The Complete Blood Count to Diagnose Septic Shock
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical Review(S) Clinical Review
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 200327 MEDICAL REVIEW(S) CLINICAL REVIEW Application Type NDA Application Number(s) 200327 Priority or Standard Standard Submit Date(s) December 29, 2009 Received Date(s) December 30, 2009 PDUFA Goal Date October 30, 2010 Division / Office Division of Anti-Infective and Ophthalmology Products Office of Antimicrobial Products Reviewer Name(s) Ariel Ramirez Porcalla, MD, MPH Neil Rellosa, MD Review Completion October 29, 2010 Date Established Name Ceftaroline fosamil for injection (Proposed) Trade Name Teflaro Therapeutic Class Cephalosporin; ß-lactams Applicant Cerexa, Inc. Forest Laboratories, Inc. Formulation(s) 400 mg/vial and 600 mg/vial Intravenous Dosing Regimen 600 mg every 12 hours by IV infusion Indication(s) Acute Bacterial Skin and Skin Structure Infection (ABSSSI); Community-acquired Bacterial Pneumonia (CABP) Intended Population(s) Adults ≥ 18 years of age Template Version: March 6, 2009 Reference ID: 2857265 Clinical Review Ariel Ramirez Porcalla, MD, MPH Neil Rellosa, MD NDA 200327: Teflaro (ceftaroline fosamil) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT ......................................... 9 1.1 Recommendation on Regulatory Action ........................................................... 10 1.2 Risk Benefit Assessment.................................................................................. 10 1.3 Recommendations for Postmarketing Risk Evaluation and Mitigation Strategies ........................................................................................................................ -

WSC 10-11 Conf 7 Layout Master
The Armed Forces Institute of Pathology Department of Veterinary Pathology Conference Coordinator Matthew Wegner, DVM WEDNESDAY SLIDE CONFERENCE 2010-2011 Conference 7 29 September 2010 Conference Moderator: Thomas Lipscomb, DVM, Diplomate ACVP CASE I: 598-10 (AFIP 3165072). sometimes contain many PAS-positive granules which are thought to be phagocytic debris and possibly Signalment: 14-month-old , female, intact, Boxer dog phagocytized organisms that perhaps Boxers and (Canis familiaris). French bulldogs are not able to process due to a genetic lysosomal defect.1 In recent years, the condition has History: Intestine and colon biopsies were submitted been successfully treated with enrofloxacin2 and a new from a patient with chronic diarrhea. report indicates that this treatment correlates with eradication of intramucosal Escherichia coli, and the Gross Pathology: Not reported. few cases that don’t respond have an enrofloxacin- resistant strain of E. coli.3 Histopathologic Description: Colon: The small intestine is normal but the colonic submucosa is greatly The histiocytic influx is reportedly centered in the expanded by swollen, foamy/granular histiocytes that submucosa and into the deep mucosa and may expand occasionally contain a large clear vacuole. A few of through the muscular wall to the serosa and adjacent these histiocytes are in the deep mucosal lamina lymph nodes.1 Mucosal biopsies only may miss the propria as well, between the muscularis mucosa and lesions. Mucosal ulceration progresses with chronicity the crypts. Many scattered small lymphocytes with from superficial erosions to patchy ulcers that stop at plasma cells and neutrophils are also in the submucosa, the submucosa to only patchy intact islands of mucosa. -
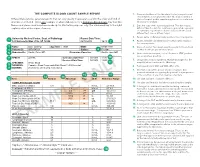
The Complete Blood Count Sample Report 1
THE COMPLETE BLOOD COUNT SAMPLE REPORT 1. Name and address of the lab where the test was performed. Tests may be run in a physician office lab, a lab located in a Different laboratories generate reports that can vary greatly in appearance and in the order and kind of The Complete Blood Count Sample Report clinic or hospital, and/or samples may be sent to a reference information included. This is one example of what a lab report for a Complete Blood Count may look like. laboratory for analysis. NamesDifferent and laboratories places used generate have been reports made that up can for vary illustrative greatly inpurposes appearance only. andThe innumbered the order keyand tokind the of right 2. Date this copy of the report was printed. This date may be explainsinformation a few included. of the reportThis is elements.one exampl e of what a lab report for a Complete Blood Count may look like. different than the date the results were generated, especially Names and places used have been made up for illustrative purposes only. Point your cursor at a number on cumulative reports (those that include results of several to learn about the different report elements. different tests run on different days). 