1614154442698 05 Preparedn
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

People, Plagues, and Prices in the Roman World: the Evidence from Egypt
People, Plagues, and Prices in the Roman World: The Evidence from Egypt KYLE HARPER The papyri of Roman Egypt provide some of the most important quantifiable data from a first-millennium economy. This paper builds a new dataset of wheat prices, land prices, rents, and wages over the entire period of Roman control in Egypt. Movements in both nominal and real prices over these centuries suggest periods of intensive and extensive economic growth as well as contraction. Across a timeframe that covers several severe mortality shocks, demographic changes appear to be an important, but by no means the only, force behind changes in factor prices. his article creates and analyzes a time series of wheat and factor Tprices for Egypt from AD 1 to the Muslim conquest, ~AD 641. From the time the territory was annexed by Octavian in 30 BCE until it was permanently taken around AD 641, Egypt was an important part of the Roman Empire. Famously, it supplied grain for the populations of Rome and later Constantinople, but more broadly it was integrated into the culture, society, and economy of the Roman Mediterranean. While every province of the sprawling Roman Empire was distinctive, recent work stresses that Egypt was not peculiar (Bagnall 1993; Rathbone 2007). Neither its Pharaonic legacy, nor the geography of the Nile valley, make it unrepresentative of the Roman world. In one crucial sense, however, Roman Egypt is truly unique: the rich- ness of its surviving documentation. Because of the valley’s arid climate, tens of thousands of papyri, covering the entire spectrum of public and private documents, survive from the Roman period (Bagnall 2009). -

Bibliographic Review on the Historical Memory of Previous
REVISIONES Bibliographic review on the historical memory of previous pandemics in nursing reviews on COVID-19: a secularly documented reality Revisión bibliográfica sobre la memoria histórica de pandemias anteriores en revisiones de enfermería sobre COVID-19: una realidad secularmente documentada Joaquín León Molina1 M. Fuensanta Hellín Gil1 Eva Abad Corpa2 1 Nurse Hospital Clínico Universitario Virgen de la Arrixaca de Murcia; Advanced Nursing Care Group of the Murcian Institute of Biosanitary Research Arrixaca. Murcia. Spain. 2 Associate nurse, Hospital General Universitario Reina Sofía de Murcia; Contracted Professor PhD linked University of Murcia. Advanced Nursing Care Group of the Murcian Institute of Biosanitary Research Arrixaca. Murcia. Spain. https://doi.org/10.6018/eglobal.456511 Received: 17/11/2020 Accepted: 10/01/2021 ABSTRACT: Introduction: Reviews for COVID-19 should reflect historical antecedents from previous pandemics. Objective: We plan to map the content of recent reviews in the nursing area on COVID-19 to see if it refers to health crises due to epidemics and infectious diseases. Methodology: Descriptive narrative review. The Science Web, PubMed and Lilacs were consulted to identify the reviews; The content of the documents was consulted to detect the presence of descriptors and terms related to pandemics prior to the 21st century of humanity, taking into account the inclusion criteria and objectives of the study. Results: Relevant reviews were found only in 11 documents of the 192 identified. Conclusions: There may be reluctance to use documentation published more than a century ago; However, it would be advisable not to lose the historical memory of pandemic crises that humanity has suffered for millennia Key words: Pandemics; Epidemics; History; Ancient History. -

Microbiology E-Journal
From the Principal’s Desk I would like to congratulate the entire team of Department of Microbiology for their wonderful though very strenuous attempt to publish a journal exclusively for the students. Presently the e-version of the journal is going to be released on auspicious day of 5th September, i.e. the Teacher's Day. I hope, later on the print version will be published. In my perception it is a tribute to the entire faculty members by the students because these write ups simply say that how much they assimilate from their teachers in this subject. We all know and still experiencing a very stressful as well as fearful daily life due to the pandemic. We came to know many information regarding this covid-19 virus from many microbiologists not only from India but also from other countries like Canada, USA and many more. The Department of Microbiology, Vijaygarh Jyotish Ray College produced many students who are pursuing their research in India as well as abroad. In response to the call from their teachers they shared their knowledge with us in many webinars organized by the department. In my perception all the students of this department are budding scientist of future. No one knows it may so happen that we come to know that one of our students succeed to be associated with the invention of any life-saving drug or vaccine. Once again, I want thank all students and faculties for initiating this attempt and hope that this will continue to publish. Dr. Rajyasri Neogy, Principal, Vijaygarh Jyotish Ray College Contents Paper Title Page No. -

