A Modi Catory Screening Protocol for ARDS in Patients with Respiratory
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anonymizing Classification Data Using Rough Set Theory
Knowledge-Based Systems 43 (2013) 82–94 Contents lists available at SciVerse ScienceDirect Knowledge-Based Systems journal homepage: www.elsevier.com/locate/knosys Anonymizing classification data using rough set theory ⇑ Mingquan Ye a,c, , Xindong Wu a,b, Xuegang Hu a, Donghui Hu a a Department of Computer Science, Hefei University of Technology, Hefei 230009, PR China b Department of Computer Science, University of Vermont, Burlington, VT 05405, USA c Department of Computer Science, Wannan Medical College, Wuhu 241002, PR China article info abstract Article history: Identity disclosure is one of the most serious privacy concerns in many data mining applications. A well- Received 16 April 2012 known privacy model for protecting identity disclosure is k-anonymity. The main goal of anonymizing Received in revised form 23 December 2012 classification data is to protect individual privacy while maintaining the utility of the data in building Accepted 8 January 2013 classification models. In this paper, we present an approach based on rough sets for measuring the data Available online 26 January 2013 quality and guiding the process of anonymization operations. First, we make use of the attribute reduc- tion theory of rough sets and introduce the conditional entropy to measure the classification data quality Keywords: of anonymized datasets. Then, we extend conditional entropy under single-level granulation to hierarchi- k-Anonymity cal conditional entropy under multi-level granulation, and study its properties by dynamically coarsening Rough sets Multi-level granulation and refining attribute values. Guided by these properties, we develop an efficient search metric and pres- Attribute value taxonomy ent a novel algorithm for achieving k-anonymity, Hierarchical Conditional Entropy-based Top-Down Privacy preserving data mining Refinement (HCE-TDR), which combines rough set theory and attribute value taxonomies. -

A Joint Delay-And-Sum and Fourier Beamforming Method for High Frame Rate Ultrasound Imaging
Computer Modeling in Engineering & Sciences CMES, vol.123, no.1, pp.427-440, 2020 A Joint Delay-and-Sum and Fourier Beamforming Method for High Frame Rate Ultrasound Imaging Wei Zhao1, 2, Shuai Feng1, Yadan Wang1, Yuanguo Wang1, Zhihui Han1 and Hu Peng1, * Abstract: Frame rate is an important metric for ultrasound imaging systems, and high frame rates (HFR) benefit moving-target imaging. One common way to obtain HFR imaging is to transmit a plane wave. Delay-and-sum (DAS) beamformer is a conventional beamforming algorithm, which is simple and has been widely implemented in clinical application. Fourier beamforming is an alternative method for HFR imaging and has high levels of imaging efficiency, imaging speed, and good temporal dynamic characteristics. Nevertheless, the resolution and contrast performance of HFR imaging based on DAS or Fourier beamforming are insufficient due to the single plane wave transmission. To address this problem, a joint DAS and Fourier beamforming method is introduced in this study. The proposed method considers the different distributions of sidelobes in DAS imaging and Fourier imaging and combines the angular spectrum and DAS to reconstruct ultrasound images. The proposed method is evaluated on simulation and experimental phantom datasets to compare its performance with DAS and Fourier beamforming methods. Results demonstrate that the proposed method improves image effective dynamic range and resolution while also retaining a high frame rate of the ultrasound imaging systems. The proposed method improves the effective dynamic range along axial and lateral directions by 10 dB, compared to standard DAS and Fourier beamforming. Keywords: High frame rate imaging, delay-and-sum, Fourier transformation, angular spectrum. -