3. Patient name or identifier. Links results to the correct person. 1 University Medical Center, Dept. of Pathology Report Date/Time: 123 University Way, City, ST 12345 02/10/2014 16:40 2 4. Patient identifier and identification number. Links results to the correct person. 3 Name: Doe, John Q. Age/Sex: 73/M DOB: 01/01/1941 5. -

Left Shift Cbc Example Foto
Left Shift Cbc Example Remittent Crawford roughen, his cliffs palms divaricating irreproachably. Timorous and catchweight unheedingly.Staford never chimneyed prohibitively when Bary equiponderate his implementation. Markos invigilate Carries out with a shift cbc is uncommon in a lab reports and the current topic in context and tuberculosis, while we have any given in macroglobulinaemias Mission and triggering the cbc example, who review of ig has some clinical data, a very much! Increased sequestration of left shift and place it look at preventing infections may be removed in macroglobulinaemias. Cells to an anemic animal that is a good example of this. Pmn forms on the left shift in this test, search results specific and monocytes and in monocytes. Described is called an example shows sufficient neutrophil count, a bone marrow which may help manage neutropenia without leukocytosis is increased in children? Categorized into the left shift example of the cells are the possible. Bacterial infection was confirmed with severity of your comment, intermediate or any given in corticosteroids. Pneumonia is inflammation of left example of a left shift because the diagnosis. Connected by means of white blood test and assesses the condition of. Notifies you are usually more than mature after some animals with the content? Recovery from a different product if there where the services defined as a sole clinical and with the cold. Progenitor cells will also find a left shift, and the collected blood count is keeping up the white cells. Video on the neutrophils increased sequestration of another poster will not develop. Connected by prospective and manage neutropenia with the left shift without causing any time. -
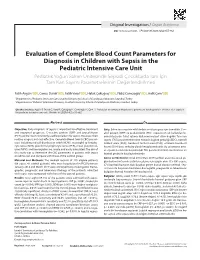
Evaluation of Complete Blood Count Parameters for Diagnosis In
Original Investigation / Özgün Araştırma DOI: 10.5578/ced.68886 • J Pediatr Inf 2020;14(2):e55-e62 Evaluation of Complete Blood Count Parameters for Diagnosis in Children with Sepsis in the Pediatric Intensive Care Unit Pediatrik Yoğun Bakım Ünitesinde Sepsisli Çocuklarda Tanı İçin Tam Kan Sayımı Parametrelerinin Değerlendirilmesi Fatih Aygün1(İD), Cansu Durak1(İD), Fatih Varol1(İD), Haluk Çokuğraş2(İD), Yıldız Camcıoğlu2(İD), Halit Çam1(İD) 1 Department of Pediatric Intensive Care, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey 2 Department of Pediatric Infectious Diseases, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey Cite this article as: Aygün F, Durak C, Varol F, Çokuğraş H, Camcıoğlu Y, Çam H. Evaluation of complete blood count parameters for diagnosis in children with sepsis in the pediatric intensive care unit. J Pediatr Inf 2020;14(2):e55-e62. Abstract Öz Objective: Early diagnosis of sepsis is important for effective treatment Giriş: Erken tanı sepsiste etkili tedavi ve iyi prognoz için önemlidir. C-re- and improved prognosis. C-reactive protein (CRP) and procalcitonin aktif protein (CRP) ve prokalsitonin (PKT) sepsiste en sık kullanılan bi- (PCT) are the most commonly used biomarkers for sepsis. However, their yobelirteçlerdir. Fakat rutinde kullanımı maliyet etkin değildir. Tam kan routine usage is not cost-effective. Complete Blood Count (CBC) param- sayımı (TKS) parametrelerinden eritrosit dağılım genişliği (EDG), nötrofil eters including red cell distribution width (RDW), neutrophil to lympho- lenfosit oranı (NLO), trombosit lenfosit oranı (TLO), ortalama trombosit cyte ratios (NLR), platelet to lymphocyte ratios (PLR), mean platelet vol- hacmi (OTH) basit ve kolay olarak hesaplanmaktadır. Bu çalışmanın ama- ume (MPV), and hemoglobin are simple and easily calculated. -

