Multifocal Iols Mix and Match
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
1. Cause List of Cases Filed Between 01.01.2018 to 21.03.2020 Shall Not Be Published Till Further Orders
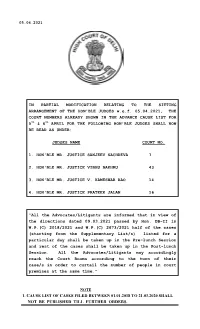
05.04.2021 IN PARTIAL MODIFICATION RELATING TO THE SITTING ARRANGEMENT OF THE HON'BLE JUDGES w.e.f. 05.04.2021, THE COURT NUMBERS ALREADY SHOWN IN THE ADVANCE CAUSE LIST FOR 5th & 6th APRIL FOR THE FOLLOWING HON'BLE JUDGES SHALL NOW BE READ AS UNDER: JUDGES NAME COURT NO. 1. HON'BLE MR. JUSTICE SANJEEV SACHDEVA 7 2. HON'BLE MR. JUSTICE VIBHU BAKHRU 43 3. HON'BLE MR. JUSTICE V. KAMESWAR RAO 14 4. HON'BLE MR. JUSTICE PRATEEK JALAN 16 “All the Advocates/Litigants are informed that in view of the directions dated 09.03.2021 passed by Hon. DB-II in W.P.(C) 2018/2021 and W.P.(C) 2673/2021 half of the cases (starting from the Supplementary List/s) listed for a particular day shall be taken up in the Pre-lunch Session and rest of the cases shall be taken up in the Post-lunch Session. All the Advocates/Litigants may accordingly reach the Court Rooms according to the turn of their case/s in order to curtail the number of people in court premises at the same time.” NOTE 1. CAUSE LIST OF CASES FILED BETWEEN 01.01.2018 TO 21.03.2020 SHALL NOT BE PUBLISHED TILL FURTHER ORDERS. HIGH COURT OF DELHI: NEW DELHI No. 384/RG/DHC/2020 DATED: 19.3.2021 OFFICE ORDER HON'BLE ADMINISTRATIVE AND GENERAL SUPERVISION COMMITTEE IN ITS MEETING HELD ON 19.03.2021 HAS BEEN PLEASED TO RESOLVE THAT HENCEFORTH THIS COURT SHALL PERMIT HYBRID/VIDEO CONFERENCE HEARING WHERE A REQUEST TO THIS EFFECT IS MADE BY ANY OF THE PARTIES AND/OR THEIR COUNSEL. -
Statement of Unclaimed Dividend Amount Consecutively for 7 Years from Dividend of FY 2010-11, Whose Shares Are to Be Transferred to IEPF Account
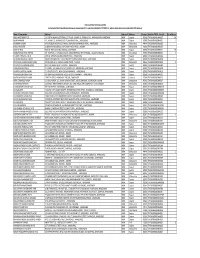
THE ANUP ENGINEERING LIMITED Statement of Unclaimed Dividend amount consecutively for 7 years from Dividend of FY 2010-11, whose shares are to be transferred to IEPF Account Name of Shareholder Address-1 Address-2 Address-3 Pincode Folio No / DP ID - Client ID No. of Shares AEGIS INVESTMENTS LTD C/O.SHETH LALBHAI DALPATBHAI, 1ST FLOOR, 'AKSHAY' 53, SHRIMALI SOC., NAVRANGPURA, AHMEDABAD INDIA Gujarat 380009 THEA0000000000A00179 306 ANJANA MANAN 101, AKSHAY, 53, SHRIMALI SOCIETY, NAVRANGPURA,, , AHMEDABAD INDIA Gujarat 380009 THEA0000000000A00217 11 ARJANBHAI ALABHAI 664 KUBERDAS MODI'S OLD CHAWAL, SAIJPUR BOGHA NARODA ROAD, , AHMEDABAD INDIA Maharashtra 444444 THEA0000000000A00203 1 BAKULA R JHAVERI 10 SEKHSARIA BUILDINGS, 2ND FLOOR, 448 SVP ROAD, , MUMBAI INDIA Maharashtra 400004 THEA0000000000B00168 1 BANK OF INDIA BANK OF INDIA BUILDING, BHADRA, , AHMEDABAD INDIA Gujarat 380001 THEA0000000000B00118 783 BHARATKUMAR SHIVJI SHETHIA 7/1 'TILOTTMA', 1-C PANKAJ MULLICK, SARANI (FORMALY RITCHIE ROAD), , CALCUTTA KOLKATA INDIA West Bengal 700019 THEA0000000000B00138 33 C V MEHTA PRIVATE LIMITED BANK OF BARODA BUILDING, GANDHI ROAD, , AHMEDABAD INDIA Gujarat 380001 THEA0000000000C00068 1 DR ARUNA RAMANLAL JHAVERI RAJAN SHRI NIWAS SOC., SUKHIPURA NEW SHARDA MANDIR ROAD, , AHMEDABAD INDIA Gujarat 380007 THEA0000000000A00086 1 DR JIVANLAL HUKAMCHANDJI PAREKH C/O.DHANRAJ & CO., RESHAM BAZAR ITWARI, , NAGPUR INDIA Maharashtra 444444 THEA0000000000J00051 13 DR SUMATILAL VIRCHAND MODI NO.1 NEW ANJALI SOCIETY, VASANA, , AHMEDABAD INDIA Gujarat 380007 -
