Categories of Mental Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
SOMATIC SYMPTOM, BODILY DISTRESS and RELATED DISORDERS in CHILDREN and ADOLESCENTS 2019 Edition
IACAPAP Textbook of Child and Adolescent Mental Health Chapter CHILD PSYCHIATRY & PEDIATRICS I.1 SOMATIC SYMPTOM, BODILY DISTRESS AND RELATED DISORDERS IN CHILDREN AND ADOLESCENTS 2019 edition Olivia Fiertag, Sharon Taylor, Amina Tareen & Elena Garralda Olivia Fiertag MBChB, MRCPsych, PGDip CBT Consultant Child and Adolescent Psychiatrist. Honorary Clinical Researcher, HPFT NHS Trust & collaboration with Imperial College London, UK Conflict of interest: none declared Sharon Taylor BSc, MBBS, MRCP, MRCPsych, CASLAT, PGDip Consultant Child and Adolescent Psychiatrist CNWL Foundation NHS Trust & Honorary Senior Clinical Lecturer Imperial College London, UK. Joint Program Director, St Mary’s Child Sick Girl. Psychiatry Training Scheme Christian Krogh, Conflict of interest: none (1880/1881) National declared Gallery of Norway This publication is intended for professionals training or practicing in mental health and not for the general public. The opinions expressed are those of the authors and do not necessarily represent the views of the Editor or IACAPAP. This publication seeks to describe the best treatments and practices based on the scientific evidence available at the time of writing as evaluated by the authors and may change as a result of new research. Readers need to apply this knowledge to patients in accordance with the guidelines and laws of their country of practice. Some medications may not be available in some countries and readers should consult the specific drug information since not all dosages and unwanted effects are mentioned. Organizations, publications and websites are cited or linked to illustrate issues or as a source of further information. This does not mean that authors, the Editor or IACAPAP endorse their content or recommendations, which should be critically assessed by the reader. -

FROM MELANCHOLIA to DEPRESSION a HISTORY of DIAGNOSIS and TREATMENT Thomas A
1 FROM MELANCHOLIA TO DEPRESSION A HISTORY OF DIAGNOSIS AND TREATMENT Thomas A. Ban International Network for the History of Neuropsychopharmacology 2014 2 From Melancholia to Depression A History of Diagnosis and Treatment1 TABLE OF CONTENTS Introduction 2 Diagnosis and classifications of melancholia and depression 7 From Galen to Robert Burton 7 From Boissier de Sauvages to Karl Kahlbaum 8 From Emil Kraepelin to Karl Leonhard 12 From Adolf Meyer to the DSM-IV 17 Treatment of melancholia and depression 20 From opium to chlorpromazine 21 Monoamine Oxidase Inhibitors 22 Monoamine Re-uptake Inhibitors 24 Antidepressants in clinical use 26 Clinical psychopharmacology of antidepressants 30 Composite Diagnostic Evaluation of Depressive Disorders 32 The CODE System 32 CODE –DD 33 Genetics, neuropsychopharmacology and CODE-DD 36 Conclusions 37 References 37 INTRODUCTION Descriptions of what we now call melancholia or depression can be found in many ancient documents including The Old Testament, The Book of Job, and Homer's Iliad, but there is virtually 1 The text of this E-Book was prepared in 2002 for a presentation in Mexico City. The manuscript was not updated. 3 no reliable information on the frequency of “melancholia” until the mid-20th century (Kaplan and Saddock 1988). Between 1938 and 1955 several reports indicated that the prevalence of depression in the general population was below 1%. Comparing these figures, as shown in table 1, with figures in the 1960s and ‘70s reveals that even the lowest figures in the psychopharmacological era (from the 1960s) are 7 to 10 times greater than the highest figures before the introduction of antidepressant drugs (Silverman 1968). -