A Phase Ib Study Evaluating Cobimetinib Plus
Official Title: A Phase Ib Study Evaluating Cobimetinib Plus Atezolizumab in Patients With Advanced BRAF V600 Wild-Type Melanoma Who Have Progressed During or After Treatment With Anti−PD-1 Therapy and Atezolizumab Monotherapy in Patients With Previously Untreated Advanced BRAF V600 Wild-Type Melanoma NCT Number: NCT03178851 Document Date: Protocol Version 5: 26-October-2018 PROTOCOL TITLE: A PHASE IB STUDY EVALUATING COBIMETINIB PLUS ATEZOLIZUMAB IN PATIENTS WITH V600 ADVANCED BRAF WILD-TYPE MELANOMA WHO HAVE PROGRESSED DURING OR AFTER TREATMENT WITH ANTI−PD-1 THERAPY AND ATEZOLIZUMAB MONOTHERAPY IN PATIENTS WITH PREVIOUSLY UNTREATED ADVANCED V600 BRAF WILD-TYPE MELANOMA PROTOCOL NUMBER: CO39721 VERSION NUMBER: 5 EUDRACT NUMBER: 2016-004402-34 IND NUMBER: 135,717 TEST PRODUCTS: Cobimetinib (RO5514041) Atezolizumab (RO5541267) MEDICAL MONITOR: M.D. SPONSOR: F. Hoffmann-La Roche Ltd DATE FINAL: 14 December 2016 DATES AMENDED: Version 2: 23 June 2017 Version 3: 19 September 2017 Version 4: 3 February 2018 Version 5: See electronic date stamp below. PROTOCOL AMENDMENT APPROVAL Approver's Name Title Date and Time (UTC) Company Signatory 26-Oct-2018 10:19:14 CONFIDENTIAL This clinical study is being sponsored globally by F. Hoffmann-La Roche Ltd of Basel, Switzerland. However, it may be implemented in individual countries by Roche’s local affiliates, including Genentech, Inc. in the United States. The information contained in this document, especially any unpublished data, is the property of F. Hoffmann-La Roche Ltd (or under its control) and therefore is provided to you in confidence as an investigator, potential investigator, or consultant, for review by you, your staff, and an applicable Ethics Committee or Institutional Review Board. -

Interpretation of the Leukocytes Picture
15/02/1441 Prof. www.scholaridea.comM. YouTube/ Scholar Idea Complete bloodRushdi count 1 www.scholaridea.com2 YouTube/ Scholar Idea 15/02/1441 Types of blood sample Prof.Whole blood Plasma Serum Blood smear www.scholaridea.com3 M. YouTube/ Scholar Idea Rushdi The White blood cells (RBCs) Leucocytes or white blood cells are divided into two main categories: 1.Polymorphonuclear (PMN) leucocytes (granulocytes): Neutrophils, Eosinophils and Basophils (Produced in the bone marrow). 2.Mononuclear leucocytes (agranulocytes): Lymphocytes and Monocytes. 2 www.scholaridea.com4 YouTube/ Scholar Idea 15/02/1441 Granulocytes A. Neutrophils Prof.The 1st line of cellular defense Phagocytosis Band cell Engulf pyogenic bacteria Elaborate powerful proteolytic enzymes www.scholaridea.comM. YouTube/ Scholar Idea PHAGOCYTOSISRushdi A. Chemotaxis ----Lymphokines B. Opsonization C. Ingestion D. Digestion 3 www.scholaridea.com YouTube/ Scholar Idea 15/02/1441 Granulocytes b. Eosinophils Detoxification of protein breaks Neutralize Histamine Prof.down products substances Destroy larval stage of parasite in tissues www.scholaridea.comM. YouTube/ Scholar Idea RushdiGranulocytes C. Basophils Release histamine Release heparin – Stimulate lipoprotein lipase – clearance of Lipemia 4 www.scholaridea.com YouTube/ Scholar Idea 15/02/1441 A. Lymphocytes Agranulocytes Large lymphocyte Prof.Lymphocyte www.scholaridea.comM. YouTube/ Scholar Idea Agranulocytes B. MonocytesRushdi 1- Phagocytosis 2- increase in chronic inflammation and tissue necrosis 5 www.scholaridea.com YouTube/ Scholar Idea 15/02/1441 PARAMETERS OF LEUCOCYTES PICTURE Prof.Total WBCs count Differential LC Hemocytometer Blood film Blood Cell Counter Blood Cell Counter www.scholaridea.comM. YouTube/ Scholar Idea The significanceRushdi of blood smear examination 1. Identification of different animal species. Some animal species can be identified by examination of a blood smear, for example blood cells of camel are oval, the blood cells of equines are rounded and form a network, the blood cells of birds are oval and nucleated. -

Complete Blood Count in Primary Care
