A Prospective, Longitudinal, Multicenter, Observational Study To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HIS in Thailand Never Ending Stories Thai Health Information System: of the Development of an Effective Situation and Challenges HIS in Thailand Dr
Never ending stories of the development of an effective HIS in Thailand Never ending stories Thai Health Information System: of the development of an effective Situation and challenges HIS in Thailand Dr. Pinij Faramnuayphal Supported by : Prince Mahidol Award Foundation under the Royal Patronage Ministry of Public Health World Health Organization The World Health Organization (WHO) identifies fully functional health Mahidol University information system as one of the six important building blocks of high Health Systems Research Institute performing health system. A well-functioning health information system (HIS) is one that ensures the production, analysis, dissemination and Published by: use of reliable and timely information on health determinants, health system performance and health status. All of these components Health Systems Research Institute (HSRI) contribute to a better health policy and planning, health resources allocation, health service delivery and finally, health outcome. With the cooperation of : The importance of health information system is crucial and is Ang Thong Provincial Health Office recognized that countries cannot build a good health system without Bangkok Hospital Group Medical Center it. Strengthening health information system, therefore, has become Bang Phae Hospital one of the most important issues worldwide in a recent decade. Bumrungrad Hospital Public Company Limited The demand on measuring the Millennium Development Goals is National Health Security office an example of the explicit requirements of -
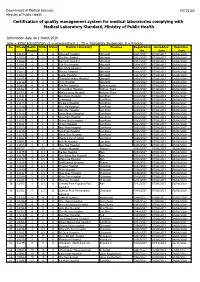
Certification of Quality Management System for Medical Laboratories Complying with Medical Laboratory Standard, Ministry of Public Health
Department of Medical Sciences F0715102 Ministry of Public Health Certification of quality management system for medical laboratories complying with Medical Laboratory Standard, Ministry of Public Health Information date on 1 March 2019 new = initial accreditation, r1 = reassessment 1 , TS = Temporary Suspension, P = Process No. HCode Health RMSc Status Medical Laboratory Province Registration Accredited Expiration Region No. Date Date 1 10673 2 2 r1 Uttaradit Hospital Uttaradit 0001/2557 07/08/2017 06/08/2020 2 11159 2 2 r1 Tha Pla Hospital Uttaradit 0002/2557 07/08/2017 06/08/2020 3 11160 2 2 r1 Nam Pat Hospital Uttaradit 0003/2557 07/08/2017 06/08/2020 4 11161 2 2 r1 Fak Tha Hospital Uttaradit 0004/2557 07/08/2017 06/08/2020 5 11162 2 2 r1 Ban Khok Hospital Uttaradit 0005/2557 07/08/2017 06/08/2020 6 11163 2 2 r1 Phichai Hospital Uttaradit 0006/2557 07/08/2017 06/08/2020 7 11164 2 2 r1 Laplae Hospital Uttaradit 0007/2557 07/08/2017 06/08/2020 8 11165 2 2 r1 ThongSaenKhan Hospital Uttaradit 0008/2557 07/08/2017 06/08/2020 9 11158 2 2 r1 Tron Hospital Uttaradit 0009/2557 07/08/2017 06/08/2020 10 10863 4 4 r1 Pak Phli Hospital Nakhonnayok 0010/2557 07/08/2017 06/08/2020 11 10762 4 4 r1 Thanyaburi Hospital Pathum Thani 0011/2557 07/08/2017 06/08/2020 12 10761 4 4 r1 Klong Luang Hospital Pathum Thani 0012/2557 07/08/2017 06/08/2020 13 11141 1 1 P Ban Hong Hospital LamPhun 0014/2557 07/08/2014 06/08/2017 14 11142 1 1 P Li Hospital LamPhun 0015/2557 07/08/2014 06/08/2017 15 11144 1 1 P Pa Sang Hospital LamPhun 0016/2557 07/08/2014 06/08/2017 -

Bangkok Anesthesia Regional Training Center