Somatoform Disorders – September 2017
CrackCast Show Notes – Somatoform Disorders – September 2017 www.canadiem.org/crackcast Chapter 103 – Somatoform disorders Episode overview 1. List 5 somatic symptom and related disorders 2. List 5 common presentations of conversion disorders 3. List 6 ddx of somatic symptom disorder Wisecracks 1. List 6 organic diseases that may be mistaken for somatoform disorders 2. Describe the treatment goals of somatoform disorders Somatoform disorders as a diagnosis has been eliminated from the DSM-5! The patient with functional neurological symptom disorder, what was termed conversion disorder previously, requires a careful and complete neurological examination. Rather than miss the subtle presentation of a neurological disorder, it may be appropriate to perform imaging and obtain neurological and psychiatric consultation. Do not assume that the patient with neurological deficits has a psychiatric disorder. Success with the SSD patient depends on establishing rapport with the patient and legitimizing their complaints to avoid a dysfunctional physician-patient interaction. • Avoid telling the SSD patient “it is all in your head” or “there is nothing wrong with you.” These patients are very sensitive to the idea that their suffering is being dismissed. • A useful approach is to discuss recent stressors with the patient and suggest to them that at times our bodies can be smarter than we are, telling us with physical symptoms that we need assistance. This approach alone may transform the ED visit from a standoff between physician and patient, to a grateful patient who develops greater insight and is amenable to referral. • Avoid prescribing unnecessary or addictive medications to the SSD patient. • If you suspect a diagnosis of SSD, refer the patient to primary care or psychiatry for further evaluation and treatment. -

Psychopathology and Somatic Complaints: a Cross-Sectional Study with Portuguese Adults
healthcare Article Psychopathology and Somatic Complaints: A Cross-Sectional Study with Portuguese Adults Joana Proença Becker 1,*, Rui Paixão 1 and Manuel João Quartilho 2 1 Faculty of Psychology and Education Sciences, University of Coimbra, 3000-115 Coimbra, Portugal; [email protected] 2 Faculty of Medicine, University of Coimbra, 3000-548 Coimbra, Portugal; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +351-910741887 Abstract: (1) Background: Functional somatic symptoms (FSS) are physical symptoms that cannot be fully explained by medical diagnosis, injuries, and medication intake. More than the presence of unexplained symptoms, this condition is associated with functional disabilities, psychological distress, increased use of health services, and it has been linked to depressive and anxiety disorders. Recognizing the difficulty of diagnosing individuals with FSS and the impact on public health systems, this study aimed to verify the concomitant incidence of psychopathological symptoms and FSS in Portugal. (2) Methods: For this purpose, 93 psychosomatic outpatients (91.4% women with a mean age of 53.9 years old) and 101 subjects from the general population (74.3% women with 37.8 years old) were evaluated. The survey questionnaire included the 15-item Patient Health Questionnaire, the 20-Item Short Form Survey, the Brief Symptom Inventory, the Depression, Anxiety and Stress Scale, and questions on sociodemographic and clinical characteristics. (3) Results: Increases in FSS severity were correlated with higher rates of depression, anxiety, and stress symptoms. The findings also suggest that increased rates of FSS are associated with lower educational level and Citation: Becker, J.P.; Paixão, R.; female gender. -

Bipolar Disorder - Accessscience from Mcgraw-Hill Education
Bipolar disorder - AccessScience from McGraw-Hill Education http://accessscience.com/content/900194 (http://accessscience.com/) Article by: Grunze, Heinz School of Neurology, Neurobiology, and Psychiatry, Newcastle University, Newcastle, United Kingdom. Publication year: 2016 DOI: http://dx.doi.org/10.1036/1097-8542.900194 (http://dx.doi.org/10.1036/1097-8542.900194) Content Course of bipolar disorder What is the neurobiology behind bipolar Bibliography How frequent is bipolar disorder? disorder? Additional Readings Treatment of bipolar disorder A major mental disorder in which there are life-long episodes of both mania and depression; also known as manic-depressive illness. The first recognizable descriptions of mania and depression date back to the writings of Aretaeus of Cappadocia (a Greek physician who lived around 150–200 CE). The modern history of bipolar disorder begins in the mid-nineteenth century with the concept of folie circulaire (“circular insanity”), proposed by the French psychiatrist Jean-Pierre Falret. Later, around the beginning of the twentieth century, it was defined by the work of the German psychiatrist Emil Kraepelin. See also: Affective disorders (/content/affective-disorders/013750) Bipolar disorder is characterized by sudden and often unexplained mood swings, ranging from delirious mania to severe depression. These mood changes are regularly accompanied by other mental and behavioral symptoms, such as fluctuations of volition, activity level, and cognitive functioning. Symptomatic criteria for bipolar disorder have been conceptualized in diagnostic manuals [the two most important being the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) by the American Psychiatric Association and the International Classification of Diseases (ICD-10) by the World Health Organization], with only minor differences between these manuals. -