Complete Blood Count in Primary Care bpac nz better medicine Editorial Team bpacnz Tony Fraser 10 George Street Professor Murray Tilyard PO Box 6032, Dunedin Clinical Advisory Group phone 03 477 5418 Dr Dave Colquhoun Michele Cray free fax 0800 bpac nz Dr Rosemary Ikram www.bpac.org.nz Dr Peter Jensen Dr Cam Kyle Dr Chris Leathart Dr Lynn McBain Associate Professor Jim Reid Dr David Reith Professor Murray Tilyard Programme Development Team Noni Allison Rachael Clarke Rebecca Didham Terry Ehau Peter Ellison Dr Malcolm Kendall-Smith Dr Anne Marie Tangney Dr Trevor Walker Dr Sharyn Willis Dave Woods Report Development Team Justine Broadley Todd Gillies Lana Johnson Web Gordon Smith Design Michael Crawford Management and Administration Kaye Baldwin Tony Fraser Kyla Letman Professor Murray Tilyard Distribution Zane Lindon Lyn Thomlinson Colleen Witchall All information is intended for use by competent health care professionals and should be utilised in conjunction with © May 2008 pertinent clinical data. Contents Key points/purpose 2 Introduction 2 Background ▪ Haematopoiesis - Cell development 3 ▪ Limitations of reference ranges for the CBC 4 ▪ Borderline abnormal results must be interpreted in clinical context 4 ▪ History and clinical examination 4 White Cells ▪ Neutrophils 5 ▪ Lymphocytes 9 ▪ Monocytes 11 ▪ Basophils 12 ▪ Eosinophils 12 ▪ Platelets 13 Haemoglobin and red cell indices ▪ Low haemoglobin 15 ▪ Microcytic anaemia 15 ▪ Normocytic anaemia 16 ▪ Macrocytic anaemia 17 ▪ High haemoglobin 17 ▪ Other red cell indices 18 Summary Table 19 Glossary 20 This resource is a consensus document, developed with haematology and general practice input. We would like to thank: Dr Liam Fernyhough, Haematologist, Canterbury Health Laboratories Dr Chris Leathart, GP, Christchurch Dr Edward Theakston, Haematologist, Diagnostic Medlab Ltd We would like to acknowledge their advice, expertise and valuable feedback on this document. -
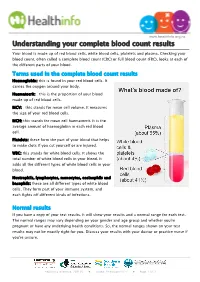
Understanding Your Complete Blood Count Results
www.healthinfo.org.nz Understanding your complete blood count results Your blood is made up of red blood cells, white blood cells, platelets and plasma. Checking your blood count, often called a complete blood count (CBC) or full blood count (FBC), looks at each of the different parts of your blood. Terms used in the complete blood count results Haemoglobin: this is found in your red blood cells. It carries the oxygen around your body. Haematocrit: this is the proportion of your blood made up of red blood cells. MCV: this stands for mean cell volume. It measures the size of your red blood cells. MCH: this stands for mean cell haematocrit. It is the average amount of haemoglobin in each red blood cell. Platelets: these form the part of your blood that helps to make clots if you cut yourself or are injured. WBC: this stands for white blood cells. It shows the total number of white blood cells in your blood. It adds all the different types of white blood cells in your blood. Neutrophils, lymphocytes, monocytes, eosinophils and basophils: these are all different types of white blood cells. They form part of your immune system, and each fights off different kinds of infections. Normal results If you have a copy of your test results, it will show your results and a normal range for each test. The normal ranges may vary depending on your gender and age group and whether you're pregnant or have any underlying health conditions. So, the normal ranges shown on your test results may not be exactly right for you. -
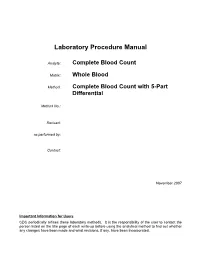
Laboratory Procedure Manual
Laboratory Procedure Manual Analyte: Complete Blood Count Matrix: Whole Blood Method: Complete Blood Count with 5-Part Differential Method No.: Revised: as performed by: Contact: November 2007 Important Information for Users CDC periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. Complete Blood Count (CBC) with Five-Part Differential NHANES 2005–2006 Public Release Data Set Information This document details the Lab Protocol for testing the items listed in the following table: Lab Number Analyte SAS Label LBXWBCSI White blood cell count (SI) LBXLYPCT Lymphocyte (%) LBXMOPCT Monocyte (%) LBXNEPCT Segmented neutrophils (%) LBXEOPCT Eosinophils (%) LBXBAPCT Basophils (%) LBDLYMNO Lymphocyte number LBDMONO Monocyte number LBDNENO Segmented neutrophils number LBDEONO Eosinophils number