RoleRole ofof BARTCBARTC (Bangkok(Bangkok AnesthesiaAnesthesia RegionalRegional TrainingTraining Center)Center) IInn cooperationcooperation inin educationeducation andand trainingtraining inin developingdeveloping countriescountries ProfProf TharaThara TritrakarnTritrakarn DirectorDirector ofof BARTCBARTC 14th WCA, Cape Town, South Africa, 3/1/2008 Oslo Center, Norway, 12/1/2008 ShortageShortage ofof anesthesiologistsanesthesiologists AA worldwideworldwide problemsproblems MoreMore seriousserious inin developingdeveloping poorpoor countriescountries MarkedMarked variationvariation amongamong countriescountries EconomyEconomy - Most important determining factors - Three levels of wealth & health - Rich countries (per capita GNP > $ 10,000) - Medium to low (GNP $ 1,000-10,000) - Poor countries (GNP < $ 1,000) RichRich && MediumMedium countriescountries GNPGNP PeoplePeople NumberNumber PeoplePeople perper capitacapita perper ofof perper (US(US $)$) doctordoctor anesthetistsanesthetists anesthetistanesthetist USA 33,799 387 23,300 11,500 Japan 34,715 522 4,229 20,000 Singapore 22,710 667 150 26,600 Hong Kong 23,597 772 150 40,000 Australia 19,313 2170 10,000 Malaysia 3,248 1,477 250 88,000 Thailand 1,949 2,461 500 124,000 Philippines 1,048 1,016 1176 64,600 MediumMedium && PoorPoor CountriesCountries GNPGNP PeoplePeople NumberNumber PeoplePeople perper capitacapita perper ofof perper (US(US $)$) doctordoctor anesthetistsanesthetists anesthetistanesthetist Indonesia 617 6,7866,786 350 591,000591,000 Pakistan 492 2,0002,000 400 340,000340,000 -

Cover Tjs 35-4-57
ISSN 0125-6068 TheThai Journal of SURGERY Official Publication of the Royal College of Surgeons of Thailand www.surgeons.or.th/ejournal Volume 35 October-December 2014 Number 4 ORIGINAL ARTICLES 121 Comparison between Ventriculoatrial Shunt and Ventriculoperitoneal Shunt: Revision Rate and Complications Korrapakc Wangtanaphat, Porn Narischart 126 Open Surgical Management of Atherosclerotic Aortoiliac Occlusive Diseases (AIOD) Type 1 Anuwat Chantip 130 “Sawanpracharak” Connector: A Single Tube Intercostal Drainage Connector Wanchai Manakijsirisuthi 134 The Trainee’s Operative Experiences for General Surgery in Thailand Potchavit Aphinives CASE REPORT 139 Mitral and Tricuspid Valve Replacement in Uncommon Case of Situs Inversus with Dextrocardia Nuttapon Arayawudhikul, Boonsap Sakboon, Jareon Cheewinmethasiri, Angsu Chartirungsun, Benjamaporn Sripisuttrakul ABSTRACTS 143 Abstracts of the 39th Annual Scientific Congress of the Royal College of Surgeons of Thailand, 10-13 July 2014, Ambassador City Jomtien Hotel, Jomtien, Pattaya, Cholburi, Thailand (Part II) 169 Index Secretariat Office : Royal Golden Jubilee Building, 2 Soi Soonvijai, New Petchaburi Road, Huaykwang, Bangkok 10310, Thailand Tel. +66 2716 6141-3 Fax +66 2716 6144 E-mail: [email protected] www.surgeons.or.th The THAI Journal of SURGERY Official Publication of the Royal College of Surgeons of Thailand Vol. 35 October - December 2014 No. 4 Original Article Comparison between Ventriculoatrial Shunt and Ventriculoperitoneal Shunt: Revision Rate and Complications Korrapakc Wangtanaphat, MD Porn Narischart, MD Prasat Neurological Institute, Department of Medical Services, Ministry of Pubic Health, Bangkok, Thailand Abstract Background and Objective: Hydrocephalus is a common problem in neurosurgical field. In current clinical practice guidelines, ventriculoatrial shunt and ventriculoperitoneal shunt are recommended treatment options. No previous study reported differences between two procedures in term of complications and revision rates. -