Bipolar Disorders 100 Years After Manic-Depressive Insanity
Bipolar Disorders 100 years after manic-depressive insanity Edited by Andreas Marneros Martin-Luther-University Halle-Wittenberg, Halle, Germany and Jules Angst University Zürich, Zürich, Switzerland KLUWER ACADEMIC PUBLISHERS NEW YORK, BOSTON, DORDRECHT, LONDON, MOSCOW eBook ISBN: 0-306-47521-9 Print ISBN: 0-7923-6588-7 ©2002 Kluwer Academic Publishers New York, Boston, Dordrecht, London, Moscow Print ©2000 Kluwer Academic Publishers Dordrecht All rights reserved No part of this eBook may be reproduced or transmitted in any form or by any means, electronic, mechanical, recording, or otherwise, without written consent from the Publisher Created in the United States of America Visit Kluwer Online at: http://kluweronline.com and Kluwer's eBookstore at: http://ebooks.kluweronline.com Contents List of contributors ix Acknowledgements xiii Preface xv 1 Bipolar disorders: roots and evolution Andreas Marneros and Jules Angst 1 2 The soft bipolar spectrum: footnotes to Kraepelin on the interface of hypomania, temperament and depression Hagop S. Akiskal and Olavo Pinto 37 3 The mixed bipolar disorders Susan L. McElroy, Marlene P. Freeman and Hagop S. Akiskal 63 4 Rapid-cycling bipolar disorder Joseph R. Calabrese, Daniel J. Rapport, Robert L. Findling, Melvin D. Shelton and Susan E. Kimmel 89 5 Bipolar schizoaffective disorders Andreas Marneros, Arno Deister and Anke Rohde 111 6 Bipolar disorders during pregnancy, post partum and in menopause Anke Rohde and Andreas Marneros 127 7 Adolescent-onset bipolar illness Stan Kutcher 139 8 Bipolar disorder in old age Kenneth I. Shulman and Nathan Herrmann 153 9 Temperament and personality types in bipolar patients: a historical review Jules Angst 175 viii Contents 10 Interactional styles in bipolar disorder Christoph Mundt, Klaus T. -

Days out of Role and Somatic, Anxious-Depressive, Hypo-Manic, and Psychotic-Like Symptom Dimensions in a Community Sample of Young Adults Jacob J
Crouse et al. Translational Psychiatry (2021) 11:285 https://doi.org/10.1038/s41398-021-01390-y Translational Psychiatry ARTICLE Open Access Days out of role and somatic, anxious-depressive, hypo-manic, and psychotic-like symptom dimensions in a community sample of young adults Jacob J. Crouse 1, Nicholas Ho 1,JanScott 1,2,3,4, Nicholas G. Martin 5, Baptiste Couvy-Duchesne 5,6,7, Daniel F. Hermens 8,RichardParker 5, Nathan A. Gillespie 9, Sarah E. Medland 5 and Ian B. Hickie 1 Abstract Improving our understanding of the causes of functional impairment in young people is a major global challenge. Here, we investigated the relationships between self-reported days out of role and the total quantity and different patterns of self-reported somatic, anxious-depressive, psychotic-like, and hypomanic symptoms in a community-based cohort of young adults. We examined self-ratings of 23 symptoms ranging across the four dimensions and days out of role in >1900 young adult twins and non-twin siblings participating in the “19Up” wave of the Brisbane Longitudinal Twin Study. Adjusted prevalence ratios (APR) and 95% confidence intervals (95% CI) quantified associations between impairment and different symptom patterns. Three individual symptoms showed significant associations with days out of role, with the largest association for impaired concentration. When impairment was assessed according to each symptom dimension, there was a clear stepwise relationship between the total number of somatic symptoms and the 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; likelihood of impairment, while individuals reporting ≥4 anxious-depressive symptoms or five hypomanic symptoms had greater likelihood of reporting days out of role. -

