Tameside Pharmaceutical Needs Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The List of Pharmacies Registered to Sell Ppcs on Our Behalf Is Sorted Alphabetically in Postcode Order
The list of pharmacies registered to sell PPCs on our behalf is sorted alphabetically in postcode order. 0 NAME PREMISES ADDRESS 1 PREMISES ADDRESS 2 PREMISES ADDRESS 3 PREMISES ADDRESS 4 LLOYDS PHARMACY SAINSBURYS, EVERARD CLOSE ST ALBANS HERTFORDSHIRE AL1 2QU BOOTS UK LIMITED 9 ST PETERS STREET ST.ALBANS HERTFORDSHIRE AL1 3DH FREEMAN GRIEVES LTD 111-113 ST PETERS STREET ST.ALBANS HERTFORDSHIRE AL1 3ET LLOYDS PHARMACY PARKBURY HOUSE ST PETER ST ALBANS HERTFORDSHIRE AL1 3HD IMED PHARMACY 67 HATFIELD ROAD ST ALBANS HERTFORDSHIRE AL1 4JE LLOYDS PHARMACY SAINSBURYS, BARNET ROAD LONDON COLNEY ST ALBANS HERTFORDSHIRE AL2 1AB LLOYDS PHARMACY 17 RUSSELL AVENUE ST ALBANS HERTFORDSHIRE AL3 5ES CROWN PHAMRACY 65 HIGH STREET REDBOURN ST ALBANS HERTFORDSHIRE AL3 7LW MANOR PHARMACY (WHEATHAMPSTEAD) LTD 2 HIGH STREET WHEATHAMPSTEAD HERTFORDSHIRE AL4 8AA BOOTS UK LIMITED 23-25 HIGH STREET HARPENDEN HERTFORDSHIRE AL5 2RU LLOYDS PHARMACY 40 HIGH STREET WELWYN GARDEN CITY HERTFORDSHIRE AL6 9EQ LLOYDS PHARMACY 84 HALDENS WELWYN GARDEN CITY HERTFORDSHIRE AL7 1DD BOOTS UK LIMITED 65 MOORS WALK WELWYN GARDEN CITY HERTFORDSHIRE AL7 2BQ BOOTS UK LIMITED 31 COLE GREEN LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3PP PEARTREE PHARMACY 110 PEARTREE LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3UJ BOOTS UK LIMITED 126 PEARTREE LANE WELWYN GARDEN CITY HERTFORDSHIRE AL7 3XY BOOTS UK LIMITED 31 THE HOWARD CENTRE WELWYN GARDEN CITY HERTFORDSHIRE AL8 6HA LLOYDS PHARMACY SAINSBURYS, CHURCH ROAD WELWYN GARDEN CITY HERTFORDSHIRE AL8 6SA LLOYDS PHARMACY 9 SHOPLANDS WELWYN GARDEN -
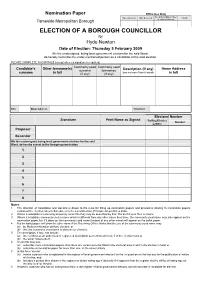
Nomination Paper Pack for By-Election of Hyde Newton on 5Th
Nomination Paper Office Use Only No of Nomination Paper Time delivered Date delivered Initials Tameside Metropolitan Borough in order of delivery ELECTION OF A BOROUGH COUNCILLOR for Hyde Newton Date of Election: Thursday 5 February 2009 We the undersigned, being local government electors for the said Ward , do hereby nominate the under-mentioned person as a candidate at the said election. PLEASE COMPLETE IN CAPITALS (except where a signature is required) Candidate’s Other forename(s) Commonly used Commonly used Home Address surname forenames Description (if any) use no more than 6 words surname in full (if any) (if any) in full Title Email Address Telephone Electoral Number Signature Print Name as Signed Polling District Number Letters Proposer Seconder We the undersigned, being local government electors for the said Ward, do hereby assent to the foregoing nomination 1 2 3 4 5 6 7 8 Notes 1. The attention of candidates and electors is drawn to the rules for filling up nomination papers and provisions relating to nomination papers contained the election rules in Schedule 2 to the Local Election (Principle Areas) Rules 2006. 2. Where a candidate is commonly known by some title they may be described by their title as if it were their surname. 3. Where a candidate commonly uses a name which is different from any other name they have, the commonly used name may also appear on the nomination paper, but if it does so, the commonly used name (instead of any other name) will appear on the ballot paper. 4. But the ballot paper will show the other name if the Returning Officer thinks that the use of the commonly used name may (a) be likely to mislead or confuse electors, or (b) that the commonly used name is obscene or offensive. -