Economic Burden of Hospitalization with Acute Wheezing in Preschool Children: a Multi-Center Study
Economic Burden of Hospitalization with Acute Wheezing in Preschool Children: A Multi-Center Study Paskorn Sritipsukho MD*,**, Khlongtip Matchimmadamrong MD***, Sasawan Chinratanapisit MD****, Jitladda Deerojanawong MD***** * Center of Excellence in Applied Epidemiology, Thammasat University, Pathumthani, Thailand ** Division of Allergy, Department of Pediatrics, Faculty of Medicine, Thammasat University, Pathumthani, Thailand *** Department of Pediatrics, Saraburi Hospital, Saraburi, Thailand **** Department of Pediatrics, Bhumibol Adulyadej Hospital, Bangkok, Thailand ***** Division of Respiratory disease and intensive care, Department of Pediatrics, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand Background: Wheezing is an important health problem in Thailand especially among preschool age. Objective: The aim of this study was to estimate costs of wheezing for hospitalization in preschool children under patient, provider, and societal perspectives. Material and Method: Two hundred and thirty-four participants who were admitted with acute wheezing at 4 hospitals including Thammasat University Hospital, Saraburi Hospital, Bhumibol Adulyadej Hospital and King Chulalongkorn Memorial Hospital during July 2014 to June 2015 were included in the present study. Data from hospital financial database and caregivers’ expenses were collected. Cost-to-charge ratio method was employed for valuation of direct medical costs. Informal care costs were determined by human capital approach. Results: The means of patient, provider and societal costs per admission were 3,020 THB (SD = 6,632 THB), 18,126 THB (SD = 16,898 THB), and 20,269 THB (SD = 20,537 THB) respectively. The main cost component in provider and societal perspective were accommodation costs during admission. Informal care cost was a major cost component for direct non- medical costs. The economic burden of acute wheezing admission of preschool children in Thailand was estimated as 759 million THB per year. -

September 2008 October 2008 R Dirty Pending Final 1 101 พระพุทธบาท
September 2008 October 2008 November 2008 No Site No. Hospital Name Record Status Total Cases Total Cases Total Cases Total Records r Dirty Pending Final 1 101 พระพุทธบาท สระบุรี Phraphuthabat Hospital 1129126 2 102 พญาไท ศรีราชา ชลบุรี Phyathai Sriracha Hospital 0116501 3 103 เวชศาสตรเขตรอน The Hospital for Tropical Medicine 0000000 4 104 ระยอง Rayong Hospital 155204016 5 105 รวมแพทยระยอง Ruampat Rayong 0000000 6 106 คลีนิคแพทยสุชาดา ระยอง Suchada Clinic 0000000 7 107 สงขลา Songkhla Hospital 0014202 8 108 สรรพสิทธิประสงค อุบลราชธานี Sapasittiprasong Hospital 10 21 30 120 19128 9 109 พระรามเกา Praram 9 Hospital 0000000 10 110 บําราศนราดูร นนทบุรี Bamrasnaradura Infectious Diseases Institute 0116132 11 111 ชลบุรี Chonburi Hospital 023120012 12 112 ธรรมศาสตรเฉลิมพระเกียรติ ปทุมธานี Thammasat University Hospital 0228017 13 113 เจาพระยา Chaophya Hospital 0000000 14 114 สงขลานครินทร สงขลา Songkhlanakarin Hospital 00416547 15 115 มูลนิธิโรคไต ณ โรงพยาบาลสงฆ The Kidney Foundation of Thailand 0000000 16 116 นพรัตนราชธานี Nopprat Rajathanee Hospital 036240717 17 117 พระจอมเกลา เพชรบุรี Phra Chom Klao Hospital Petburi 0000000 18 118 พระมงกุฎเกลา (กุมาร) Phramongkutklao Hospital, (Pediatrics) 0000000 19 119 สุราษฎรธานี Surat Thani Hospital 12 12 14 55 1054 20 120 รามาธิบดี Ramathibodi Hospital 0000000 21 121 วชิรพยาบาล Vajira Hospital 1112020 22 122 บานแพว สมุทรสาคร Banphaeo Hospital 1116501 23 123 สวรรคประชารักษ นครสวรรค Sawanpracharak Hospital 00312066 24 124 จุฬาลงกรณ Chulalongkorn Hospital 18 19 20 79 26 35 18 25 125 บํารุงราษฎร Bumrungrad International 0000000 26 126 ทักษิณ สุราษฎรธานี Thaksin Hospital 0000000 27 127 คายวิภาวดีรังสิต Fort Wiphavadirangsit Hospital 22215771 28 128 พระนครศรีอยุธยา Pranakornsriayudhaya Hospital 0000000 29 129 อุดรธานี Udonthani Hospital 19 22 28 112 26 57 29 30 130 ศรีนครินทร ม.