A Treatise Offered in a Time of Pestilence by St. Cyprian of Carthage
A Treatise Offered in a Time of Pestilence by St. Cyprian of Carthage The Plague of Cyprian was a pandemic that afflicted the Roman Empire from about AD 249 to 262. The plague is thought to have caused widespread manpower shortages for food production and the Roman army, severely weakening the empire during the Crisis of the Third Century. Its modern name commemorates St. Cyprian, Bishop of Carthage, an early Christian writer who witnessed and described the plague. The agent of the plague is highly speculative due to sparse sourcing, but suspects include smallpox, pandemic influenza and viral hemorrhagic fever (filoviruses) like the Ebola virus. In 250 to 262, at the height of the outbreak, 5,000 people a day were said to be dying in Rome. Cyprian's biographer, Pontius of Carthage, wrote of the plague at Carthage: Afterwards there broke out a dreadful plague, and excessive destruction of a hateful disease invaded every house in succession of the trembling populace, carrying off day by day with abrupt attack numberless people, every one from his own house. All were shuddering, fleeing, shunning the contagion, impiously exposing their own friends, as if with the exclusion of the person who was sure to die of the plague, one could exclude death itself also. There lay about the meanwhile, over the whole city, no longer bodies, but the carcasses of many, and, by the contemplation of a lot which in their turn would be theirs, demanded the pity of the passers-by for themselves. No one regarded anything besides his cruel gains. -

Download This PDF File
THE INTERNATIONAL JOURNAL OF BUSINESS & MANAGEMENT ISSN 2321–8916 www.theijbm.com THE INTERNATIONAL JOURNAL OF BUSINESS & MANAGEMENT Effect of Coronavirus Pandemic (Covid 19) on Nigerian Economy: A study of Tummy-Tummy Noodles Producing Firm in Kaduna, Nigeria Nduji Romanus Lecturer, Department of Business Administration, Veritas University, Abuja, Nigeria Oyenuga Michael Lecturer, Department of Marketing, Veritas University, Abuja, Nigeria Idewele Israel Lecturer, Department of Banking and Finance, Veritas University, Abuja, Nigeria Oriaku Christian Lecturer, Department of Business Administration, Veritas University, Abuja, Nigeria Abstract In Africa, the rate at which the incidence of co-vid 19 pandemic is escalating is alarming. Despite efforts made to reduce it through quarantines, lockdown, social/physical distancing and other measures by the Government, yet it is still on the rise especially in Nigeria. The research design adopted for this study is the descriptive design; while structured questionnaire was administered to raise data meant for empirical analysis. Findings from the study showed that Co-vid 19 has a positive and significant effect on Nigerian economy . In addition, Lockdown measure has a significant influence on economic activities of the firms in Nigeria. However, social / physical distancing was discovered to have an insignificant effect on the growth of the firms in Nigeria. Based on these findings, the study recommends that building situational awareness will require sustained investment in infectious disease surveillance, crisis management, and risk communications systems. Investments in these capacities are likely to surge after pandemic or epidemic events and then abate as other priorities emerge. If further recommends that Governments should avoid sweeping and overly broad restrictions on movement and personal liberty, and only move towards mandatory restrictions when scientifically warranted and necessary and when mechanisms for support of those affected can be ensured. -