A4-Depression Disease Fact Sheet
Depression Fact Sheet What is Depression? Major depressive disorder (simply known as clinical depression or just depression) is a mental disorder that causes a persistent feeling of sadness and loss of interest¹. Depression is characterized by extended peCommonriods of low mo osymptd. It can lomsead to ainclude: variety of emotional and physical problems and can negatively affect a person's personal life as well as sleeping, eating habits, and general health decrease a person’s ability to function at work and at home. Key facts Depression is a common illness worldwide, with more than 264 million people affected². Major depression is one of the most common mental disorders with a 1-year prevalence of 7.1% with 2/3 having severe functional impairment but with only 1/3 seeking help³. Major depression reduces life expectancy by about 10 years. History The term depression derives from the Latin verb deprimere ("to press down"). The Greek physician Hippocrates årat described a syndrome of melancholia (“black bile”) characterized by all "fears and despondencies, if they last a long time"⁴. Depression became a synonym of melancholia by the end of the 19th century, probably thanks to the German psychiatrist Emil Kraepelin who was the årst to use it as a global term. The denomination “Major depressive disorder” was introduced the mid-1970s and was incorporated into the Diagnostic and Statistical Manual of Mental Disorders (DSM)-III in 1980. Symptoms Not everyone who is depressed experiences every symptom of depression. In many cases, depression symptoms are severe enough to cause problems in daily activities, such as work, school, social activities or relationships. -

Melancholia and Mania: the Historical Contributions of Aretaeus of Cappadocia and Emil Kraepelin
University of Calgary PRISM: University of Calgary's Digital Repository Graduate Studies The Vault: Electronic Theses and Dissertations 2020-04-27 Melancholia and Mania: The Historical Contributions of Aretaeus of Cappadocia and Emil Kraepelin Marlier, Krystal Marlier, K. (2020). Melancholia and Mania: The Historical Contributions of Aretaeus of Cappadocia and Emil Kraepelin ( Unpublished master's thesis). University of Calgary, Calgary, AB. http://hdl.handle.net/1880/111923 master thesis University of Calgary graduate students retain copyright ownership and moral rights for their thesis. You may use this material in any way that is permitted by the Copyright Act or through licensing that has been assigned to the document. For uses that are not allowable under copyright legislation or licensing, you are required to seek permission. Downloaded from PRISM: https://prism.ucalgary.ca UNIVERSITY OF CALGARY Melancholia and Mania: The Historical Contributions of Aretaeus of Cappadocia and Emil Kraepelin by Krystal Marlier A THESIS SUBMITTED TO THE FACULTY OF GRADUATE STUDIES IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF ARTS GRADUATE PROGRAM IN GREEK AND ROMAN STUDIES CALGARY, ALBERTA APRIL, 2020 © Krystal Marlier 2020 Abstract Two millennia ago, Aretaeus of Cappadocia, a physician from the first to second century CE, first presented a modern portrayal of the relationship between μανίη (mania) and μελαγχολίη (melancholia). His understanding is reflective of the nineteenth-century German clinician, Emil Kraepelin. I propose that Kraepelin and Aretaeus possess more similarities than differences. They were homologous in research techniques and nosology, with one significant difference in aetiology. Presently, Aretaeus’ classification remains recognized in psychiatry, though with a slight deviation in understanding and under different psychiatric labels. -