ขอนแกน Srinakarin Hospital, Khon Kaen University 0000000 31 131 หนองคาย Nongkhai Hospital 0000000 32 132 ศิริราช Siriraj Hospital 1111010 Page 1 of 2 28 Jul 2008 September 2008 October 2008 November 2008 No Site No. -

A Randomized Controlled Trial Comparing Concurrent
J Gynecol Oncol. 2019 Jul;30(4):e82 https://doi.org/10.3802/jgo.2019.30.e82 pISSN 2005-0380·eISSN 2005-0399 Original Article A randomized controlled trial comparing concurrent chemoradiation versus concurrent chemoradiation followed by adjuvant chemotherapy in locally advanced cervical cancer patients: ACTLACC trial Siriwan Tangjitgamol ,1 Ekkasit Tharavichitkul ,2 Chokaew Tovanabutra ,3 Kanisa Rongsriyam ,4 Tussawan Asakij ,5 Kannika Paengchit ,6 Jirasak Sukhaboon ,7 Somkit Penpattanagul ,8 Apiradee Kridakara ,9 Received: Oct 28, 2018 Jitti Hanprasertpong ,10 Kittisak Chomprasert ,3 Sirentra Wanglikitkoon ,8 Revised: Mar 18, 2019 10 11 4 Accepted: Mar 18, 2019 Thiti Atjimakul , Piyawan Pariyawateekul , Kanyarat Katanyoo , Prapai Tanprasert ,12 Wanwipa Janweerachai,13 Duangjai Sangthawan ,14 Correspondence to Jakkapan Khunnarong ,1 Taywin Chottetanaprasith ,15 Siriwan Tangjitgamol Busaba Supawattanabodee ,16 Prasert Lertsanguansinchai ,17 Department of Obstetrics and Gynecology, Jatupol Srisomboon ,18 Wanrudee Isaranuwatchai ,19,20 Vichan Lorvidhaya 3 Faculty of Medicine Vajira Hospital, Navamindradhiraj University, 681 Samsen 1Department of Obstetrics and Gynecology, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, Road, Khet Dusit, Bangkok 10300, Thailand. Bangkok, Thailand E-mail: [email protected] 2Department of Radiology, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand [email protected] 3Radiation Oncology Section, Chonburi Cancer Hospital, Chonburi, Thailand 4Department of Radiology, Faculty -

TISCO Bank Public Company Limited Annual Report 2012
TISCO Bank Public Company Limited Annual Report 2012 Table of Contents Page Report from the Board of Directors A-1 Part 1 The Company 1. General Information 1-1 2. Risk Factors 2-1 3. Overview of TISCO Business 3-1 4. Business Operations by Area 4-1 5. Operating Assets 5-1 6. Legal Disputes 6-1 7. Capital Structure 7-1 8. Management 8-1 9. Internal Controls 9-1 10. Related Party Transactions 10-1 11. Financial Status and Performance 11-1 12. Other Related Information 12-1 Part 2 Attachment Attachment 1 Details of Directors, Management and Controlling Persons A 1-1 Attachment 2 Changes in TISCO Bank Shareholdings by Directors and Management A 2-1 Attachment 3 Report of the Audit Committee A 3-1 Attachment 4 Evaluation of the Sufficiency of Internal Control System A 4-1 Attachment 5 Statement of the Board of Directors’ Responsibility for Financial Statements A 5-1 and Auditor’s Report and Financial Statements Report from the Board of Directors In year 2012, Thai economy recovered from the aftermath of flood crisis to solid economic expansion driven by domestic consumption, following the accommodative fiscal and monetary policy, with high level of resiliency to external uncertainty. Strong economy coupled with the government stimulus programs helped to spur nationwide spending as evidenced by strong growth in private consumption and investment. Meanwhile, the Bank of Thailand eased monetary stance by lowering the policy rates to cushion against potential deterioration in export-related sectors amidst the fragile global economy. Capital market has been particularly benefited from these fundamentals as seen in the benchmark SET index rose by 36%, the best performing in Asia, whereas Bank’s credit growth has enjoyed another strong year with a growth rate of as high as 14%. -

Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveilla
applyparastyle “fig//caption/p[1]” parastyle “FigCapt” View metadata, citation and similar papers at core.ac.uk brought to you by CORE Open Forum Infectious Diseases provided by Apollo MAJOR ARTICLE Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveillance System Viriya Hantrakun,1, Somkid Kongyu,2 Preeyarach Klaytong,1 Sittikorn Rongsumlee,1 Nicholas P. J. Day,1,3 Sharon J. Peacock,4 Soawapak Hinjoy,2,5 and Direk Limmathurotsakul1,3,6, 1Mahidol-Oxford Tropical Medicine Research Unit (MORU), Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand, 2 Epidemiology Division, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, 3 Centre for Tropical Medicine and Global Health, Nuffield Department of Clinical Medicine, Old Road Campus, University of Oxford, Oxford, United Kingdom, 4 Department of Medicine, University of Cambridge, Cambridge, United Kingdom, 5 Office of International Cooperation, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, and 6 Department of Tropical Hygiene, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand Background. National notifiable diseases surveillance system (NNDSS) data in developing countries are usually incomplete, yet the total number of fatal cases reported is commonly used in national priority-setting. Melioidosis, an infectious disease caused by Burkholderia pseudomallei, is largely underrecognized by policy-makers due to the underreporting of fatal cases via the NNDSS. Methods. Collaborating with the Epidemiology Division (ED), Ministry of Public Health (MoPH), we conducted a retrospec- tive study to determine the incidence and mortality of melioidosis cases already identified by clinical microbiology laboratories nationwide. A case of melioidosis was defined as a patient with any clinical specimen culture positive for B. -

Saturday 5 September 2015
SATURDAY 5 SEPTEMBER 2015 SATURDAY 5 SEPTEMBER Registration Desk 0745-1730 Registration Desk, SECC for Pre-conference Workshop and Course Participants Location: Hall 4, SECC Group Meeting 1000-1700 AMEE Executive Committee Meeting (Closed Meeting) Location: Green Room 10, Back of Hall 4 AMEE-Essential Skills in Medical Education (ESME) Courses Pre-registration is essential and lunch will be provided. 0830-1700 ESME – Essential Skills in Medical Education Location: Argyll I, Crowne Plaza 0845-1630 ESMEA – Essential Skills in Medical Education Assessment Location: Argyll III, Crowne Plaza 0845-1630 RESME – Research Essential Skills in Medical Education Location: Argyll II, Crowne Plaza 0845-1700 ESMESim - Essential Skills in Simulation-based Healthcare Instruction Location: Castle II, Crowne Plaza 0900-1700 ESCEPD – Essential Skills in Continuing Education and Professional Development Location: Castle 1, Crowne Plaza 1000-1330 ESCEL – Essential Skills in Computer-Enhanced Learning Location: Carron 2, SECC Course Pre-registration is essential and lunch will be provided. 0830-1630 ASME-FLAME - Fundamentals of Leadership and Management in Education Location: Castle III, Crowne Plaza Masterclass Pre-registration is essential and lunch will be provided. 0915-1630 MC1 Communication Matters: Demystifying simulation design, debriefing and facilitation practice Kerry Knickle (Standardized Patient Program, Faculty of Medicine, University of Toronto, Canada); Nancy McNaughton, Diana Tabak) University of Toronto, Centre for Research in Education, Standardized -

