Oxygen Devices and Delivery Systems
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2018 Full Line Catalog Products to Support Dive Shop Operations Table of Contents
2018 FULL LINE CATALOG PRODUCTS TO SUPPORT DIVE SHOP OPERATIONS TABLE OF CONTENTS 3 6 8 TEST EQUIPMENT REGULATOR SERVICE & Flowbenches, ACCESSORIES MAINTENANCE workstations, test Regulator, BC and Tools, O-rings, chambers and other console hoses, chemicals and products used in swivels, adapters and equipment used testing regulators, dive related items. for the service and computers and other maintenance of dive related items. regulators, tanks and other dive equipment. 15 17 19 AIR FILTRATION COMPRESSORS TANK FILLING Filters, towers, bulk Small to medium Whips, fill filter chemicals sized breathing attachments and and related control air compressors, adapters for filling hardware for compressor oils and SCUBA, DIN, SCBA breathing air filtration related accessories. and many other tank/ systems. valve styles. 22 28 30 COMPRESSED GAS PAINTBALL MIXED GAS / HARDWARE Whips, adapters and NITROX / OXYGEN Air station hardware, accessories for filling Hardware, chemicals regulators, valves and servicing paint and tools used and fittings for ball tanks and related for the creation, the storage and equipment. handling and analysis distributions of High of mixed gas, Nitrox Pressure Air. and Oxygen. SALES INFORMATION [email protected] 512.240.6644 • 800.558.1811 voice • 512.240.6645 fax MAILING ADDRESS 4674 Priem Lane, Suite 402 • Pflugerville, TX 78660 ANY AND ALL INFORMATION SUBJECT TO CHANGE WITHOUT NOTICE. ALL RIGHTS RESERVED. www.global-mfg.com 2 | TABLE OF CONTENTS TEST EQUIPMENT and stability, and systemic air rubber cup adapter which 48250 Compact Deluxe FLOWBENCHES tightness. Air flow rates through replaces the mouthpiece. First Flowbench with Double tank valves or gas manifolds stage intermediate pressure is Magnehelic Our top-of-the-line analyzer is can also be determined. -

Frequently Asked Questions (Faqs)
Frequently Asked Questions (FAQs) What is hyperbaric oxygen therapy? Commonly referred to as HBOT, hyperbaric oxygen therapy enhances the body’s natural healing process by delivering oxygen under pressure, which increases the oxygen content in the blood, plasma, cerebral spinal fluid, and other body tissues. There are two basic types of HBOT—hard HBOT and mild HBOT. With hard HBOT, treatments are delivered in a hard-sided chamber typically at pressures greater than 1.5 ATA and using 100% oxygen. 100% oxygen is extremely flammable; therefore, hard HBOT involves managing the risk of explosion. Another concern with hard HBOT is oxygen toxicity. While hard HBOT with 100% oxygen results in greater oxygen saturation in the tissues, many conditions respond better to mild HBOT. In clinical trials to date, there has been virtually no difference in clinical outcome between mild HBOT and hard HBOT. Mild HBOT refers to hyperbaric oxygen therapy at lower pressures, typically 1.5 ATA or below, and the use of an oxygen concentrator delivering 90-95% oxygen inside a portable soft-sided chamber. Mild HBOT has no known safety risks with fire or toxicity, and it is substantially less expensive. Our facility provides concentrated oxygen (90-95%) at 1.3 ATA—(Mild HBOT)a highly effective combination clinically, and without the risk of oxygen toxicity or explosion, as 100% oxygen is avoided. How should I expect mild HBOT to feel? You will be seated or lying down inside the chamber, relaxing comfortably in your own clothing, as you breathe concentrated oxygen (90-95% O2) through a facemask. -
Stratus 5 Oxygen Concentrator User Manual