Deletion Notes
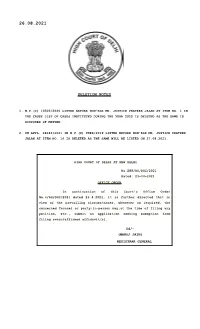
26.08.2021 DELETION NOTES 1. W.P.(C) 10505/2020 LISTED BEFORE HON'BLE MR. JUSTICE PRATEEK JALAN AT ITEM NO. 1 IN THE CAUSE LIST OF CASES INSTITUTED DURING THE YEAR 2020 IS DELETED AS THE SAME IS DISPOSED OF MATTER. 2. CM APPL. 28242/2021 IN W.P.(C) 9986/2019 LISTED BEFORE HON'BLE MR. JUSTICE PRATEEK JALAN AT ITEM NO. 16 IS DELETED AS THE SAME WILL BE LISTED ON 27.08.2021. HIGH COURT OF DELHI AT NEW DELHI No.289/RG/DHC/2021 Dated: 23-04-2021 O FFICE ORD ER In continuation of this Court's Office Order No.4/RG/DHC/2021 dated 23.4.2021, it is further directed that in view of the prevailing circumstances, wherever so required, the concerned Counsel or party-in-person may,at the time of filing any petition, etc., submit an application seeking exemption from filing sworn/affirmed affidavit(s). Sd/- (MANOJ JAIN) REGISTRAR GENERAL As approved by Hon'ble Chairman, DHCLSC, National Lok Adalat is to be held on 11.09.2021(SECOND SATURDAY) at High Court of Delhi for pending cases under following category:- 1. Criminal Compoundable Offence 2. NI Act cases under Section 138; 3. Bank Recovery cases; 4. MACT cases; 5. Labour disputes cases; 6. Electricity and Water Bills[excluding non-compoundable] 7. Matrimonial disputes; 8. Land Acquisition cases; 9. Services matters relating to pay and allowances and retiral benefits; 10. Revenue cases; 11. Other civil cases(rent, easmentary rights, injunction suits, specific performance suits) etc; To facilitate settlements, DHCLSC will conduct on line Pre-Lok Adalat sittings w.e.f. -

The Phonograph in India
The Phonograph in India G. N. Joshi The Beginnings The history of the phonograph in India dates back to the beginning of the century. Though gramophones began to be exported to India since 1 898, the idea of commercially exploiting the phonograph on a large scale in the east was mooted in 1 900 and Messrs. The Mutoscope Biograph Co. of India was given the agency of selling horn-gramophones and records of European music imported from America. In 1 898, Mr. W. B. Owen had established in England the parent company of the Gramophone Co. Ltd. He was sent to England by the American inventor of disc recording, Mr. Emile Berliner, to sell, if possible, his European rights for the disc records which he had patented in the U.S.A. Since Mr. Owen did not succeed in selling Mr. Berliner's rights outright, the two formed The Gramophone Co. Ltd. in England. Mr. Berliner erected a record pressing factory at Hanover in the U.S.A . for supplying records and machines to the newly-formed company in England . At this point a· mechanic named Johnson invented a spring-wound motor for the phonograph machine. Until the time his invention was perfected, users (during the period when the record was being played) had to rotate, with the help of a handle, the turntable with the disc on it. The spring-motor Edison 'Home' Model A enabled the phonograph to be \Nound for a certain number of playings and hence the listener could sit at a distance \Nithout having to bother to crank the machine all the time. -

RÉTROSPECTIVE DU CINÉMA INDIEN POPULAIRE Et