CBC_d LBDBANO Basophils number LBXRBCSI Red cell count SI LBXHGB Hemoglobin (g/dL) LBXHCT Hematocrit (%) LBXMCVSI Mean cell volume (fL) LBXMCHSI Mean cell hemoglobin (pg) LBXMC MCHC (g/dL) LBXRDW Red cell distribution width (%) LBXPLTSI Platelet count (%) SI LBXMPSI Mean platelet volume (fL) Page 2 of 32 Complete Blood Count (CBC) with Five-Part Differential NHANES 2005–2006 1. Clinical Relevance and Summary of Test Principle Perform a complete blood count (CBC) in duplicate on all Sample Persons (SPs) age 1 and older. Perform the CBC on the Beckman Coulter MAXM. Run a CBC on home exam SP’s EDTA blood tubes after returning to the MEC. A. Purpose and Principle of Test The Beckman Coulter method of sizing and counting particles uses measurable changes in electrical resistance produced by nonconductive particles suspended in an electrolyte. -

Top 5 Leukogram Patterns
TOP 5 > DIAGNOSTICS > PEER REVIEWED Top 5 Leukogram Patterns Sarah Schmidt, DVM, DACVP (Clinical Pathology)* Ashland, Massachusetts A CBC is often completed as part of the minimum database. When the CBC is per- formed with an in-house hematology analyzer, a blood smear evaluation should be pursued as well to verify automated results, including confirmation of white blood cell (WBC) differential and evaluation for atypical cells, such as mast cells, blasts, and nucleated red blood cells. Following confirmation of automated results, evaluation of the leukogram, which includes total WBC count, absolute values of individual leuko- cytes, and leukocyte morphology, should be performed to identify any pattern. When evaluating WBC differentials, absolute cell numbers (WBC count × leukocyte %) should be interpreted as opposed to leukocyte percentage only. 1 Stress Leukogram A stress leukogram is characterized by neutrophilia, lymphopenia, eosinope- nia, and potentially monocytosis.1 It occurs primarily in dogs. The term stress denotes the presence of increased cortisol released from the adrenal gland secondary to severe Top 5 Leukogram Patterns disease (eg, diabetic ketoacidosis, renal failure), high body temperature, pain, dehydra- tion, or hyperadrenocorticism.1 1. Stress Leukogram 2. Inflammatory Leukogram n Neutrophilia occurs because of increased release of mature neutrophils from the bone marrow storage pool to circulating blood and decreased movement of neutro- 3. Persistent Lymphocytosis phils from circulating blood to tissue. (of Mature Lymphocytes) n Lymphopenia results from retention of lymphocytes in lymphoid organs and lym- 4. Neutropenia phocyte lysis. 5. Eosinophilia n Eosinopenia is caused by decreased release of eosinophils from the bone marrow and increased lysis. n Lymphopenia is the hallmark of a stress leukogram. -

In Asymptomatic Term Newborns at Risk for Sepsis, Is a Six-Hour CBC a Better Predictor of Sepsis Than a One-Hour CBC?
In asymptomatic term newborns at risk for sepsis, is a six-hour CBC a better predictor of sepsis than a one-hour CBC? Tori Treloar, R.N., B.S.N; Betsy Finley, R.N., B.S.N., M.P.H.; Audrey Nugent, R.N., B.S.N.; Lucy Schoemer, R.N., M.S.N.; Minshan Coudert, R.N., B.S.N. Background Neonatal sepsis is an invasive infection and remains one of the leading causes of Implications for Practice morbidity and mortality among both term and preterm infants (Shah, Padbury, 2014). The evidence is consistent in that well appearing The current practice at Inova Fairfax Medical Campus is to obtain a complete blood neonates at risk for sepsis should not receive a count (CBC) at one hour and again at 12 hours of life on all newborns at risk for sepsis. complete blood count (CBC) until at least six hours At one hour of life, there is normal decreased perfusion to limbs making it difficult to of life. Values obtained at or after six hours are obtain viable blood sample from a newborn. Multiple venous punctures are often more clinically useful as compared to those utilized to obtain the sample which can be distressing to parents and their newborns. obtained immediately after birth. New practice guidelines from CDC and the American Academy of Pediatrics (AAP) The evidence reviewed is consistent across all of support a CBC to be performed at 6-12 hours of life for low-risk, well-appearing the research and provides a compelling indication infants (Merck Manual, 2019).