USER MANUAL OXYGEN CONCENTRATOR CE 0123 v2.1 STR1005 User Manual Symbol Key MARK DEFINITION II Power on Power off Follow Instruction for Use No smoking Caution, consult accompanying documents. Class Ⅱ (Double Insulated) Type BF Applied Part CE certification mark 0123 AC Power Stacking Limit by Number This Way Up Fragile, handle with care Keep dry Temperature limit No open flames IIPP2211 IP21 Drip Proof Equipment Consult instructions for use Stand-by Warning, electricity 2 v2.1 STR1005 User Manual 3 v2.1 STR1005 User Manual SPECIAL NOTES • Please read this manual carefully before using this product and save it for future reference. • If you need assistance with this manual, Please contact your local DME or home health provider • The Stratus 5 is a prescription device. Use only the liter setting prescribed for you. • It is always recommended for critically ill patients to have a backup oxygen source in case of malfunction. • If patient experiences an adverse reaction contact physician or call 911 immediately. • In case of machine malfunction, contact the home medical equipment provider; do not attempt to disassemble the Stratus 5. • The Stratus 5 is not intended as life support, it is for supplemental oxygen use only. Patients with special needs may be unable to understand the alarm features and should be well supervised while using an oxygen concentrator. • The Stratus 5 is for single patient use. • Do not adjust the flowmeter float beyond the red line position. Long-term use out of range will reduce the efficiency of the oxygen generator. SAFETY NOTICE Please read the following information carefully before Operating the oxygen concentrator Warning Special attention should be paid to reducing the risk of fire when using oxygen therapy. -

Subchapter V—Marine Occupational Safety and Health Standards
SUBCHAPTER V—MARINE OCCUPATIONAL SAFETY AND HEALTH STANDARDS PART 197—GENERAL PROVISIONS 197.456 Breathing supply hoses. 197.458 Gages and timekeeping devices. 197.460 Diving equipment. Subpart A [Reserved] 197.462 Pressure vessels and pressure piping. Subpart B—Commercial Diving Operations RECORDS GENERAL 197.480 Logbooks. 197.482 Logbook entries. Sec. 197.484 Notice of casualty. 197.200 Purpose of subpart. 197.486 Written report of casualty. 197.202 Applicability. 197.488 Retention of records after casualty. 197.203 Right of appeal. 197.204 Definitions. Subpart C—Benzene 197.205 Availability of standards. 197.206 Substitutes for required equipment, 197.501 Applicability. materials, apparatus, arrangements, pro- 197.505 Definitions. cedures, or tests. 197.510 Incorporation by reference. 197.208 Designation of person-in-charge. 197.515 Permissible exposure limits (PELs). 197.210 Designation of diving supervisor. 197.520 Performance standard. 197.525 Responsibility of the person in EQUIPMENT charge. 197.300 Applicability. 197.530 Persons other than employees. 197.310 Air compressor system. 197.535 Regulated areas. 197.312 Breathing supply hoses. 197.540 Determination of personal exposure. 197.314 First aid and treatment equipment. 197.545 Program to reduce personal expo- 197.318 Gages and timekeeping devices. sure. 197.320 Diving ladder and stage. 197.550 Respiratory protection. 197.322 Surface-supplied helmets and masks. 197.555 Personal protective clothing and 197.324 Diver’s safety harness. equipment. 197.326 Oxygen safety. 197.560 Medical surveillance. 197.328 PVHO—General. 197.565 Notifying personnel of benzene haz- 197.330 PVHO—Closed bells. ards. 197.332 PVHO—Decompression chambers. -

Rebreathers Open Inspiration Fully Closed Rebreather What Is It Like? Text & Photos by Peter Symes Diving Rebreathers Why Bother?