Direction de la communication DOSSIER DE PRESSE VOUS AVEZ DIT BOLLYWOOD ! RÉTROSPECTIVE DU CINÉMA INDIEN POPULAIRE et www.centrepompidou.fr VOUS AVEZ DIT BOLLYWOOD ! RÉTROSPECTIVE DU CINÉMA INDIEN POPULAIRE 4 FEVRIER – 1er MARS 2004 ET 17 MARS – 19 AVRIL 2004 CINEMA 1 (NIVEAU 1), CINEMA 2 (NIVEAU –1) DDirection sommaire de la communication 75 191 Paris cedex 04 responsable du pôle presse I. COMMUNIQUE DE PRESSE page 2 Carole Rio-Latarjet chargée des relations presse Albane Jouis-Maucherat II. VOUS AVEZ DIT « BOLLYWOOD » ! page 4 téléphone par Nadine Tarbouriech 00 33 (0)1 44 78 13 81 télécopie III PROGRAMMATION ET SYNOPSIS DES FILMS page 6 00 33 (0)1 44 78 13 02 mél IV. CALENDRIER DES PROJECTIONS page 29 albane.jouis-maucherat @cnac-gp.fr V. RENCONTRE ORGANISEE PAR LES FORUMS DE SOCIETE La « résistance » de Bollywood ? page 38 VI. EVENEMENTS AUTOUR DE LA MANIFESTATION page 40 VII. LISTE DES PHOTOS DISPONIBLES POUR LA PRESSE page 48 VIII. REMERCIEMENTS page 52 IX. INFORMATIONS PRATIQUES page 53 VOUS AVEZ DIT BOLLYWOOD ! RÉTROSPECTIVE DU CINÉMA INDIEN POPULAIRE 4 FEVRIER – 1er MARS 2004 ET 17 MARS – 19 AVRIL 2004 CINEMA 1 (NIVEAU 1), CINEMA 2 (NIVEAU –1) Direction Pour la première fois en France, une grande rétrospective consacrée à la cinématographie de la communication indienne populaire est proposée par les Cinémas du Centre Pompidou. 75 191 Paris cedex 04 responsable du pôle presse er Carole Rio-Latarjet Pensée en deux temps, la manifestation rend d’abord hommage, du 4 février au 1 mars 2004, chargée des relations presse aux auteurs des grands classiques en noir et blanc des années 50 considérées comme l’âge Albane Jouis-Maucherat d’or des studios indiens : Guru Dutt, Raj Kapoor, Bimal Roy, Mehboob Khan, V. -

Dadasaheb Phalke Awards
Dadasaheb Phalke Awards The Dadasaheb Phalke Awards is the highest award in cinema. It is annually presented at the National Film Awards ceremony by the Directorate of Film Festivals. The award is named after Dhundiraj Govind Phalke, popularly known as Dadasaheb Phalke. Dadasaheb Phalke is regarded as the ‘father of Indian cinema’. In the 2021 edition of the Dadasaheb Phalke Awards Deepika Padukone received the best actress award for her film Chhapaak while Akshay Kumar got the awards for fis performance in the film Laxmi. This article will give details about Dadasaheb Phalke Awards within the context of the IAS Exam Brief facts about Dadasaheb Phalke Ddasheb Phalke was a producer-director-screenwriter who made India’s first feature-length film, Raja Harishchandra in 1913. He made 95 feature-length films and 27 short films in his career, spanning 19 years, until 1937, including his most noted works: Mohini Bhasmasur (1913), Satyavan Savitri (1914), Lanka Dahan (1917), Shri Krishna Janma (1918) and Kaliya Mardan (1919). His contributions to India cinema was legendary and thus was the reason why the Indian government instituted an award in his honour. Recipients of the Dadasaheb Phalke Awards The following table gives the list of winners of the Dadasaheb Phalke Awards through the years Dadasaheb Phalke Awards Recipients (1969-1979) Year Recipient Film Industry 1969 Devika Rani Hindi 1970 Birendranath Sircar Bengali 1971 Prithviraj Kapoor Hindi 1972 Pankaj Mullick ● Hindi ● Bengali 1973 Ruby Myers (Sulochana) Hindi 1974 Bommireddy Narasimha Reddy Telugu 1975 Dhirendra Nath Ganguly Bengali 1976 Kanan Devi Bengali 1977 Nitin Bose Bengali Hindi 1978 Raichand Boral ● Hindi ● Bengali 1979 Sohrab Modi Hindi The following table gives the list of winners from 1980-1989 Dadasaheb Phalke Awards Recipients (1980-1989) Year Recipient Film Industry 1980 Paidi Jairaj ● Hindi ● Telugu 1981 Naushad Hindi 1982 L. -