Download This Issue
COVID ECONOMICS VETTED AND REAL-TIME PAPERS ECONOMIC EPIDEMIOLOGY: ISSUE 48 A REVIEW 10 SEPTEMBER 2020 David McAdams INDIVIDUALISM Bo Bian, Jingjing Li, Ting Xu FORECASTING THE SHOCK and Natasha Z. Foutz Felipe Meza ENTREPRENEUR DEBT AVERSION IS WHO TRUSTED? Mikael Paaso, Vesa Pursiainen Nirosha Elsem Varghese, Iryna and Sami Torstila Sabat, Sebastian Neuman‑Böhme, SUPPLY CHAIN DISRUPTION Jonas Schreyögg, Tom Stargardt, Matthias Meier and Eugenio Pinto Aleksandra Torbica, Job van Exel, PANDEMICS, POVERTY, AND Pedro Pita Barros and Werner Brouwer SOCIAL COHESION ECONOMISTS: FROM VILLAINS Remi Jedwab, Amjad M. Khan, Richard TO HEROES? Damania, Jason Russ and Esha D. Zaver Diane Coyle Covid Economics Vetted and Real-Time Papers Covid Economics, Vetted and Real-Time Papers, from CEPR, brings together formal investigations on the economic issues emanating from the Covid outbreak, based on explicit theory and/or empirical evidence, to improve the knowledge base. Founder: Beatrice Weder di Mauro, President of CEPR Editor: Charles Wyplosz, Graduate Institute Geneva and CEPR Contact: Submissions should be made at https://portal.cepr.org/call-papers- covid-economics. Other queries should be sent to [email protected]. Copyright for the papers appearing in this issue of Covid Economics: Vetted and Real-Time Papers is held by the individual authors. The Centre for Economic Policy Research (CEPR) The Centre for Economic Policy Research (CEPR) is a network of over 1,500 research economists based mostly in European universities. The Centre’s goal is twofold: to promote world-class research, and to get the policy-relevant results into the hands of key decision-makers. CEPR’s guiding principle is ‘Research excellence with policy relevance’. -
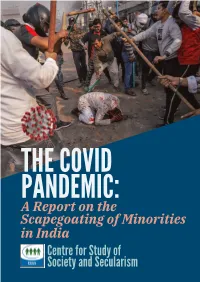
THE COVID PANDEMIC: a Report on the Scapegoating of Minorities in India Centre for Study of Society and Secularism I
THE COVID PANDEMIC: A Report on the Scapegoating of Minorities in India Centre for Study of Society and Secularism i The Covid Pandemic: A Report on the Scapegoating of Minorities in India Centre for Study of Society and Secularism Mumbai ii Published and circulated as a digital copy in April 2021 © Centre for Study of Society and Secularism All rights reserved No part of this book may be reproduced or utilized in any form or by any means, electronic or mechanical, including, printing, photocopying, recording or by any information storage or retrieval system, without the prior written permission of the publisher and without prominently acknowledging the publisher. Centre for Study of Society and Secularism, 603, New Silver Star, Prabhat Colony Road, Santacruz (East), Mumbai, India Tel: +91 9987853173 Email: [email protected] Website: www.csss-isla.com Cover Photo Credits: Danish Siddiqui/Reuters iii Preface Covid -19 pandemic shook the entire world, particularly from the last week of March 2020. The pandemic nearly brought the world to a standstill. Those of us who lived during the pandemic witnessed unknown times. The fear of getting infected of a very contagious disease that could even cause death was writ large on people’s faces. People were confined to their homes. They stepped out only when absolutely necessary, e.g. to buy provisions or to access medical services; or if they were serving in essential services like hospitals, security and police, etc. Economic activities were down to minimum. Means of public transportation were halted, all educational institutions, industries and work establishments were closed. -