Minor Eye Conditions Service (MECS) Tameside and Glossop Pharmacies That Are Currently Providing Mecs
Minor Eye Conditions Service (MECS) Tameside and Glossop Pharmacies that are currently providing MECs Name Address Telephone 169 Mossley Road, Ashton-under-Lyne, Lancashire, OL6 Adams Pharmacy 6NE 0161 339 8889 Stalybridge Resource Centre, 2 Waterloo Road, Stalybridge. Adams Pharmacy SK15 2AU 0161 303 8599 Alipharma Ltd Thornley House Med Ctr) 11 Thornley Street, Hyde SK14 1JY 0161 351 1386 Asda Cavendish Street, Ashton Under Lyne, OL6 7DP 0161 342 6610 Asda Water Street, Hyde, Cheshire, SK14 1BD 0161 882 5700 22 Stockport Road, Ashton-Under-Lyne, Lancashire, OL7 Ashton Pharmacy 0LB 0161 330 4389 Ashton Primary Care Centre Pharmacy 193 Old Street, Ashton-Under-Lyne, Lancashire, OL6 7SR 0161 820 8281 Audenshaw Pharmacy 3 Chapel Street, Audenshaw, Manchester, M34 5DE 0161 320 9123 Boots 116-118 Station Road, Hadfield, Glossop SK13 1AJ 01457 853635 Hattersley Health Centre, Hattersley Road East, Hattersley, Boots Hyde SK14 3EH 0161 368 8498 Boots 72 Market Street, Droylsden, Manchester M43 6DE 0161 370 1626 Boots 30 Concorde Way, Dukinfield, Cheshire SK16 4DB 0161 330 3586 Boots 173 Mossley Road, Ashton-Under-Lyne OL6 6NE 0161 330 1303 Boots 1-3 Bow Street, Ashton-Under-Lyne OL6 6BU 0161 330 1746 Boots UK Ltd 15-17 Staveleigh Way, Ashton-Under-Lyne OL6 7JL 0161 308 2326 Boots UK Ltd 19 High Street West, Glossop, Derbyshire SK13 8AL 01457 852011 Boots UK Ltd 1A Market Place, Hyde, Cheshire SK14 2LX 0161 368 2249 Boots UK Ltd 33 Queens Walk, Droylsden, Manchester M43 7AD 0161 370 1402 Crown Point North, Retail Park, Ashton Road, Denton M34 -

Parliamentary Debates (Hansard)
Tuesday Volume 512 29 June 2010 No. 23 HOUSE OF COMMONS OFFICIAL REPORT PARLIAMENTARY DEBATES (HANSARD) Tuesday 29 June 2010 £5·00 © Parliamentary Copyright House of Commons 2010 This publication may be reproduced under the terms of the Parliamentary Click-Use Licence, available online through the Office of Public Sector Information website at www.opsi.gov.uk/click-use/ Enquiries to the Office of Public Sector Information, Kew, Richmond, Surrey TW9 4DU; e-mail: [email protected] 697 29 JUNE 2010 698 almost identical to the chances in the rest of Europe. House of Commons Does the Secretary of State therefore believe that a one-year survival indicator is a good idea both for Tuesday 29 June 2010 encouraging early diagnosis and for matching the survival rates of the best in Europe? The House met at half-past Two o’clock Mr Lansley: My hon. Friend makes an extremely good point. When we set out proposals for an outcomes PRAYERS framework, I hope that he and others will respond, because that is one of the ways in which we can best identify how late detection of cancer is leading to very [MR SPEAKER in the Chair] poor levels of survival to one year. I hope that we can think about that as one of the quality indicators that we shall establish. Oral Answers to Questions Diana R. Johnson (Kingston upon Hull North) (Lab): I welcome the Secretary of State to his new position and wish him well in his role. I understand that he is keeping HEALTH the two-week target for seeing a cancer specialist, but abandoning the work that the Labour Government did on the one-week target for access to diagnostic testing. -