The C Om Poser
The Newsletter | No.65 | Autumn 2013 10 | The Study Rabindrasangit: uncovering a ‘Bengali secret’ The Composer On 14 November 1913, Rabindranath Tagore (1861-1941) was awarded the Nobel Prize for Literature for Gitanjali – a selection of his Bengali lyrics in English prose, translated by the poet himself, with an ecstatic introduction by W.B. Yeats. Rabindranath was the first Asian to win the prize, and was honoured that year by bypassing one of the English greats: novelist and poet Thomas Hardy. Rituparna Roy Gitanjali and the Nobel Tagore’s prophecy great memory with a song. If the person grew up in a house When Alfred Nobel instituted the prize in 1901, he intended One of his earliest English admirers and biographer, that cultivated Tagore, then the association will be deeper for the committee to discover a new genius for the world E. P. Thompson, in trying to establish Tagore’s impressive and more vital – but even otherwise, there is no getting away every year. But by 1913, Tagore was already a very distinguished fecundity, wrote in 1948: from Tagore. Especially his songs. My own earliest memory figure in his own country – he was the foremost poet and is of my mother singing Rabindrasangit, late into the evening. writer of Bengal; a pioneering educationist who had started Milton’s English verse is less than 18,000 lines. Tagore’s A marble bust of Tagore had pride of place in our living room an experimental educational institution in Shantiniketan; published verse and dramas amount to 15,000 lines or their – it still does! – the only god that my atheist father has lived and a national leader who had given creative leadership in equivalent. -

History of Indian Cinema.Pdf
CHAPTER – 2 A BRIEF HISTORY OF INDIAN CINEMA Indian films are unquestionably the most –seen movies in the world. Not just talking about the billion- strong audiences in India itself, where 12 million people are said to go to the cinema every day, but of large audiences well beyond the Indian subcontinent and the Diaspora, in such unlikely places as Russia, China, the Middle East, the Far East Egypt, Turkey and Africa. People from very different cultural and social worlds have a great love for Indian popular cinema, and many have been Hindi Films fans for over fifty years. Indian cinema is world – famous for the staggering amount of films it produces: the number is constantly on the increase, and recent sources estimate that a total output of some 800 films a year are made in different cities including Madrass , Bangalore , Calcutta and Hyderabad . Of this astonishing number, those films made in Bombay, in a seamless blend of Hindi and Urdu, have the widest distribution within India and Internationally. The two sister languages are spoken in six northern states and understood by over 500 million people on the Indian sub – continent alone – reason enough for Hindi and Urdu to be chosen above the fourteen official Indian languages to become the languages of Indian Popular cinema when sound came to the Indian Silver screen in 1931 . Silent Era – The cinematographe (from where we have the name cinema) invented by the Lumiere brothers functioned better the Kinetoscope of Edison and Dickson. The Lumiere brothers who invented the cinematographe started projection of short (very short, one to two minutes long) films for the Parsian public on November 28, 1895. -