Table of Codes for Each Court of Each Level
Table of Codes for Each Court of Each Level Corresponding Type Chinese Court Region Court Name Administrative Name Code Code Area Supreme People’s Court 最高人民法院 最高法 Higher People's Court of 北京市高级人民 Beijing 京 110000 1 Beijing Municipality 法院 Municipality No. 1 Intermediate People's 北京市第一中级 京 01 2 Court of Beijing Municipality 人民法院 Shijingshan Shijingshan District People’s 北京市石景山区 京 0107 110107 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Haidian District of Haidian District People’s 北京市海淀区人 京 0108 110108 Beijing 1 Court of Beijing Municipality 民法院 Municipality Mentougou Mentougou District People’s 北京市门头沟区 京 0109 110109 District of Beijing 1 Court of Beijing Municipality 人民法院 Municipality Changping Changping District People’s 北京市昌平区人 京 0114 110114 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Yanqing County People’s 延庆县人民法院 京 0229 110229 Yanqing County 1 Court No. 2 Intermediate People's 北京市第二中级 京 02 2 Court of Beijing Municipality 人民法院 Dongcheng Dongcheng District People’s 北京市东城区人 京 0101 110101 District of Beijing 1 Court of Beijing Municipality 民法院 Municipality Xicheng District Xicheng District People’s 北京市西城区人 京 0102 110102 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Fengtai District of Fengtai District People’s 北京市丰台区人 京 0106 110106 Beijing 1 Court of Beijing Municipality 民法院 Municipality 1 Fangshan District Fangshan District People’s 北京市房山区人 京 0111 110111 of Beijing 1 Court of Beijing Municipality 民法院 Municipality Daxing District of Daxing District People’s 北京市大兴区人 京 0115 -

China to Keep Watch on TPP
Table for strangers Hainan helps visitors Memory protection Special police target tourism An app connects amateur chefs industry irregularities in Sanya with willing dining companions Database to be created on > CHINA, PAGE 4 > LIFE, PAGE 9 the Nanjing Massacre > p3 MONDAY, October 12, 2015 chinadailyusa.com $1 COMMERCE China to keep watch on TPP Such trade deals can disrupt non-signatories: offi cial By ZHONG NAN highly unlikely that the TPP would in Beijing lead to the creation of a trade bloc [email protected] that excludes China. “The economic development China will conduct comprehensive mode in China has already changed and systematic assessments of the from low-end product trade to ‘going fallout from the Trans-Pacifi c Part- global’ strategies like setting up or nership, a broad agreement between moving manufacturing facilities and 12 Pacifi c Rim countries, including to more direct investment in over- Japan and the United States, since it seas markets,” said Fan. believes that such deals have disrup- Besides the US, other signatories tive eff ects on non-signatory nations, to the TPP are Australia, Brunei, a top government offi cial said. Canada, Chile, Japan, Malaysia, Mex- Commerce Minister Gao Hucheng ico, New Zealand, Peru, Singapore said China is of the view that changes and Vietnam. in the global trade pattern should be China has to date signed bilateral decided by adjustments in the indus- and multilateral free trade agree- trial structure and through product ments with seven TPP members. competitiveness in global -

Complex As Two-Photon Fluorescence Probe for Imaging Nuclear Histidine
Electronic Supplementary Material (ESI) for Chemical Communications. This journal is © The Royal Society of Chemistry 2018 A benzoic acid terpyridine-based cyclometalated iridium (III) complex as two-photon fluorescence probe for imaging nuclear histidine Qiong Zhang¶a, Xin Lu¶a, Hui Wang¶a,c, Xiaohe Tianb*, Aidong Wangd, Hongping Zhoua, Jieying Wua and Yupeng Tiana,e* [a] Department of Chemistry, Key Laboratory of Functional Inorganic Material Chemistry of Anhui Province, Anhui University, Hefei 230601, P. R. China [b] School of Life Science, Anhui University, Hefei 230601, P.R. China [c] Department of Chemistry, Wannan Medical College, Wuhu 241002, P. R. China [d] School of Chemistry and Chemical Engeering, Huangshan University, Huangshan, P. R. China. [e] State Key Laboratory of Coordination Chemistry, Nanjing University, Nanjing 210093, P. R. China ¶ These authors contributed equally to this work. E-mail address: [email protected]; [email protected] 1 Materials and instruments ..................................................................................................................3 Optical Measurements........................................................................................................................3 Synthesis of Ir1 ..................................................................................................................................3 Synthesis of Ir2 ..................................................................................................................................4 Synthesis -