NOTICE of PARTICULARS of ELECTION SUB-AGENTS Combined Authority Mayoral Election for the Greater Manchester Combined Authority Thursday 6 May 2021
NOTICE OF PARTICULARS OF ELECTION SUB-AGENTS Combined Authority Mayoral Election for the Greater Manchester Combined Authority Thursday 6 May 2021 I HEREBY GIVE NOTICE that the following names and addresses of election sub-agents of candidates at this election, and the addresses of the offices of such election sub-agents to which all claims, notices, legal process, and other documents addressed to them may be sent, have been declared in writing to me as follows:- Part of the Office of Election Combined Sub-agent to which Name of Election Authority for which Address of Election Name of Candidate claims, notices, legal Sub-agent the Election Sub- Sub-agent process, etc. may be agent is appointed sent to act 69 Manor Road 69 Manor Road Levenshulme Levenshulme BURNHAM WILLIAMS District of Manchester Manchester Andy Tom Manchester Greater Manchester Greater Manchester M19 3EU M19 3EU 43 Thorn Road 43 Thorn Road Swinton BURNHAM DICKMAN Swinton District of Salford Manchester Andy Stuart Manchester M27 5QU M27 5QU 12 Cliffe Court 12 Cliffe Court BURNHAM BRADSHAW Bury South Preston Preston Andy Lee Constituency PR1 4QB PR1 4QB 116 Ainsworth Road 116 Ainsworth Road BURNHAM SMITH Bury North Bury Bury Andy John Constituency Lancashire Lancashire BL8 2RX BL8 2RX 387 Leigh Road 387 Leigh Road BURNHAM ANDERSON Hindley Green Hindley Green District of Wigan Andy Dane Wigan Wigan WN2 4XL WN2 4XL Apartment 18 Apartment 18 Provender Court Provender Court BURNHAM WESTERN District of Trafford 3 ProvenderClose 3 ProvenderClose Andy Andrew Altrincham Altrincham -

Submission to the Boundary Commission for England 2013 Review North West Region Greater Manchester and Lancashire
Submission to the Boundary Commission for England 2013 Review North West Region Greater Manchester and Lancashire Andrew Teale December 4, 2011 Abstract This submission disagrees with and presents a counter-proposal to the Boundary Commission for England’s proposals for new parliamentary con- stituency boundaries in Greater Manchester and Lancashire. The counter- proposal allocates seven whole constituencies to the boroughs of Stockport, Tameside and Oldham, nine whole constituencies to the boroughs of Man- chester, Salford and Trafford, and twenty-four whole constituencies to the rest of the region. No comment is made on the Boundary Commission’s proposals for the rest of the North West region or for any other region. Contents 1 Introduction2 1.1 The statutory criteria.........................2 1.2 Splitting of wards...........................3 2 Theoretical entitlements4 3 Southern Greater Manchester5 3.1 Manchester, Salford and Trafford..................5 3.2 Oldham, Stockport and Tameside.................. 10 4 Lancashire and Northern Greater Manchester 14 4.1 Crossing the boundary between Greater Manchester and Lancashire 16 4.2 Rochdale................................ 17 4.3 Bolton, Bury, Wigan and Rossendale................ 18 4.4 South Lancashire........................... 22 4.5 East Lancashire............................ 23 4.6 North Lancashire........................... 24 4.7 Summary................................ 25 5 Closing remarks 28 1 1 Introduction This document is my submission to the 2013 Review of Parliamentary constit- uency boundaries. I should first introduce myself. I am the editor and webmaster of the Lo- cal Elections Archive Project (http://www.andrewteale.me.uk/leap/), the in- ternet’s largest freely available collection of British local election results. I have been for some years a contributor to election-related web forums, and this submission is based on material originally posted on the Vote UK forum (http://www.vote-2007.co.uk/) and in some cases modified in the light of comments made. -