WWW.AQUALUNG.COM Dräger Ray semiclosed rebreather. Behind, an Rebreathers open Inspiration fully closed rebreather What is it like? WWW.AMBIENTPRESSUREDIVING.COM Text & photos by Peter Symes Diving Rebreathers Why bother? Rebreathers look cool, glitzy, tech- they provide for a much differ- nical and heralded as the future of ent and richer diving experience, which, in the first place, is why we go in diving, right? We read a lot about the water ourselves rather than watch- their impressive performances con- ing dive movies on Animal Planet from cerning duration of dives, gas econ- the comfort of our reclining chair at home. omy, extended no deco limits and However, as we all know, there is no such thing as a free lunch in diving either. There is what not. But isn’t it a bit like watch- a trade-off, and you will have to consider if it the underwater realm so you can have an ing Jeremy Clarkson from BBC’s car is still worth your while despite this. enriching experience by witnessing, first program, Top Gear, whiz around in It is not merely a matter of comparing hand, this magic realm. So, as far as I am fancy Ferraris and Aston Martins with technical matters, performance and param- concerned, if someone invented human eters when pitting rebreathers against the gills and a thin hide to cover and keep me a goofy, happy grin on his face and open circuits (regulators and tanks). It is warm, my twin-set would surely be left to rust reeling off a string of excited super- easy to be blinded by dazzling numbers and in the attic for good. -

Compressed Gas Cylinder Procedure for Scuba Diving
The University of Maine DigitalCommons@UMaine General University of Maine Publications University of Maine Publications 5-20-2019 Compressed Gas Cylinder Procedure for Scuba Diving University of Maine System Follow this and additional works at: https://digitalcommons.library.umaine.edu/univ_publications Part of the Higher Education Commons, and the History Commons Repository Citation University of Maine System, "Compressed Gas Cylinder Procedure for Scuba Diving" (2019). General University of Maine Publications. 837. https://digitalcommons.library.umaine.edu/univ_publications/837 This Other is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in General University of Maine Publications by an authorized administrator of DigitalCommons@UMaine. For more information, please contact [email protected]. Campus: The University of Maine System / Safety Management Page 1 of 15 Document: Compressed Gas Cylinder Procedure for Scuba Diving 0507425, 05/20/19 Compressed Gas Cylinder Procedure for Scuba Diving TABLE OF CONTENTS Title Page Purpose and Background ..................................................................................................................... 2 Regulatory Guidance .................................................................................................................... 2 Requirements ................................................................................................................................. 2 Responsibilities ............................................................................................................................. -
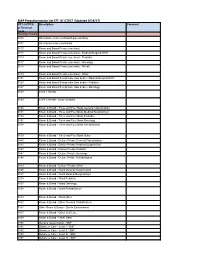
MAP Preauthorization List EFF: 8/1/2017 (Updated 8/24/17)
MAP Preauthorization List EFF: 8/1/2017 (Updated 8/24/17) CPT, HCPCS Description Comment or Revenue Code Revenue Codes 0100 All inclusive room and board plus ancillary 0101 All inclusive room and board 0110 Room and Board Private (one bed) 0111 Room and Board Private (one bed) - Medical/Surgical/GYN 0113 Room and Board Private (one bed) - Pediatric 0117 Room and Board Private (one bed) - Oncology 0118 Room and Board Private (one bed) - Rehab 0119 Room and Board Private (one bed) - Other 0121 Room and Board Semiprivate (two beds) - Medical/Surgical/GYN 0123 Room and Board Semiprivate (two beds) - Pediatric 0127 Room and Board Semiprivate (two beds) - Oncology 0128 Level 1 Rehab 0129 Level 2 Rehab - acute complex 0130 Room & Board - Three and Four Beds General Classification 0131 Room & Board - Three and Four Beds Medical/Surgical/Gyn 0133 Room & Board - Three and Four Beds Pediatric 0137 Room & Board - Three and Four Beds Oncology 0138 Room & Board - Three and Four Beds Rehabilitation 0139 Room & Board - Three and Four Beds Other 0140 Room & Board - Deluxe Private General Classification 0141 Room & Board - Deluxe Private Medical/Surgical/Gyn 0143 Room & Board - Deluxe Private Pediatric 0147 Room & Board - Deluxe Private Oncology 0148 Room & Board - Deluxe Private Rehabilitation 0149 Room & Board - Deluxe Private Other 0150 Room & Board - Ward General Classification 0151 Room & Board - Ward Medical/Surgical/Gyn 0153 Room & Board - Ward Pediatric 0157 Room & Board - Ward Oncology 0158 Room & Board - Ward Rehabilitation 0159 Room & Board - -