SUBSTR DESCR International Schools CAMEROON 000944
SUBSTR DESCR International Schools CAMEROON 000944 Universite Yaounde CANADA 001048 Athabasca University 005528 Augustana University College 005516 Bishops University 005525 Concordia Lutheran College 002464 Keyano College 005536 Lethbridge Comm Coll 005536 Lethbridge Community College 002466 Prairie Bible College 009294 Red Deer College 005464 Southern Alberta Inst Tech 005464 Southrn Alb Inst Tec 005464 Southrn Alberta Inst Tech 005567 Univ Alberta 005435 Univ Alberta Calgary Branch 005435 Univ Calgary 005567 University Of Alberta 005469 University Of Lethbridge 003535 Capilano College 008792 Northern Lights Community Coll 006220 Northwest Cmty Coll 002313 Okanagan College 001054 Royal Roads Military Col 002193 Selkirk Col Castlegar Campus 002194 Selkirk Col Rosemont Campus 002195 Selkirk Col Trail Campus 005454 Selkirk College 005597 Simon Fraser University 005569 University Of British Columbia 005590 University Of Victoria 006310 Vancouver Comm College 005515 Brandon University 007078 Sal Army C Booth Bib 001058 United Col Winnipeg 005575 Univ Manitoba 001058 Univ Winnipeg 001058 Wesley Col Winnipeg 005545 Mount Allison University 001051 Universite De Moncton 005578 University Of New Brunswick 005497 Memorial Univ Newfou 005511 Acadia University 005524 Dalhousie University 005478 Mount St Vincent University 005459 Nova Scotia Agricultural Coll 001052 Nova Scotia Col Art Design 005557 St Francis Xavier University 005562 St Marys University International Schools 001057 Tech Univ Nova Scotia 001049 Univ Col Cape Breton 001055 Universite -

CHINA VANKE CO., LTD.* 萬科企業股份有限公司 (A Joint Stock Company Incorporated in the People’S Republic of China with Limited Liability) (Stock Code: 2202)
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. CHINA VANKE CO., LTD.* 萬科企業股份有限公司 (A joint stock company incorporated in the People’s Republic of China with limited liability) (Stock Code: 2202) 2019 ANNUAL RESULTS ANNOUNCEMENT The board of directors (the “Board”) of China Vanke Co., Ltd.* (the “Company”) is pleased to announce the audited results of the Company and its subsidiaries for the year ended 31 December 2019. This announcement, containing the full text of the 2019 Annual Report of the Company, complies with the relevant requirements of the Rules Governing the Listing of Securities on The Stock Exchange of Hong Kong Limited in relation to information to accompany preliminary announcement of annual results. Printed version of the Company’s 2019 Annual Report will be delivered to the H-Share Holders of the Company and available for viewing on the websites of The Stock Exchange of Hong Kong Limited (www.hkexnews.hk) and of the Company (www.vanke.com) in April 2020. Both the Chinese and English versions of this results announcement are available on the websites of the Company (www.vanke.com) and The Stock Exchange of Hong Kong Limited (www.hkexnews.hk). In the event of any discrepancies in interpretations between the English version and Chinese version, the Chinese version shall prevail, except for the financial report prepared in accordance with International Financial Reporting Standards, of which the English version shall prevail. -

A Benzoic Acid Terpyridine-Based Cyclometalated Iridium(Iii) Complex As a Two-Photon Fluorescence Probe for Imaging Nuclear Hist
ChemComm COMMUNICATION A benzoic acid terpyridine-based cyclometalated iridium(III) complex as a two-photon fluorescence Cite this: Chem. Commun., 2018, 54, 3771 probe for imaging nuclear histidine† Received 2nd February 2018, a a ab c d Accepted 14th March 2018 Qiong Zhang, ‡ Xin Lu, ‡ Hui Wang, ‡ Xiaohe Tian, * Aidong Wang, Hongping Zhou, a Jieying Wu a and Yupeng Tian *ae DOI: 10.1039/c8cc00908b rsc.li/chemcomm A series of two-photon active cyclometalated iridium(III) complexes include reduced photobleaching, autofluorescence, non-invasive (Ir1, Ir2 and Ir3) were designed. Ir1 with a two-photon action cross- excitation, and deeper tissue penetration.8–10 However, two- section of 40 GM in the NIR region has been developed for photon absorption (2PA) materials with moderate two-photon targeting intracellular histidine. Two-photon micrographs showed absorption cross-section (s) values usually possess extended that Ir1 could rapidly and selectively light up the nucleus in both p-conjugated planar structures, consequently leading to the use fixed and live cells and is capable of displaying nuclear histidine of biologically unfriendly solvents (e.g. DMSO). Therefore, the distribution in ultra-detail using a super resolution (SR) technique design and synthesis of novel fluorescent probes with histidine under stimulated emission depletion (STED) microscopy. specificity still remain a challenge.11 Recently, the use of precious-metal complexes such as Ru(II), Among the twenty amino acids, histidine is active in maintaining Ir(III) and Pt(II) as luminescent probes has attracted increasing healthy tissues and protecting nerve cells that transport messages interest due to their advantageous photophysical properties and 1,2 12 from the brain to the various other parts of the body. -