Tameside Locality Assessments GMSF 2020
November 2020 Transport Locality Assessments Introductory Note and Assessments – Tameside allocations GMSF 2020 Table of contents 1. Background 2 1.1 Greater Manchester Spatial Framework (GMSF) 2 1.2 Policy Context – The National Planning Policy Framework 3 1.3 Policy Context – Greater Manchester Transport Strategy 2040 5 1.4 Structure of this Note 9 2. Site Selection 10 2.1 The Process 10 2.2 Greater Manchester Accessibility Levels 13 3. Approach to Strategic Modelling 15 4. Approach to Technical Analysis 17 4.1 Background 17 4.2 Approach to identifying Public Transport schemes 18 4.3 Mitigations and Scheme Development 19 5. Conclusion 23 6. GMSF Allocations List 24 Appendix A - GMA38 Ashton Moss West Locality Assessment A1 Appendix B - GMA39 Godley Green Garden Village Locality Assessment B1 Appendix C - GMA40 Land South of Hyde Locality Assessment C1 1 1. Background 1.1 Greater Manchester Spatial Framework (GMSF) 1.1.1 The GMSF is a joint plan of all ten local authorities in Greater Manchester, providing a spatial interpretation of the Greater Manchester Strategy which will set out how Greater Manchester should develop over the next two decades up to the year 2037. It will: ⚫ identify the amount of new development that will come forward across the 10 Local Authorities, in terms of housing, offices, and industry and warehousing, and the main areas in which this will be focused; ⚫ ensure we have an appropriate supply of land to meet this need; ⚫ protect the important environmental assets across the conurbation; ⚫ allocate sites for employment and housing outside of the urban area; ⚫ support the delivery of key infrastructure, such as transport and utilities; ⚫ define a new Green Belt boundary for Greater Manchester. -

Boundary Review 2013 England Secondary Consultation
Boundary Review 2013 England Secondary Consultation Submission of the Labour Party Page 1 of 50 1) General Points a) Submission This submission is made on behalf of the Labour Party and the nine regional Labour parties within England. The submission represents the Labour’s Party’s response to the representations made to the Commission, both orally at the public hearings and in writing during the Initial Consultation Period and published by the Commission on 6 March 2012. The Labour Party made a detailed formal submission of its own which included a number of counter proposals. We have now considered the options further in each region, including those counter proposals submitted by others. We will refer to them in this response. While we are not formally amending our submission we will indicate those points and proposals with which we agree, and those with which we disagree. b) Factors to be considered In assessing the merits of different proposals we will as far as possible be guided by the stipulations of Clause 5 (1) of Schedule 2 to the Parliamentary Voting System and Constituencies Act 2011 which lays down the rules by which the Commission shall conduct the review. Under the terms of the Act1, the Commission may, in choosing between different schemes, take into account i) Special Geographical Circumstances, including the size shape and accessibility of a constituency ii) Local government boundaries iii) The boundaries of existing constituencies iv) Any local ties that would be broken by changes to constituencies 1 Parliamentary Voting System and Constituencies Act 2011, Schedule 2 Clause 5 (1). -

COUNCIL 25 May 2021 Present: Councillors Kitchen (Chair), Affleck
COUNCIL 25 May 2021 Present: Councillors Kitchen (Chair), Affleck, Alam, Billington, Bowden, Bowerman, Boyle, Bray, Cartey, Chadwick, Choksi, Cooney, Cooper, Costello, Dickinson, Drennan, Fairfoull, Feeley, J Fitzpatrick, P Fitzpatrick, Glover, Gosling Gwynne, A Holland, B Holland, J Homer, S Homer, Huntbach, Jackson, Jones, Lane, Lewis, McNally, Martin, Mills, Naylor, Newton, North, Owen, Patel, Patrick, Pearce, Quinn, Reid, Ricci, Robinson, Ryan, N Sharif, T Sharif, M Smith, T Smith, Sweeton, Taylor, Ward, Warrington, R Welsh and Wills 1 ELECTION OF CIVIC MAYOR It was moved by Councillor Owen, seconded by Councillor Fairfoull and RESOLVED That Councillor Janet Cooper, be and is hereby elected Civic Mayor of the Metropolitan Borough of Tameside for the ensuing Municipal Year 2 ELECTION OF DEPUTY MAYOR It was moved by Councillor Choksi, seconded by Councillor Lewis and RESOLVED That Councillor Glover be and is hereby appointed Deputy Mayor of the Metropolitan Borough of Tameside for the ensuing Municipal Year 3. APPOINTMENT OF CHAIR OF COUNCIL BUSINESS It was moved by Councillor Warrington, seconded by Councillor Fairfoull and RESOLVED That Councillor Kitchen be appointed Chair of Council Business for the Municipal Year 2021/22. 4. DECLARATION OF INTEREST There were no declarations of interest. 5. COUNCIL MINUTES Consideration was given to the minutes of the meeting of Council held on 23 February 2021. RESOLVED That the Minutes of the meeting of Council held on 23 February 2021 be signed by the Chair of Council Business as a correct record. 6. ELECTION OF COUNCILLORS A report of the Returning Officer was received detailing the persons elected to the office of Councillor for the Wards of the Borough For details see Appendix A to the minutes. -