Affective Disorders
Psychiatr. Pol. 2020; 54(4): 641–659 PL ISSN 0033-2674 (PRINT), ISSN 2391-5854 (ONLINE) www.psychiatriapolska.pl DOI: https://doi.org/10.12740/PP/123167 A half-century of participant observation in psychiatry. Part II: Affective disorders Janusz Rybakowski Poznan University of Medical Sciences, Department of Adult Psychiatry and Department of Psychiatric Nursing Summary The last half-century, thanks to the efforts of outstanding researchers, brought about great progress in the pathogenesis and clinics of affective illnesses. The catecholamine and serotonin hypothesis delineated in the 1960s have retained significant merit. Since the 1990s, the theories have pointed on excessive immune activation and impairment of neuroplasticity under stress. Since the 1970s, a systematic subclassification of unipolar and bipolar affective disorder has proceeded. Epidemiological studies of the last half-century indicated a significantly higher prevalence of depression compared with previous decades. The 21st century brought evidence for a greater frequency of various forms of bipolar affective disorder. During the last 50 years, the etiopathogenesis, diagnosis and treatment of affective disorders were my favorite and fascinating clinical and research topics. This initiated in 1970 when I began my work in the Department of Psychiatry, Medical Academy in Poznan, on account of the introduction of lithium salts for the treatment of these disorders. In 1976–1977, I received a fellowship of the National Institutes of Health at the University of Pennsylvania in Philadelphia and partici- pated in research that elucidated the mechanism of lithium transport across cell membranes. I carried out the studies on the pathogenesis of affective disorders for more than 40 years afterward. -
Antipsychotic Availability (Other Than Pill/Capsule) Notes Paliperidone
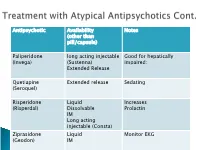
Antipsychotic Availability Notes (other than pill/capsule) Paliperidone long acting injectable Good for hepatically (Invega) (Sustenna) impaired; Extended Release Quetiapine Extended release Sedating (Seroquel) Risperidone Liquid Increases (Risperdal) Dissolvable Prolactin IM Long acting injectable (Consta) Ziprasidone Liquid Monitor EKG (Geodon) IM Supportive Psychotherapy Club House ACT services NAMI Vocational Rehab Nicotine counseling 1 (or more ) delusions Duration: 1 month or longer Criterion A for Schizophrenia has never been met. Functioning is not markedly impaired Behavior is not obviously odd or bizarre Features: Differential Diagnosis Prevalence: Obsessive-compulsive and ◦ lifetime 0.2 % related disorders ◦ Most frequent is persecutory Delirium • Males > females for Jealous major neurocognitive d/o type psychotic disorder due to • Function is generally better another medical condition than in schizophrenia substance-medication- • Familiar relationship with induced psychotic disorder schizophrenia and Schizophrenia & schizotypal Schizophreniform Depressive and bipolar d/o Schizoaffective Disorder Delusion types Erotomanic Grandiose Jealous Persecutory Somatic Mixed Unspecified • Substance Abuse • Dependence • Withdrawal ◦ Alcohol Divided into 2 ◦ Caffeine groups: ◦ Cannabis ◦ Hallucinogens (with separate ◦ Substance use categories for phencyclidine and other disorders hallucinogens) ◦ Substance-induced ◦ Inhalants disorders ◦ Opioids ◦ Sedatives, hypnotics, and anxiolytics ◦ Stimulants (amphetamine-type -

The Process People with Schizophrenia Or Schizoaffective Disorder Use to Return to Or
The Process People with Schizophrenia or Schizoaffective Disorder Use to Return to or Initially Secure Employment after Diagnosis A dissertation presented to the faculty of the College of Education of Ohio University In partial fulfillment of the requirements for the degree Doctor of Philosophy Willard A. Sheets June 2009 © Willard A. Sheets. All Rights Reserved. 2 This dissertation titled The Process People with Schizophrenia or Schizoaffective Disorder Use to Return to or Initially Secure Employment after Diagnosis by WILLARD A. SHEETS has been approved for the Department of Counseling and Higher Education and the College of Education by Tracy C. Leinbaugh Associate Professor of Counseling and Higher Education Renée A. Middleton Dean, College of Education 3 ABSTRACT SHEETS, WILLARD A., Ph.D., June 2009, Counselor Education The Process People with Schizophrenia or Schizoaffective Disorder Use to Return to or Initially Secure Employment after Diagnosis (184 pp.) Director of Dissertation: Tracy C. Leinbaugh Research indicates that people with schizophrenia or schizoaffective disorder have a high rate of unemployment. This qualitative phenomenological study was designed to explore the perceptions of eight individuals with either disorder who have secured employment after diagnosis. The rationale for this study arises from the researcher’s desire to find the process which was used by individuals with either disorder to become employed. It was the researcher’s assumption that uncovering such a process could lead to implementation of employment as a therapeutic goal of treatment with such individuals. The purposefully selected sample consisted of eight individuals from a Midwestern state who have been diagnosed with either disorder.