Airgas Booklet
AIR-233-doc 11/7/03 9:45 AM Page 1 SafetySafety BookletBooklet You’ll find it with us. Airgas, Inc. 259 North Radnor-Chester Road Suite 100 Radnor, PA 19087-5283 (610) 687-5253 FAX: (610) 687-1052 For the Safe Handling 800-255-2165 www.airgas.com and Transportation of Compressed Gases © 2003 Airgas, Inc. MCM-0XX 11/03 AIR-233-doc 11/7/03 9:45 AM Page 3 TThings you should know before handling or HHandling Compressed Gases transporting compressed gas cylinders. Compressed gases are capable of creating environ- Did you know that all compressed gases are labeled ments that are explosive, reactive, flammable, hazardous materials simply because they’re under oxidizing, oxygen deficient, extremely cold, corrosive pressure? Many gases are also considered hazardous or otherwise extremely hazardous to health, depend- materials because of the properties of the gas con- ing upon the product contained in the cylinder. tained in the cylinder. Since all compressed gases are classified as a hazardous material, specific training on Most compressed gas cylinders are very heavy, and federal and state regulations covering the safe han- remain so whether they are empty or full, as their dling and transportation of compressed gases should contents are in gaseous form and weigh very little. be provided to you by your manager or employer Cylinders containing product in liquid form are before you ever touch a compressed gas cylinder. You extremely heavy when full, but less so when empty. should also receive training by your manager or Acetylene cylinders are designed with a heavy filler employer concerning the nature and properties of any material in addition to the gas product itself. -

Summary of Gas Cylinder and Permeation Tube Standard Reference Materials Issued by the National Bureau of Standards
A111D3 TTbS?? o z C/J NBS SPECIAL PUBLICATION 260-108 o ^EAU U.S. DEPARTMENT OF COMMERCE/National Bureau of Standards Standard Reference Materials: Summary of Gas Cylinder and Permeation Tube Standard Reference Materials Issued by the National Bureau of Standards QC 100 U57 R. Mavrodineanu and T. E. Gills 260-108 1987 m he National Bureau of Standards' was established by an act of Congress on March 3, 1901. The Bureau's overall goal i s t0 strengthen and advance the nation's science and technology and facilitate their effective application for public benefit. To this end, the Bureau conducts research to assure international competitiveness and leadership of U.S. industry, science arid technology. NBS work involves development and transfer of measurements, standards and related science and technology, in support of continually improving U.S. productivity, product quality and reliability, innovation and underlying science and engineering. The Bureau's technical work is performed by the National Measurement Laboratory, the National Engineering Laboratory, the Institute for Computer Sciences and Technology, and the Institute for Materials Science and Engineering. The National Measurement Laboratory Provides the national system of physical and chemical measurement; • Basic Standards 2 coordinates the system with measurement systems of other nations and • Radiation Research furnishes essential services leading to accurate and uniform physical and • Chemical Physics chemical measurement throughout the Nation's scientific community, • Analytical Chemistry industry, and commerce; provides advisory and research services to other Government agencies; conducts physical and chemical research; develops, produces, and distributes Standard Reference Materials; provides calibration services; and manages the National Standard Reference Data System. -
Compressed Gas Cylinder Training