A Complete Collection of Chinese Institutes and Universities For
Study in China——All China Universities All China Universities 2019.12 Please download WeChat app and follow our official account (scan QR code below or add WeChat ID: A15810086985), to start your application journey. Study in China——All China Universities Anhui 安徽 【www.studyinanhui.com】 1. Anhui University 安徽大学 http://ahu.admissions.cn 2. University of Science and Technology of China 中国科学技术大学 http://ustc.admissions.cn 3. Hefei University of Technology 合肥工业大学 http://hfut.admissions.cn 4. Anhui University of Technology 安徽工业大学 http://ahut.admissions.cn 5. Anhui University of Science and Technology 安徽理工大学 http://aust.admissions.cn 6. Anhui Engineering University 安徽工程大学 http://ahpu.admissions.cn 7. Anhui Agricultural University 安徽农业大学 http://ahau.admissions.cn 8. Anhui Medical University 安徽医科大学 http://ahmu.admissions.cn 9. Bengbu Medical College 蚌埠医学院 http://bbmc.admissions.cn 10. Wannan Medical College 皖南医学院 http://wnmc.admissions.cn 11. Anhui University of Chinese Medicine 安徽中医药大学 http://ahtcm.admissions.cn 12. Anhui Normal University 安徽师范大学 http://ahnu.admissions.cn 13. Fuyang Normal University 阜阳师范大学 http://fynu.admissions.cn 14. Anqing Teachers College 安庆师范大学 http://aqtc.admissions.cn 15. Huaibei Normal University 淮北师范大学 http://chnu.admissions.cn Please download WeChat app and follow our official account (scan QR code below or add WeChat ID: A15810086985), to start your application journey. Study in China——All China Universities 16. Huangshan University 黄山学院 http://hsu.admissions.cn 17. Western Anhui University 皖西学院 http://wxc.admissions.cn 18. Chuzhou University 滁州学院 http://chzu.admissions.cn 19. Anhui University of Finance & Economics 安徽财经大学 http://aufe.admissions.cn 20. Suzhou University 宿州学院 http://ahszu.admissions.cn 21. -

Research Article the Effects of Sidt2 on the Inflammatory Pathway in Mouse Mesangial Cells
Hindawi Mediators of Inflammation Volume 2020, Article ID 3560793, 9 pages https://doi.org/10.1155/2020/3560793 Research Article The Effects of Sidt2 on the Inflammatory Pathway in Mouse Mesangial Cells Hui Sun,1,2 Jia-ming Ding,3 Hui-hao Zheng,4 Kang-jia Lv,3 Yun-fei Hu,1,2 Ying-hui Luo,5 Xue Wu,1,2 Wen-jun Pei,6 Li-zhuo Wang,2,7 Ming-cai Wu,7 Yao Zhang,6,7 and Jia-lin Gao 1,2,6 1Department of Endocrinology and Genetic Metabolism, Yijishan Hospital of Wannan Medical College, Wuhu 241002, China 2Institute of Endocrine and Metabolic Diseases, Yijishan Hospital of Wannan Medical College, Wuhu 241002, China 3School of Clinical Medicine, Wannan Medical College, Wuhu 241002, China 4School of Medical Imaging, Wannan Medical College, Wuhu 241002, China 5School of Pharmacy, Wannan Medical College, Wuhu 241002, China 6Anhui Province Key Laboratory of Biological Macro-molecules Research, Wannan Medical College, Wuhu 241001, China 7Department of Biochemistry and Molecular Biology, Wannan Medical College, Wuhu 241002, China Correspondence should be addressed to Jia-lin Gao; [email protected] Received 7 March 2020; Accepted 2 May 2020; Published 28 May 2020 Academic Editor: Daniela Caccamo Copyright © 2020 Hui Sun et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In patients with chronic kidney disease, the abnormal activation of inflammatory pathways is usually an important factor leading to renal fibrosis and further deterioration of renal function. -