Denton & Reddish Labour Party, C/O 139 St Anne’S Road, Denton M34 3DY Denton South Delivered FREE by Volunteers √" " Local Oice SPRING 2014 DENTON
Printed by Greatledge, Malaga House, Pink Bank Lane, Manchester M11 2EU Promoted by Denton & Reddish Labour Party, c/o 139 St Anne’s Road, Denton M34 3DY Denton South Delivered FREE by volunteers √" " local oice SPRING 2014 DENTON , chosen for seat again Cllr. Claire Francis Local Labour Councillor Claire Francis, , at the opening has been picked once again to contest Cllr. Claire Francis ‘Oasis’ the Denton South seat in the Tameside of the Haughton Green Council Elections on Thursday 22nd May. Claire has worked hard over the last four years alongside Councillors Mike Fowler, NEW LIFE FOR HG LIBRARY Margaret Downs and local residents, to get a fairer deal for our town. Claire Francis attended the official opening of the ‘Oasis’, the former Haughton Green Library building, which Irwell Valley took on after Tory Government funding cuts forced its closure. Already they have a wide variety of activities happening every week. Claire said: “Denton South is lucky to have Irwell Valley working hard to improve the area and it’s fantastic to know that the local community are willing to work with us all to help preserve vital facilities.” Since 2010, the equivalent of * across Denton and Reddish almost 50p in every £1 has 1,295 families , been cut from Tameside’s grant (which including many by the with Tory disabled Bedroom are Tax are being penalised disability. by this Tory-led Government. including many with a * including the effect of inflation on spending power Labour will scrap this unfair charge . " Andrew Gwynne says Denton’s MP, .penalised Labour’s Claire Francis – Working hard for YOU all year round. -

Area Profile
A profile of needs and s Services about children, young people and their families In the Hyde, Hattersley & Longdendale area of Tameside September 2007 Hyde, Hattersley & Longdendale: Profile of need and services Introduction This is a selective statistical profile of needs and services in the Hyde, Hattersley & Longdendale area, this is one of four areas chosen as a basis from which future integrated services for children, young people and their families will be delivered. The other areas are Ashton-under-Lyne: Denton, Droylsden & Audenshaw and Stalybridge, Mossley & Dukinfield. Companion profiles of these other areas are also available. This profile has a focus on data that has relevance to children and families rather than other community members (e.g. older people). The data selected is not exhaustive, rather key indicators of need are selected to help produce an overall picture of need in the area and offer some comparisons between localities (mainly wards) within the area. Some commentary is provided as appropriate. It is expected that the profile will aid the planning and delivery of services. The profile has two parts: Part 1 focuses on the presentation of basic need data, whilst Part 2 focuses on services. The top three categories of the new occupational classification are ‘Managers & Senior Officials; Professionals’ and Associate Professional & Technical’ (hatched at the top of the graph on right) Tameside as a whole comes 350 th out of 376 in the country for Professional; and bottom in Greater Manchester for all three categories -

Tameside Housing Need Assessment (HNA) (2017) Provides the Latest Available Evidence to Help to Shape the Future Planning and Housing Policies of the Area
Tameside Housing Need Assessment (HNA) 2017 Tameside Metropolitan Borough Council Final Report December 2017 Main Contact: Michael Bullock Email: [email protected] Telephone: 0800 612 9133 Website: www.arc4.co.uk © 2017 arc4 Limited (Company No. 06205180) Tameside HNA 2017 Page | 2 Table of contents Executive summary ......................................................................................................................... 8 Introduction ........................................................................................................................ 8 The Housing Market Area (HMA) ........................................................................................ 8 The current housing market ................................................................................................ 9 Understanding the future housing market ....................................................................... 11 The need for all types of housing ...................................................................................... 11 Conclusion ......................................................................................................................... 14 1. Introduction ...................................................................................................................... 15 Background and objectives ............................................................................................... 15 National Planning Policy Framework (NPPF), Planning Practice Guidance (PPG) and other requirements