Compressed Gas Cylinder Training PFW ANNUAL TRAINING Overview of Training Description of compressed gas cylinders How compressed gas cylinders are used Potential hazards of compressed gas cylinders Best practices for storage, transport, and use Description of compressed gas cylinders Compressed gas cylinders are portable tanks used to store, transport, and dispense gases for use in a broad range of industrial, research, and medical applications. The purpose of a high pressure gas cylinder is to serve as a reliable source of a specific type of gas for a specialized function. A large volume of gas is compressed into a relatively small volume of the cylinder… the result is a versatile high pressure cylinder that can be easily delivered where ever its needed . These cylinders are designed to be easy to handle BUT can create potential health and safety hazards if not properly handled. Description of compressed gas cylinders Common Industrial High Pressure Cylinder ◦ Height 5 ft. ◦ Diameter 9 in. ◦ Wall Thickness ½ in. steel ◦ Weight 140 lbs. ◦ Internal Capacity 1.8 ◦ Design Pressure 2,400 3psi Description of compressed gas cylinders A main fill and shut off valve is secured into the single opening at the top of the cylinder. When the cylinder is put into use, a pressure regulator is attached to reduce and control the pressure of gas flowing from the cylinder. When the cylinder is not in use, the regulator is typically removed and a protective cap can be screwed over the main valve for safe storage. Some cylinders have a built in protective ring in place of the cap. -

E-Cigarette Use in Patients Receiving Home Oxygen Therapy
FOCUSED REVIEW E-cigarette use in patients receiving home oxygen therapy Yves Lacasse MD MSc FRCP1,2, Martin Légaré MD FRCP3, François Maltais MD FRCP1,2 Y Lacasse, M Légaré, F Maltais. E-cigarette use in patients receiving La cigarette électronique chez les patients sous home oxygen therapy. Can Respir J 2015;22(2):83-85. oxygénothérapie à domicile Current smokers who are prescribed home oxygen may not benefit from the therapy. In addition to being an obvious fire hazard, there is some evi- Il se peut que les fumeurs qui se font prescrire une oxygénothérapie à domi- dence that the physiological mechanisms by which home oxygen is cile ne profitent pas de ce traitement. Sans compter que le tabagisme pose believed to operate are inhibited by smoking. Although their effectiveness un risque d’incendie évident, certaines données probantes indiquent qu’il is yet to be demonstrated, electronic cigarettes (e-cigarettes) are often inhibe les mécanismes physiologiques par lesquels l’oxygénothérapie à regarded as an aid to smoking cessation. However, several burn accidents domicile fonctionnerait. Même si son efficacité reste à démontrer, la ciga- in e-cigarette smokers receiving home oxygen therapy have also been rette électronique (vapoteuse) est souvent perçue comme une aide au reported, leading Health Canada to release a warning of fire risk to oxygen sevrage du tabagisme. Cependant, plusieurs incidents de brûlure chez des therapy patients from e-cigarettes. It is the authors’ position that patients vapoteurs sous oxygénothérapie à domicile ont été déclarés, ce qui a incité receiving oxygen should definitely not use e-cigarettes. -

Thermo Valves Corporation
Thermo Valves Corporation Scuba Diving Valves The Leader in High Pressure Technology Date: 05/31/04 Thermo Scuba Products are Sold Through Authorized Distributors Only Thermo PRO Thermo PRO Modular with H Connector Thermo DIN WWW.THERMOVALVES.COM Page 2 Thermo Valves Corporation Table of Contents Introduction 4 Products and Features 5 Scuba Valve Outlets 6 Breathing Air or EAN? 6 Stand Alone Valves 5251 Thermo K 7 5651 Thermo PRO 8 5262 Thermo DIN 9 5282 Thermo DIN 10 Modular Valves 8043 Thermo Modular 11 8063 Thermo Modular 12 8082 Thermo Modular 13 Modular Valve Attachments 9020 Thermo 230 Bar H Connector 14 9040 Thermo 300 Bar DIN H Connector 15 Manifold Center Bars 16 Exploded View Drawings 5251 Series Exploded View 17 5651, 5262 & 5282 Exploded View 18 8043, 8063 & 8082 Exploded View 19 9020 & 9040 Exploded View 20 8002 CTR W VLV Manifold Center Bar Exploded View 21 Parts Index 22 Scuba Valve Parts Warnings 23 Warnings, Terms and Conditions of Sale 24 Page 3 Thermo Valves Corporation The Leader in High Pressure Technology Who We Are Thermo Valves Corporation was founded in 1972 as a manufacturer of compressed gas cylinder valves and adaptors to a wide variety of international standards. Thermo was acquired in 1988 by Hamai Industries Limited who has been manufacturing cyl- inder valves for over 75 years! Thermo now spe- cializes in specialty gas valves, valves for the semi- conductor industry and scuba diving valves. Thermo’s mission is to supply state of the art equip- ment with a focus on safety and innovation SCUBA Diving Valves With over 75 years of manufacturing experi- ence, Thermo Valves full line includes the Thermo K, Thermo PRO, Thermo DIN and Thermo Modu- lar Series of scuba diving valves.