Saregama India Limited India’S Only Entertainment Company Into
India’s Oldest Music Label operating as The Gramophone Company of India Ltd under HMV brand since 1902 Saregama India Limited India’s only Entertainment Company into Music Films IP Television Serials Retail Business India’s Largest Music IP Content IP rights of Content IP rights of Distribution network 130k+ 59 6k+ 28k+ Songs Films Hours of Television Serials Retailers Most POPULAR Indian Music Library Rapidly Growing Consumption (Song Usage across Platforms in billions) FY20 63 FY19 53 FY18 31 FY17 13 Most POPULAR Indian Music Library - ON ACCOUNT OF - Depth of Content Investment in New Music Song Library across 18 Indian languages 30% of Saregama’s songs, by Count and Revenue, belong to the 21st century 2001-2020 31% 34% 17% 25% 1981-20000 31% 27% 3% 5% 1961-1980 26% 34% 5% 6% Till 1960 11% 4% 22% 7% 9% Most POPULAR Indian Music Library 2M+ Units Sold ($100) On back of Saregama Music Library The Only Content For Which Indian Consumers Pay Most POPULAR Indian Music Library OUR LICENSING PARTNERS Music Streaming Platforms Broadcasting Platforms Video Streaming Platforms v v v Social Media Platforms Most EXTENSIVE Indian Music Library 130000+ Songs Covering multiple Indian languages and genres HINDI BENGALI TAMIL MARATHI 38900+ 26600+ 11800+ 6300+ TELUGU MALAYALAM PUNJABI KANNADA 8100+ 7000+ 8400+ 3100+ DEVOTIONAL CLASSICAL Ghazals Folk 18300+ 8400+ 1200+ 4700+ Music In India Debuted with Saregama Gauhar Jaan – 1902 First Recorded Song Gauhar Jaan arrived with her suite of attendants and accompanying musicians on 11thNov, 1902 dressed in her best finery for her recording session with Frederick William Gaisberg, the first recording expert of The Gramophone and Typewriter Limited from London. -

Annual Report-2004-2005
122 Board of Trustees Shri Soli J. Sorabjee, President Dr Kapila Vatsyayan Prof. M.G.K. Menon Smt. Justice (Retd.) Leila Seth Dr L.M. Singhvi Dr R.K. Pachauri Dr Karan Singh Shri P.C. Sen, Director Director Shri P. C. Sen Executive Committee Shri P.C. Sen, Chairman Shri M.P. Wadhawan, Hon. Treasurer Smt. Rajni Kumar Shri Inder Malhotra Cmdre C. Uday Bhaskar Dr Arvind Pandalai Shri Vipin Malik Cmdre K.N. Venugopal, Secretary Dr S.M. Dewan Finance Committee Dr L.M. Singhvi Shri M.P. Wadhawan Shri Inder Malhotra Cmdre (Retd.) K.N. Venugopal Dr E.A.S. Sarma Shri P.R. Sivasubramanian Shri P.C. Sen Medical Consultants Dr K. P. Mathur Dr (Mrs.) Rita Mohan Dr K. A. Ramachandran Dr B. Chakravorty Dr Mohammad Qasim Senior Staff Cmdre (Retd.) K. N. Venugopal Secretary Shri L. K. Joshi Chief General Manager Shri P. R. Sivasubramanian Chief Finance Officer Dr H. K. Kaul Chief Librarian Dr Geeti Sen Chief Editor Dr A. C. Katoch Administration Officer Ms Premola Ghose Chief, Programme Division Shri Arun Potdar Chief, Maintenance Division Shri W. R. Sehgal Accounts Officer 120 2005-2006 THIS IS THE 45th Annual Report of the India International Centre for the year commencing the 1st of February 2005 to the 31st of January 2006. It will be placed before the 50th Annual General Body Meeting of the Centre, to be held on the 31st of March 2006. Elections to the Executive Committee and the Board of Trustees of the Centre for the two year period 2005-07 were initiated in the latter half of 2004. -

Iphd 2012 Applicant List Selected WEB Version