Fast-Tracking Vaccines for Epidemic Diseases: an Update from CEPI
Coalition for Epidemic Preparedness Innovations Fast-tracking vaccines for epidemic diseases: an update from CEPI Richard Hatchett, MD CEO, CEPI First traces of a mysterious disease Plague of Cyprian Started in Ethiopia before 250 CE and spread through Egypt, reaching Alexandria by 249 and Rome in 251, causing a pandemic lasting 20 years. At its peak, 5000 a day died in Rome. Its geographic scope was vast; it is attested everywhere we have sources. St. Cyprian, the Bishop of Carthage, left the most detailed account we have, saying he believed the kingdom of God to be at hand. Plague in the 21st Century cnn.com cnn.com • 2348 suspected cases (82 HCW), 202 deaths (November 22) • 55% of cases in Antananarivo and Toamasina • 16 of 22 regions reporting cases • Schools and universities closed, mass gatherings banned; travel advisories • South Africa, Mauritius, Seychelles, Tanzania, La Reunion, Mozambique, Kenya, Ethiopia and Comoros placed on high alert 44 Lassa outbreak in Nigeria • From 1st Jan to 4th March 2018 − Total reported suspected cases 1121 − 353 confirmed cases − 8 probable cases − 86 deaths (78 lab confirmed, 8 probable) − 16 Health care workers − CFR: 23.8% − Cases reported in 18 states LEGEND 0 1- 10 Cases − Ondo, Edo and Ebonyi most affected 11-40 Cases >60 1>suspected cases • Response being led by Nigeria CDC 1 dot = 1 Confirmed/Probable • WHO requested to coordinate proposition for research response • CEPI willing to support where it can, focussing on laying groundwork for future vaccine development including harmonisation -

Intellectual Property in Times of Covid-19
INTELLECTUAL PROPERTY IN TIMES OF COVID-19 Cristiana BUDILEANU* Abstract Since the beginning of year 2020, we are facing a pandemic of a coronavirus disease discovered in 2019 in China and rapidly spread worldwide. This pandemic affected many sectors of economic activities, such as the medical system, tourism, culture, education, work life. The life we knew before the pandemic may never return to us or it would be possible to have a better life after the pandemic is over because since the beginning of times, the human being tried to overcome his condition by creating all sort of things to have an easier and more comfortable life. All such creations were made due to his intellectual activity which later, with the development of the societies, it began to be recognized and protected by laws. Nowadays, the intellectual property is present in all economic sectors and we protect it through patents, designs, copyright, trademarks. Therefore, the intellectual property is nowadays more important than ever in order to try to end the pandemic because only the creative mind of human beings may find a way to eradicate this disease. The purpose of this article is to analyse the consequences of the pandemic into the intellectual property. We would try, among others, to see if the human being remained as creative as before the pandemic or if he taken the opportunity to become even more creative, to invest more in research and development and if the laws protecting the intellectual property would stay in front of the needed progress to overcome this pandemic. -

Pursued by Plague
DE HOOP Pursued by Plague Did the Plague of Cyprian Cause the Romans to Migrate? Anne de Hoop Utrecht University, the Netherlands ABSTRACT Studies of migration in the context of the Roman world have gained immense popularity in recent years. Migration studies are versatile and include multiple different foci, including the movement of minorities, the various types of historical evidence for migration, and the many migration motives. Amongst those motives, contagious diseases are usually neglected by scholars as a push factor. In his most recent work, Kyle Harper takes note of the population decline during the Plague of Cyprian in Alexandria, arguing that not all of these casualties need to be dead of plague; some people may have fled the chaos. Aside from this single critical note, however, Harper does not explore the possibility that migration during the third century CE may have been caused by the Plague of Cyprian. How people spread diseases as they travel is well-researched—in history, as well as in modern times with COVID-19 restricting our mobile way of living. However, migration as a result of pestilence in the Roman world—in other words, people fleeing cities to avoid getting ill and possibly dying as a result thereof—has not been given sufficient scholarly attention. Therefore, this study seeks to analyze the extent to which the Plague of Cyprian acted as a motive for migration in the Roman Empire between 250 and 270 CE. In doing so, it will demonstrate that the Plague of Cyprian likely caused indirect migration based on socio-economic and cultural consequences rather than direct migration as a strategy to avert disease. -