Trematodos Aspidogastrea Encontrados En Los Mejillones De
Nutr Hosp. 2017; 34(2):460-462 ISSN 0212-1611 - CODEN NUHOEQ S.V.R. 318 Nutrición Hospitalaria Trabajo Original Otros Trematode Aspidogastrea found in the freshwater mussels in the Yangtze River basin Trematodos Aspidogastrea encontrados en los mejillones de agua dulce en la cuenca del río Yangtze Xiaodong Zhan1, Chaopin Li1,2 and Hua Wu1 1Department of Medical Parasitology. Wannan Medical College. Wuhu, Anhu. China. 2School of Medicine. Anhui University of Science & Technology. Huainan, Anhui. China Abstract Objective: To investigate the prevalence of trematode Aspidogastrea in the freshwater mussels in the Yangtze River basin within Anhui province, China. Methods: We initially harvested the freshwater mussels living in the Yangtze River running through Anhui area, and labeled them with corre- sponding number. Then the samples were dissected for isolating the fl ukes, which were identifi ed by conventional staining. Results: Infection rate of trematode Aspidogastrea in freshwater mussels in the Yangtze River basin within the territory of Anhui province was Key words: 30.38% (103/339) in general, and a total of 912 fl ukes of Aspidogastrea were detected in the 103 mussels, with average infection rate of 8.85 for each mussel. Freshwater mussels. Aspidogastrea. Conclusion: Trematode Aspidogastrea is prevalent in the freshwater bivalves living in the Yangtze River basin running through Anhui area, and Trematode. the treamatode was identifi ed asAspidogaster sp. belong to Aspidogaste under Aspidogastridae of Aspidogastrea. Resumen Objetivo: investigar la prevalencia de trematodos Aspidogastrea en mejillones de agua dulce en la cuenca del río Yangtze en la provincia de Anhui, China. Métodos: se recogieron mejillones de agua dulce en el río Yangtze a su paso por la provincia de Anhui y se etiquetaron con su número corres- pondiente. -
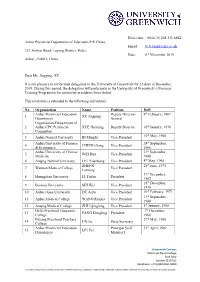
Dear Ms. Jingping, XU It Is My Pleasure to Invite Your Delegation To
Direct line: 0044 (0) 208 331 8882 Anhui Provincial Department of Education P.R China, Email: [email protected] 321 Jinzhai Road, Luyang District, Hefei, Date: 6th November 2019 Anhui, 230061, China Dear Ms. Jingping, XU It is my pleasure to invite your delegation to the University of Greenwich for 21 days in December, 2019. During this period, the delegation will participate in the University of Greenwich’s Overseas Training Programme for university presidents from Anhui. This invitation is extended to the following individuals: No. Organisation Name Position DoB Anhui Provincial Education Deputy Director- 9th February, 1967 1 XU Jingping Department General Organisation Department of 2 Anhui CPC Provincial XUE Huiming Deputy Director 10th January, 1976 Committee th 3 Anhui Normal University BI Mingfu Vice President 10 May, 1968 Anhui University of Finance 24th September, 4 CHENG Gang Vice President & Economics 1966 Anhui University of Chinese 21st September, 5 WEI Hua Vice President Medicine 1966 6 Anqing Normal University LIU Youzhong Vice President 4th May, 1965 ZHENG 28th June, 1975 7 Wannan Medical College Vice President Lanrong 31st December, 8 Huangshan University LI Tiefan President 1967 18th December, 9 Bozhou University SHI Wei Vice President 1970 10 Anhui Open University DU Aiyu Vice President 16th February, 1971 11th September, 11 Anhui Medical College WANG Runxia Vice President 1968 12 Anqing Medical College ZHU Qingfeng Vice President 5th January, 1968 Hefei Preschool Education 7th December, 13 FANG Dongling President College 1968 Fuyang Preschool Teachers 27th May, 1968 14 JIN Jie Party Secretary College Anhui Provincial Education Principal Staff 21st April, 1981 15 LIU Fei Department Member I Greenwich Campus Old Royal Naval College Park Row London SE10 9LS Telephone: +44 (0)20 8331 8000 University of Greenwich, a charity and company limited by guarantee, registered in England (reg no.986729).