Admission - 2012 Integrated PhD Programme - List of Selected Interviewees Reporting Time: 09:00 AM Interview Time: 10:00 AM onwards SL. INTERVIEW ID STUDENT PARENT UNIVERSITY (BSc) INSTITUTE (BSc) NO. DATE BANWARILAL BHALOTIA 1 I-26 BAISHALI DUTTA SRIKANTA DUTTA THE UNIVERSITY OF BURDWAN 11.06.2012 COLLEGE UNIVERSITY OF DELHI NEW 2 I-41 BHAVYA TIWARI SHIV SHANKER TIWARI GARGI COLLEGE NEW DELHI 11.06.2012 DELHI 3 I-45 MANAOJ ARAVIND V T K VIVEKANANDAN UNIVERSITY OF MADRAS LOYOLA COLLEGE 11.06.2012 4 I-48 SUCHETA MAJUMDAR REKHA MAJUMDAR UNIVERSITY OF CALCUTTA LADY BRABOURNE COLLEGE 11.06.2012 5 I-53 AMARTYA DUTTA AVIJIT DUTT CALCUTTA UNIVERSITY SCOTTISH CHURCH COLLEGE 11.06.2012 6 I-59 KIMBERLY HSIEH SUI MEE HSIEH KUO CHUNG CALCUTTA UNIVERSITY ST. XAVIER'S COLLEGE, KOLKATA 11.06.2012 7 I-67 SHAMREEN IRAM MD BADRUL ALAM CU 11.06.2012 RAMAKRISHNA MISSION 8 I-71 ANTU LAHA PRASANTA LAHA UNIVERSITY OF CALCUTTA RESIDENTIAL COLLEGE, 11.06.2012 NARENDRAPUR RAMAKRISHNA MISSION 9 I-73 ABHISEK SAMANTA RABINDRANATH SAMANTA UNIVERSITY OF CALCUTTA RESIDENTIAL COLLEGE, 11.06.2012 NARENDRAPUR 10 I-81 DEEPANKAR GUPTA SATISH CHANDRA GUPTA DELHI UNIVERSITY HINDU COLLEGE 11.06.2012 11 I-110 MANIBRATA SEN TAPAS SEN CALCUTTA UNIVERSITY ST.XAVIER'S COLLEGE, KOLKATA 11.06.2012 12 I-124 PRATIK MULLICK PANKAJ MULLICK CALCUTTA UNIVERSITY ST. XAVIER'S COLLEGE 11.06.2012 SUBHAM DUTTA PARTHA SARATHI DUTTA 13 I-139 UNIVERSITY OF CALCUTTA ST. XAVIER'S COLLEGE, KOLKATA 11.06.2012 CHOWDHURY CHOWDHURY 14 I-148 MD ARIF SHAIKH JYOTSNA BEWA --- --- 11.06.2012 Page 1 Admission - 2012 Integrated PhD Programme - List of Selected Interviewees Reporting Time: 09:00 AM Interview Time: 10:00 AM onwards SL. -

Indian Awards
BANK GK FACT FILES Indian Awards Dadasaheb Phalke Awards Sr.No Year Winner Role of Winner 1 2013 Gulzar Lyricist 2 2012 Pran Actor 3 2011 Soumitra Chatterjee Actor 4 2010 K. Balachander Director 5 2009 D. Ramanaidu Producer, Director 6 2008 V. K. Murthy Cinematographer 7 2007 Manna Dey Playback singer 8 2006 Tapan Sinha Director 9 2005 Shyam Benegal Director 10 2004 Adoor Gopalakrishnan Director 11 2003 Mrinal Sen Director 12 2002 Dev Anand Actor, Director, Producer 13 2001 Yash Chopra Director, Producer 14 2000 Asha Bhosle Playback singer 15 1999 Hrishikesh Mukherjee Director 16 1998 B. R. Chopra Director, Producer 17 1997 Pradeep Lyricist 18 1996 Sivaji Ganesan Actor 19 1995 Rajkumar Actor, Singer 20 1994 Dilip Kumar Actor 21 1993 Majrooh Sultanpuri Lyricist Musician, singer, poet, filmmaker, 22 1992 Bhupen Hazarika lyricist 23 1991 Bhalji Pendharkar Director, Producer, Screenwriter 24 1990 Akkineni Nageswara Rao Actor 25 1989 Lata Mangeshkar Playback singer 26 1988 Ashok Kumar Actor 27 1987 Raj Kapoor Actor, Director, Producer 28 1986 Bommireddy Nagi Reddy Producer 29 1985 V. Shantaram Actor, Director, Producer 30 1984 Satyajit Ray Director 31 1983 Durga Khote Actress 32 1982 L. V. Prasad Actor, Director, Producer 33 1981 Naushad Music Director 34 1980 Paidi Jairaj Actor, Director 35 1979 Sohrab Modi Actor, Director, Producer 36 1978 Raichand Boral Music Director, Director 37 1977 Nitin Bose Cinematographer, Director,Screenwriter 38 1976 Kanan Devi Actress B-GK-FF 1 © www.TestFunda.com BANK GK FACT FILES Sr.No Year Winner Role of Winner 39 1975 Dhirendranath Ganguly Actor, Director 40 1974 Bommireddy Narasimha Reddy Director 41 1973 Ruby Myers (Sulochana) Actress 42 1972 Pankaj Mullick Music Director 43 1971 Prithviraj Kapoor Actor 44 1970 B.