Introduction
Introduction This report, Situation of the Thai Elderly 2019, is a production of the National Commission on Older Persons which has the responsibility to issue this report in accordance with Article 9(10) of the Elderly Act of 2003, and present the findings to the Cabinet each year. Ever since 2006, the National Commission on Older Persons has assigned the Foundation of Thai Gerontology Research and Development Institute (TGRI) to implement this assignment. This edition compiles data and information on older Thai persons for the year 2019, and explores trends in changes of the age structure of the population in the past in order to project the situation of older persons in the future. Each edition of the annual report on the Situation of the Thai Elderly has a particular focus or theme. For example, the 2013 edition focused on income security of older persons, the 2014 issue emphasized the vulnerability of older persons in the event of natural disasters, the 2015 focused on living arrangements of older persons, the 2016 edition focused on the health of the Thai elderly, the 2017 edition explored the concept of active aging in the Thai context of older persons, while the 2018 edition examined Thai elderly and employment. For the current edition (2019), the focus is on the social welfare of the elderly. In one sense, ‘Social Welfare’ sounds like a distant dream or ideal for Thai society, especially given the threat of the country’s being caught in the “middle-income trap.” However, if one considers examples of past policy, whether it is education or public health, Thailand should be able to create a system that covers the priority target groups, reduces the burden, and creates opportunities for people to have a good quality of life. -

314 Provider List (For Client)@01-09-57
Bangkok tel. fax web B Care Medical Center 29 Moo 6 Phaholyothin Rd., Saimai 0-2523-3359-71 www.bcaremedicalcenter.com OPD&IPD BNH Hospital (Bangkok Nursing Home) 9 Convent Rd, Silom Bangrak , Bangkok 0-2686-2700 www.bnhhospital.com OPD&IPD Bangkok Hospital 2 Soi Soonvijai 7, New Petchburi Rd, Huaykwang , Bangkok 0-2310-3000 www.bangkokhospital.com IPD ONLY Bangkok Hospital (Heart Center) 2 Soi Soonvijai 7, New Petchburi Rd, Huaykwang , Bangkok 0-2310-3000 www.bangkokhearthospital.com IPD ONLY Bangkok Christian Hostital 124 Silom Rd., Suriyavong , Bangrak , Bangkok 0-2625-9000 www.bkkchristianhosp.th.com OPD&IPD Bangna 1 Hospital 1302 Bangna-Trad 3rd KM Rd., Bangna, Bangna, Bangkok 10260 02- 746 8630-9 02-398-9531 www.bangna.co.th OPD&IPD Bangmod Hospital 747 Rama 2 Rd., Bangmod , Jomthong, Bangkok 10150 0-2867-0606,0-2416-0049 www.bangmodhos.com OPD&IPD Bangpai Hospital 58/2 Phetkasem Rd, Pak-Klong , Phasicharoen , Bangkok 0-2457-9740, 0-2865-7948 _ OPD&IPD Bangpakok 1 Hospital 2 Soi Suksawad 25/1 Suksawad Rd., Bangpakok Ratboorana 0-2872-1111 www.bangpakokhospital.com/ OPD&IPD Bangpakok 2 Hospital 372-372/1 Eakkachai Rd., Bangbon, Bangbon, Bangkok 10150 02-899-0130-9 02-451-0357 _ OPD&IPD Bangpakok 8 Hospital 115/524 Moo. 4 Akekachai Road, Bangbon, Bangkok 10150 0-2894-4111 www.bangpakokhospital.com OPD&IPD Bangpakok 9 Hospital 362 M.4 Rama 2 Bangmod Chomthong 0-2877-1111 www.bangpakokhospital.com/ OPD&IPD Bangkok Health Clinic 2/42-43 Nusasiri Building,2nd floor Unit204-205 Soi Sukhumit 42, Sukhumvit Road ,Prakhanong,Khlongtoey02-712-0335-7,Bangkok