Epidemics and Pandemics, Disinfectants and Antiseptics Photo by Kari Shea on Unsplash More! SIMB Enews Banner Advertisement
SIMB News News Magazine of the Society for Industrial Microbiology and Biotechnology July/August/September 2020 V.69 N.3 • www.simbhq.org Epidemics and Pandemics, Disinfectants and Antiseptics Photo by Kari Shea on Unsplash SIMB eNEWS ADVERTISING OPPORTUNITY Online advertising is an effective way to reach your target audience and should be part of your marketing strategy. Get in front of the customers you want to reach with a SIMB eNews banner advertisement. Contact SIMB to learn more! contents news 80 NEWSWORTHY SIMB News Melanie Mormile | Editor-in-Chief feature Elisabeth Elder | Associate Editor Stephanie Gleason | Associate Editor 84 EPIDEMICS AND PANDEMICS, DISINFECTANTS AND ANTISEPTICS: Kristien Mortelmans | Associate Editor FROM ANTIQUITY UNTIL THE PRESENT CORONAVIRUS SARS- Vanessa Nepomuceno | Associate Editor COV-2 PANDEMIC DESIGN & PRODUCTION members Katherine Devins | Production Manager 78 LETTER FROM SIMB PAST PRESIDENT BOARD OF DIRECTORS 99 SIMB RESOLUTIONS President Steve Decker 101 2020–2021 SIMB BOARD OF DIRECTORS President-elect Noel Fong 107 ETHICS COMMITTEE Past President Jan Westpheling 109 SIMB COMMITTEE LISTING Secretary Elisabeth Elder Treasurer Laura Jarboe book review Directors Katy Kao 102 MICROBIOTA CURRENT RESEARCH AND EMERGING TRENDS Priti Pharkya Tiffany Rau in every issue Rob Donofrio 74 CORPORATE MEMBERS HEADQUARTERS STAFF 75 LETTER FROM THE EDITOR-IN-CHIEF Christine Lowe | Executive Director Jennifer Johnson | Director of Member Services 77 SIMB STRATEGIC PLAN Tina Hockaday | Meeting Coordinator 104 SIMB MEETING CALENDAR Suzannah Citrenbaum | Web Manager Esperanza Montesa | Accountant 111 SIMB CORPORATE MEMBERSHIP APPLICATION EDITORIAL CORRESPONDENCE Melanie R. Mormile Email: [email protected] ADVERTISING For information regarding rates, contact SIMB News On the cover 3929 Old Lee Highway, Suite 92A With masks over their faces, members of Fairfax, VA 22030-2421 the American Red Cross remove a victim P: 703-691-3357 ext 30 F:703-691-7991 of the 1918 Spanish Flu from a house at Email: [email protected] Etzel and Page Avenues, St. -

Distant Times So Close: Excellence ROOTS Describe Human Reactions in Past Societies That Were Organized Quite Differently from Ours
Archaeology is all about how the present came into existence. Thus, it contributes to the social understanding of crises, including present and potential future adversities. Even diseases, such as pandemics in past societies, were and are observed by archaeology. Some examples can be found in this booklet. The scientists of the Kiel Cluster of Distant Times So Close: Excellence ROOTS describe human reactions in past societies that were organized quite differently from ours. This is precisely why it is possible to identify the basic features of human behaviour for the management of crises. Pandemics and From the emergence of agriculture more than 10,000 years ago to the Russian colonisation of Siberia a few hundred years ago, a fundamental pattern is becoming apparent: crises, including those caused by disease, can only be managed by increasing diversity. Acceptance of Crises Reloaded diversity, the introduction of new technologies and socially responsible action have always led to the mastering of crises. It is also clear that values can only be preserved or updated in crises through active involvement. For example, scientists describe that when people are passive, other social groups can easily bind power to themselves, whereas when people actively participate, more democratic structures can develop even in crisis scenarios. This is the message that we take with us from the past: Whether as a forager or as a simple farmer in earliest agricultural societies, in ancient ROOTS Cluster of Excellence Greece or in an early modern society – diversity and social commitment are the components that help us to overcome crises. Learning from the past for the present – that is the task of international archaeology.