OF STARS — COLD PLAY LONELY BOY — BLACK KEYS AIN’T IT FUN — PARAMORE LOVE AND MEMORIES — O.A.R. ALL ABOUT THAT BASS — MEGHAN TRAINOR LOVE ON TOP — BEYONCE BAD ROMANCE — LADY GAGA MANGO TREE — ZAC BROWN BAND BANG BANG — JESSIE J, ARIANA GRANDE & NIKKI MARRY YOU — BRUNO MARS MINAJ MOVES LIKE JAGGER — MAROON 5 BE MY FOREVER — CHRISTINA PERRI FT. ED SHEERAN MR. SAXOBEAT — ALEXANDRA STAN BEST DAY OF MY LIFE — AMERICAN AUTHORS NO EXCUSES — MEGHAN TRAINOR BETTER PLACE — RACHEL PLATTEN NOTHING HOLDING ME BACK — SHAWN MENDES BLOW — KE$HA ON THE FLOOR — J. -
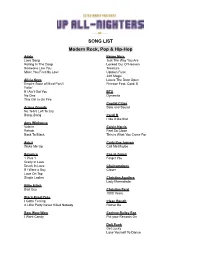
Band Song-List
SONG LIST Modern Rock, Pop & Hip-Hop Adele Bruno Mars Love Song Just The Way You Are Rolling In The Deep Locked Out Of Heaven Someone Like You Treasure Make You Feel My Love Uptown Funk 24K Magic Alicia Keys Leave The Door Open Empire State of Mind Part II Finesse Feat. Cardi B Fallin' If I Ain't Got You BTS No One Dynamite This Girl Is On Fire Capital Cities Ariana Grande Safe and Sound No Tears Left To Cry Bang, Bang Cardi B I like it like that Amy Winhouse Valerie Calvin Harris Rehab Feel So Close Back To Black This is What You Came For Avicii Carly Rae Jepsen Wake Me Up Call Me Maybe Beyonce Cee-lo Green 1 Plus 1 Forget You Crazy In Love Drunk In Love Chainsmokers If I Were a Boy Closer Love On Top Single Ladies Christina Aguilera Lady Marmalade Billie Eilish Bad Guy Christina Perri 1000 Years Black-Eyed Peas I Gotta Feeling Clean Bandit A Little Party Never Killed Nobody Rather Be Bow Wow Wow Corinne Bailey Rae I Want Candy Put your Records On Daft Punk Get Lucky Lose Yourself To Dance Justin Timberlake Darius Rucker Suit & Tie Wagon Wheel Can’t Stop The Feeling Cry Me A River David Guetta Love You Like I Love You Titanium Feat. Sia Sexy Back Drake Jay-Z and Alicia Keys Hotline Bling Empire State of Mind One Dance In My Feelings Jess Glynne Hold One We’re Going Home Hold My Hand Too Good Controlla Jessie J Bang, Bang DNCE Domino Cake By The Ocean Kygo Disclosure Higher Love Latch Katy Perry Dua Lipa Chained To the Rhythm Don’t Start Now California Gurls Levitating Firework Teenage Dream Duffy Mercy Lady Gaga Bad Romance Ed Sheeran Just Dance Shape Of You Poker Face Thinking Out loud Perfect Duet Feat. -

Quartet March2020
Pop/Contemporary (June 2020) A Dream Is A Wish Your Heart Makes - Cinderella A Million Dream Greatest Showman (2 versions) A River Flows in You-Yiruma A Sky Full of Stars - Coldplay A Thousand Miles - Vanessa Carlton A Thousand Years- Peri (2 versions) A Whole New World Accidentally In Love - Counting Crows Ain't No Sunshine - Bill Withers All About That Bass- Trainor (2 versions) All I Ask of You All I Need - RadioHead All I Want Is You - U2 All My Life - KC & Jojo All of Me- John Legend All of My love All of the Lights - Kayne West All The Small Things - Blink 182 Always - Bon Jovi America - Simon & Garfunkel Annie's Song - John Denver Another Day of Sun - La La Land Applause - Lady Gaga As Time Goes By At Last Autumn Leaves Away Into the Night - Joyce Hope Siskind Baba O'Reily - The Who Baby Love - The Supremes Baby One More Time - Britney Spears Back In Black - AC/DC Bad Romance - Lady Gaga Bad Touch - Bloodhound Gang Bailando - Enrique Bang Bang - Jessie J / Grande / Minaj Be MyBaby- Phil Spector Beat It - Michael Jackson Beautiful Day - U2 Beautiful in White - Westlife Be Our Guest- Beauty and Beast (2 versions) Beauty and the Beast Best Day of My Life Better Place - Rachel Platten Beyond the Sea Billie Jean - Michael Jackson Bittersweet Symphony Blank Space - Swift Bloom - The Paper Kites Blue Moon - Rodgers and Hart Bleeding Love - Leona Lewis Blurred Lines - Robin Thicke Bohemian Rapsody-Queen Book of Days - Enya Book of Love - Peter Gabriel Boom Clap - Charli XCX Brown Eyed Girl - Van Morrison Budapest - Geo Ezra Buddy Holly- -
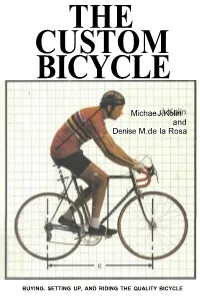
The Custom Bicycle
THE CUSTOM BICYCLE Michae J. Kolin and Denise M.de la Rosa BUYING. SETTING UP, AND RIDING THE QUALITY BICYCLE Copyright© 1979 by Michael J. Kolin and Denise M. de la Rosa All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopy, recording, or any information storage and retrieval system, without the written permission of the publisher. Book Design by T. A. Lepley Printed in the United States of America on recycled paper, containing a high percentage of de-inked fiber. 468 10 9753 hardcover 8 10 9 7 paperback Library of Congress Cataloging in Publication Data Kolin, Michael J The custom bicycle. Bibliography: p. Includes index. 1. Bicycles and tricycles—Design and construction. 2. Cycling. I. De la Rosa, Denise M., joint author. II. Title. TL410.K64 629.22'72 79-1451 ISBN 0-87857-254-6 hardcover ISBN 0-87857-255-4 paperback THE CUSTOM BICYCLE BUYING, SETTING UP, AND RIDING i THE QUALITY BICYCLE by Michael J. Kolin and Denise M. de la Rosa Rodale Press Emmaus, Pa. ARD K 14 Contents Acknowledgments Introduction Part I Understanding the Bicycle Frame CHAPTER 1: The Bicycle Frame 1 CHAPTER 2: Bicycle Tubing 22 CHAPTER 3: Tools for Frame Building 3 5 Part II British Frame Builders CHAPTER 4: Condor Cycles 47 CHAPTER 5: JRJ Cycles, Limited 53 CHAPTER 6: Mercian Cycles, Limited BO CHAPTER 7: Harry Quinn Cycles, Limited 67 CHAPTER 8: Jack Taylor Cycles 75 CHAPTER 9: TI Raleigh, Limited 84 CHAPTER 10: Woodrup Cycles 95 Part III French Frame Builders CHAPTER 11: CNC Cycles 103 CHAPTER 12: Cycles Gitane 106 CHAPTER 13: Cycles Peugeot 109 THE CUSTOM BICYCLE Part IV Italian Frame Builders CHAPTER 14: Cinelli Cino & C.